Chapter 81 Viral Infections of the Nervous System
Throughout recorded history, viral infections have caused considerable human suffering [Hughes, 1977]. Approximately 100 species of viruses from 13 different families have been associated directly or indirectly with disorders of the central or peripheral nervous system (Box 81-1) [Johnson, 1998]. Although many viral infections have become infrequent or less severe because of immunization programs or antiviral chemotherapy (Figure 81-1), others remain potential threats to the well-being of children throughout the world. This chapter describes virus-induced neurologic disorders, emphasizing pathogenesis, epidemiology, clinical manifestations, treatment, and prevention.
Box 81-1 Selected Viruses Associated with Human Neurologic Disease
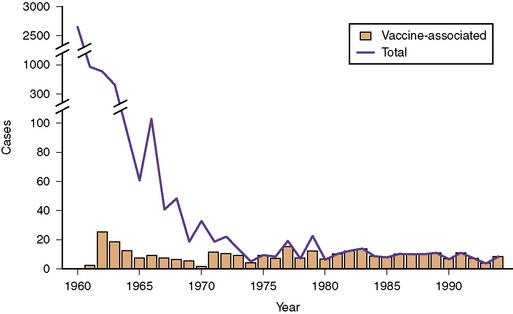
Fig. 81-1 Data for paralytic poliomyelitis in the United States from 1960 to 1994.
(Centers for Disease Control Prevention. Paralytic poliomyelitis – United States, 1980–1994. MMWR Morb Mortal Wkly Rep 1997;46:79).
General Considerations
The pathogenesis of a viral neurologic infection reflects the complex interactions of a viral pathogen and the infected host. Virus-induced neurologic disorders begin with virus entry and replication in the skin, conjunctiva, or mucosal surfaces of the gastrointestinal, respiratory, or genital tracts [Knipe et al., 2007; Johnson, 1998]. Consequently, several host factors, such as the gastric pH, local immune responses, integrity of the skin or mucosal barriers, or enzymes that inactivate viruses, influence whether viral pathogens successfully invade human tissues.
Viruses, among the smallest microorganisms causing human disease, consist of an outer capsid, composed of glycoproteins and lipids, and an inner core, composed of ribonucleic acid (RNA) or deoxyribonucleic acid (DNA) [Knipe et al., 2007]. Virus attachment and penetration of host cells depend on the virus encountering and attaching to receptors located on the surface of host cells. The molecular components of this interaction consist of the viral surface glycoproteins and the host cell surface proteins, such as pre-existing cellular receptors that mediate certain essential cell functions [Knipe et al., 2007; Johnson, 1998]. An example of the virus–host interaction that leads to successful viral replication is the attachment of glycoprotein 120 of the human immunodeficiency virus (HIV) to the CD4 molecule and chemokine receptors of host cells [Knipe et al., 2007].
Viruses enter host cells by endocytosis, release of genomic material, or fusion of the virus envelope with the cell membrane followed by release of viral RNA or DNA. Viruses use host-cell synthetic pathways to uncoat their nucleic acid and to produce virus-encoded nucleic acids and proteins. Replicative strategies vary among viruses [Knipe et al., 2007]. The double-stranded DNA herpesviruses use RNA polymerases in the host-cell nucleus to transcribe viral DNA into viral messenger RNA (mRNA). The RNA of positive-strand RNA viruses serves as the viral mRNA, whereas negative-strand RNA viruses first must be transcribed into an mRNA strand. By contrast, RNA-containing retroviruses, such as HIV, replicate via a DNA intermediary synthesized in the host-cell cytoplasm by a viral-encoded reverse transcriptase [Knipe et al., 2007].
Next, virus-encoded immediate-early and early proteins facilitate the production of additional viral proteins and assembly of mature virus particles, called virions. Viral replication occurs within the nucleus or cytoplasm of the host cell, depending on the viral species, and final assembly of viral particles uses components of existing host-cell structures, such as the nuclear membrane or the Golgi apparatus [Knipe et al., 2007]. Mature virus particles are released from host cells by budding or lysis. Effective replication ultimately releases large quantities of infectious virions into the lymphatics and peripheral circulation of the infected host.
Most viruses reach the central nervous system (CNS) hematogenously and penetrate the blood–brain barrier via the choroid plexus or through the vascular endothelium [Johnson, 1998]. CNS infection depends on the magnitude and duration of viremia, which reflect the efficiency of viral replication at extraneural sites and the ability of the virus to evade host defense mechanisms. CNS invasion, a relatively infrequent event, occurs during infections associated with prolonged viremia or high viral loads.
A few viruses, notably the rabies virus and certain herpesviruses, reach the CNS predominantly through neural routes [Johnson, 1998]. Rabies virus, a negative-strand RNA virus, infects neuromuscular junctions, enters nerve endings, and travels by retrograde axonal transport to the neurons of the spinal cord. The virus then ascends to the brain. Transmission via nerve pathways also mediates the pathogenesis of herpes simplex virus type 1 encephalitis and the mucocutaneous reactivations of herpes simplex virus type 1, herpes simplex virus type 2, and varicella zoster virus.
Viruses induce neurologic signs and symptoms by damaging neural cells directly or by stimulating host-dependent immune responses that perturb neural cell function [Johnson, 1998]. The spectrum and severity of neurologic signs or symptoms depend on several factors, including neurovirulence (the capacity of the virus to cause disease within the nervous system), neurotropism (the propensity of the virus to infect specific cell groups of the CNS), and the nature of the host immune response.
Certain viruses, such as herpes simplex virus type 1, produce lytic infection of neuronal cells and cause hemorrhagic necrosis within the brain, whereas other viruses, such as the La Crosse encephalitis virus, produce minimal cellular damage, despite infection of neural cells. The JC virus, the cause of progressive multifocal leukoencephalopathy, selectively infects oligodendrocytes, causing progressive demyelination [Johnson, 1998]. Some viruses may not infect neural cells directly, but induce immune-mediated processes, such as acute disseminated encephalomyelitis, a condition that accounts for approximately 10–15 percent of acute encephalitis cases in the United States[Johnson, 1996].
Cellular and humoral host immune responses and responses mediated by interferons and inflammatory cytokines (e.g., tumor necrosis factor and the interleukins) have major roles in inhibiting viral infections of the CNS [Zhang et al., 2007a]. The unique roles that specific immune factors have in controlling viral infections in humans continue to constitute an area of intense scientific scrutiny. In animal models, certain Toll and Toll-like receptors, or pattern recognition receptors, participate in the host immune responses to viruses, and in rare instances, human mutations in the genes encoding such receptors have been linked to susceptibility to severe viral infections, such as herpes simplex virus encephalitis [Zhang et al., 2007b]. Immune responses may contribute to the severity of certain diseases, such as herpes simplex virus encephalitis [Conrady et al., 2009], and may provoke certain neurologic disorders, such as Guillain–Barré syndrome, Bell palsy, transverse myelopathy, or acute disseminated encephalomyelitis. The latter disorders can complicate several childhood infections, including relatively benign systemic viral syndromes [Johnson, 1996, 1998].
Clinical Manifestations of Viral Neurologic Disorders
Aseptic Meningitis
Aseptic meningitis, the most frequent CNS disorder associated with viral infections (Box 81-2), produces headache, vomiting, irritability, and neck or back pain. Children appear moderately ill, with photophobia and signs of meningeal irritation, including Kernig’s sign (involuntary spasm of the hamstring muscle provoked by knee extension in a supine patient) or Brudzinski’s sign (flexion of the knees provoked by forced flexion of the neck). In a young infant, signs of meningeal irritation are often absent, and the features of CNS infection, in general, are subtle.
Box 81-2 Viruses Associated with Aspetic Meningitis and Encephalitis in Children
Encephalitis
Numerous viruses (see Box 81-2) can produce encephalitis in childhood. In addition to the headache, vomiting, and systemic features common in aseptic meningitis, children with viral encephalitis have seizures and altered sensorium, ranging from somnolence to coma [Whitley, 1990; Johnson, 1996]. Fever, a common but not invariable feature, ranges from low-grade to 40°C or higher.
Other Neurologic Disorders
Myelitis, Guillain–Barré syndrome, Bell palsy, acute cerebellar ataxia, myositis, and poliomyelitis-like disorders are additional neurologic conditions that can be associated with antecedent childhood viral infections (Box 81-3). Myelitis and Guillain–Barré syndrome frequently begin with vague sensory phenomena, but flaccid weakness and areflexia become the predominant neurologic signs. Marked sensory dysfunction, such as a sensory loss corresponding to a spinal level, indicates spinal cord involvement, whereas facial paralysis favors Guillain–Barré syndrome. Autonomic nervous system dysfunction also can be a major complication of the latter condition, producing life-threatening cardiac dysrhythmias or blood pressure fluctuations.
Cerebellar ataxia (see Chapter 67), as summarized by Connolly and associates, can complicate systemic infections with several different viruses [Connolly et al., 1994]. Varicella-associated ataxia typically begins 5–14 days after the onset of the characteristic rash, although occasional cases can appear during the pre-eruptive phase of infection. Virus-induced ataxia and the associated behavioral disturbance peak in severity at onset or within 1–2 weeks, then improve during the ensuing 4–8 weeks.
Polioviruses (usually type 1) could infect the anterior horn cells of the spinal cord and cause asymmetric paralysis of the extremities (infantile paralysis) and often respiratory failure [Johnson, 1998]. Several other viruses, including West Nile virus, enterovirus 71, and other nonpolio enteroviruses, can produce disorders that can mimic classic poliomyelitis [Chen et al., 2001; Huang et al., 1999; Li et al., 2003].
Intrauterine and Perinatal Viral Infections
Intrauterine infections with certain viruses (and occasional nonviral pathogens) (see Box 81-3) can seriously damage the developing CNS, causing hydrocephalus, cerebral atrophy, intracranial calcifications, schizencephaly, porencephaly, or hydranencephaly [Bale, 2009]. Linked conceptually by the TORCH (toxoplasmosis, rubella, cytomegalovirus, and herpes simplex virus) acronym, these agents produce similar neonatal symptoms and signs consisting of intrauterine growth retardation, hepatosplenomegaly, jaundice, and petechial or purpuric rash [Bale, 2009]. Neurologic features can include microcephaly, chorioretinitis, macrocrania, sensorineural hearing loss, seizures, hypotonia, and focal deficits. Though the TORCH paradigm reminds clinicians that such pathogens produce overlapping clinical manifestations, some agents are associated with relatively unique or characteristic features. Rubella virus, as an example, is the only agent linked convincingly with congenital heart lesions, and varicella zoster virus is the only agent causing a dermatomal pattern of skin scarring known as a cicatrix. Osteopathy suggests congenital syphilis or congenital rubella syndrome, whereas isolated chorioretinitis can occur with congenital toxoplasmosis or lymphocytic choriomeningitis (LCM) virus infection.
Because congenital infections must begin with maternal infection, maternal immune status is a major determinant in the outcome of maternal infection. The fetuses of rubella-immune women, as indicated by the presence of rubella-virus specific IgG in mothers preconceptually, are protected from congenital rubella syndrome [Dudgeon, 1975; CDC, 2005b]; women who are seropositive for cytomegalovirus pre-conceptually are less likely than seronegative women to give birth to infants with congenital cytomegalovirus disease [Fowler et al., 2003]. The timing of maternal infection also affects the outcome of fetal infection and the pathogenesis of the CNS abnormalities associated with congenital infection. Maternal rubella during the initial 8–12 weeks may lead to ophthalmologic abnormalities and congenital heart disease, while infection during the initial 16 weeks can cause sensorineural hearing loss [Dudgeon, 1975; Hanshaw and Dudgeon, 1978]. By contrast, infections after the 20th week, although producing sensorineural hearing loss in some infants, occur silently and rarely cause neurodevelopmental disabilities. Cytomegalovirus-induced defects of neuronal migration, such as lissencephaly, schizencephaly, polymicrogyria, and cortical dysplasia, suggest that infections during critical gestational periods, especially before the 20th week, can be associated with severe neurodevelopmental abnormalities. Early infections with the parasite Toxoplasma gondii also seem to be associated with more severe outcome [Swisher et al., 1994]. The outcome of LCM virus infections is closely linked to the timing of maternal infection, a conclusion supported by studies of LCM virus infection of experimental animals [Bonthius et al., 2007a]. Congenital varicella syndrome, as an additional example of this phenomenon, rarely complicates maternal varicella zoster virus infections before the 5th week or after the 24th week of gestation [Sauerbrei, 2007].
Diagnosing perinatal infections with certain viruses, such as herpes simplex virus type 1 or 2 or parechovirus, remains challenging because the clinical features can be nonspecific during the initial phase of the neurological disease. Early symptoms of serious viral CNS disease in neonates, including herpes encephalitis, may consist only of poor feeding or fussiness, and the physical examination often reveals few signs localizing to the CNS [Bale and Miner, 2005]. Neonatal infections with parechovirus, a picornavirus with at least 14 types, can be associated with encephalitis and CNS white-matter injury [Verboon-Maciolkek et al., 2008a, b]. This disorder should be suspected in infants with fever, rash, and seizures, features that mimic neonatal infection with other enteroviruses.
Slow Viral Infections
Conventional viral pathogens can occasionally produce chronic disorders of the CNS, historically termed slow viral infections. These include subacute sclerosing panencephalitis, postrubella panencephalitis [Townsend et al., 1975], chronic nonpolio enterovirus infection, and progressive multifocal leukoencephalopathy caused by the JC virus (a polyomavirus named for the initials of the patient from whom the virus initially was isolated). Children with these disorders generally lack systemic signs of infection and have clinical signs restricted to the CNS, such as dementia, spasticity, paralysis, vision loss, and seizures. These slow viral disorders typically cause progressive debility and invariably end in death.
Epidemiology of Viral Infections
Worldwide epidemiological data indicate that viruses cause neurological disease (meningitis, encephalitis, and others) in many thousands of persons annually. The rates of encephalitis range from 3 cases per 100,000 persons [Johnson, 1996; Nicolosi et al., 1986] to 33 per 100,000 person-years, with rates highest among children [Koskiniemi et al., 1991, 2001]. Japanese encephalitis, a disease of young children, accounts for several thousand cases of encephalitis annually among unimmunized children in the endemic regions of India and eastern Asia [Dhillon and Raina, 2008].
Until the emergence of West Nile virus in the United States in 1999, the Centers for Disease Control and Prevention (CDC) received reports of 200–500 cases of arboviral encephalitis and many cases of aseptic meningitis every year. As the West Nile viral epidemic spread, numerous cases of West Nile virus infection were reported to the CDC. In 2003 alone, the CDC recorded more than 2800 human cases of neuroinvasive disease caused by West Nile virus [CDC, 2004a]. Recent West Nile virus activity in the United States peaked in 2006, when more than 4500 cases of West Nile virus infection were reported to the CDC; approximately 50 percent have been neuroinvasive infections [CDC, 2009d].
Human rabies cases average between 1 per 100,000 and 1 per million inhabitants annually in Africa and Asia, producing several thousand deaths [Dutta, 1999; Fishbein and Robinson, 1993]. By contrast, the United States has fewer than 5 indigenous cases of human rabies per year because of mandatory vaccination of domestic dogs [Blanton et al., 2009; Plotkin, 2000]. Rabies virus persists in many wild and domestic animal reservoirs, including bats, raccoons, skunks, and foxes in the United States, and wild canines or other mammals in many regions. In 2008, the CDC received reports of nearly 7000 cases of animal rabies, including some among domestic cats, dogs, and cattle [Blanton et al., 2009].
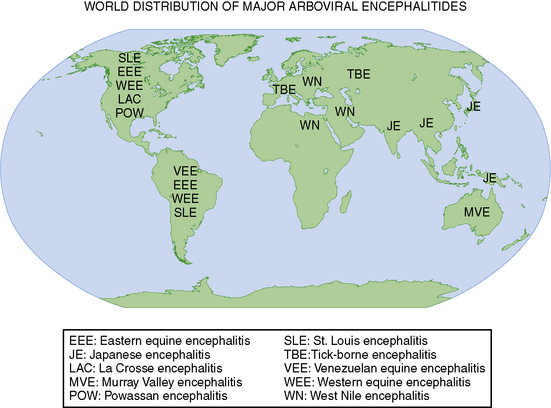
Environmentally derived viral pathogens display relatively uniform epidemiologic characteristics. Mosquitoes, ticks, and biting flies serve as the vectors for most human viral diseases. Human disease occurs when vectors are active, typically in spring, summer, and fall in temperate climates, and often displays distinct epidemiological characteristics that correspond to the habitat of the vector (Figure 81-2). Hiking, camping, and outdoor professions that facilitate vector contact enhance the probability of infections with vector-borne diseases [Miller et al., 2009].
By contrast, human-derived viral pathogens require direct contact with the infected host, either by exposure to aerosols that contain infectious viruses or by contact with tissues, blood, or body fluids from infected individuals. Herpes simplex virus type 1 can be acquired by oral–oral or oral–genital contact, whereas varicella zoster virus (the virus causing chickenpox) usually is transmitted by exposure to aerosolized particles that contain infectious virus. Cytomegalovirus can be acquired by direct contact with infected secretions, transfusion of blood products, or transplantation of organs or tissues from cytomegalovirus-seropositive persons [Bale, 1999].
La Crosse virus encephalitis, a frequently recognized arthropod-borne neurologic infection in the United States, illustrates the epidemiologic characteristics of environmentally derived agents. The disorder affects children who reside in the eastern and midwestern United States (Figure 81-3), a prime habitat for the Aedes triseriatus mosquito, a species that breeds preferentially in water that collects in tree trunks (“tree-holes”) and discarded automobile tires. Cases occur from June to early October, reflecting the seasonal activity of the mosquito vector, and frequently involve males 5–15 years old who enter wooded areas to hunt or play.
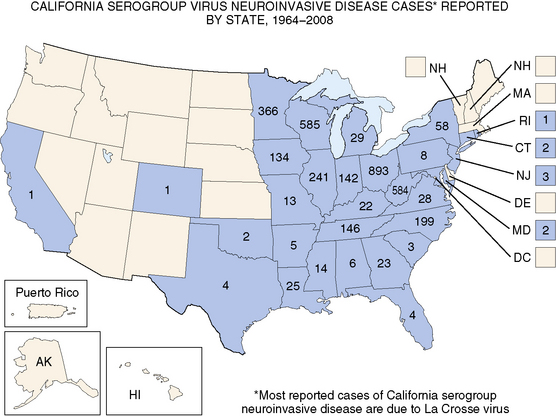
Approximately 70 cases are reported annually.
(Adapted from the Centers for Disease Control and Prevention. Available at: http://www.cdc.gov/ncidod/dvbid/arbor/images/LAC_Map.jpg.)
Members of the herpesvirus family (herpes simplex virus types 1 and 2; cytomegalovirus; Epstein–Barr virus; varicella zoster virus; and human herpesviruses types 6, 7, and 8) display few seasonal or geographic predilections [Whitley et al., 1982]. When Whitley and colleagues reviewed the epidemiology of herpes simplex virus encephalitis, they observed no unique characteristics with regard to race, sex, age, season, or geographic location [Whitley et al., 1982]. Epidemiologic data indicate, however, that herpes simplex virus type 1 is the most common cause of nonepidemic encephalitis in persons older than 50 years. These data reflect the current opinion that most cases of herpes simplex virus encephalitis in older individuals result from reactivated herpes simplex virus infections rather than primary exposures to the virus.
Infection with HIV illustrates well the effects that human behavior and immune competence can have on the spectrum of disease resulting from a neurotropic viral agent. Early in the epidemic of acquired immunodeficiency syndrome (AIDS) in the United States, intravenous drug use, homosexuality, and sexual contact with persons in these groups increased the probability of HIV infection substantially. When CD4+ cell counts decrease to less than 200/mL in persons infected with HIV, opportunistic infections, including infections resulting from other neurotropic viruses, become more likely. The latter conditions include progressive multifocal encephalopathy and cytomegalovirus retinitis and encephalitis [Jacobson, 1997], which are uncommon disorders in immunocompetent persons.
Diagnostic Evaluation
Cerebrospinal Fluid
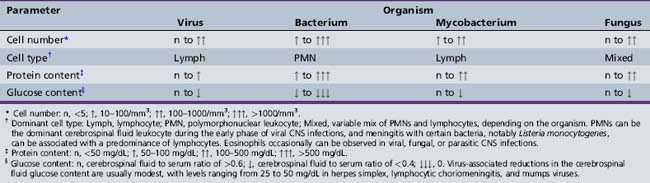
The CSF in viral meningitis or encephalitis typically has a lymphocytic pleocytosis (5–500 cells/mL), mildly elevated protein content (usually 50–200 mg/dL), and normal or slightly depressed glucose content (Table 81-1). The CSF profile can vary, however, depending on the specific viral pathogen and the timing of the lumbar puncture with respect to the onset of neurological disease. Many patients (5–15 percent) with herpes simplex virus encephalitis have an entirely normal initial CSF examination [Whitley et al., 1982], and 10 percent or more of children with California encephalitis have normal cerebrospinal fluid parameters [McJunkin et al., 2001].
Early in the course of many viral CNS infections, the CSF has a preponderance of neutrophils, thus mimicking bacterial disease, but the CSF profile typically shifts to a lymphocytic pleocytosis over time [Feigin and Shackelford, 1973]. Protein elevations in viral meningitis and encephalitis tend to be modest (often <100 mg/dL), and glucose content in viral diseases, although modestly depressed in some cases (30–50 mg/dL), rarely reaches the low levels (e.g., <20 mg/dL) common in acute bacterial meningitis. None the less, some viral infections, such as eastern equine encephalitis, may have CSF parameters that seem more “bacterial” than “viral” [Przelomski et al., 1988].
Electrodiagnostic Studies
The EEG has an important role in evaluating pediatric patients with suspected viral encephalitis. Although the EEG occasionally can be normal in such patients, infants or children with encephalitis usually have abnormal studies, consisting of slowing or epileptiform discharges that can be diffuse or focal. Because herpes simplex virus encephalitis of children or adults frequently produces focal EEG features [Whitley et al., 1982], consisting of slowing, sharp-wave discharges, or periodic lateralizing epileptiform discharges, the EEG has considerable value in suspected cases of herpes simplex virus encephalitis. Although these abnormalities usually localize to the temporal lobes in children, atypical cases of herpes simplex virus encephalitis with other cortical localizations have been confirmed by MRI and polymerase chain reaction (PCR) detection of herpes simplex virus DNA in the CSF [Schlesinger et al., 1995]. Neonates also may have early EEG abnormalities that alert clinicians to the possibility of herpes simplex virus encephalitis [Mikati et al., 1990; Mizrahi and Tharp, 1982].
The EEG has modest sensitivity and specificity in several other forms of encephalitis. Between 40 and 50 percent of patients with La Crosse encephalitis or eastern equine encephalitis have lateralizing EEG abnormalities that suggest focal brain disease [Hilty et al., 1972; Przelomski et al., 1988]. In many cases, the EEG shows only diffuse slowing of variable severity. In contrast to the abnormalities observed in virus encephalitis, the EEG is usually normal in cases of aseptic meningitis [Pollak et al., 2001].
Neuroimaging
Computed tomography (CT) and MRI have major roles in evaluating infants and children with CNS viral infections [Bale, 1999; Baskin and Hedlund, 2007; Kimberlin, 2004]. Depending on their clinical status, patients with suspected viral encephalitis should undergo a neuroimaging study early in the course of their illnesses. Although large mass lesions, such as tumors or brain abscess, can be detected reliably by CT, especially when obtained with contrast enhancement, MRI has sensitivity that exceeds CT, especially in patients with herpes simplex encephalitis [Baskin and Hedlund, 2007; Domingues et al., 1998; Schroth et al., 1987]. Because of the sensitivity of MRI for the early changes of herpes simplex encephalitis, MRI is the preferred imaging modality in children with suspected viral encephalitis.
After the neonatal period, MRI in herpes simplex encephalitis usually shows T2 prolongation in the medial temporal lobe, orbitofrontal region, or cingulate gyrus, and cortical enhancement in these regions when the paramagnetic agent, gadolinium, is administered intravenously [Baskin and Hedlund, 2007]. Atypical features can be observed, however, including parieto-occipital localization of T2 prolongation and abnormalities of diffusion-weighted images [Leonard et al., 2000; Maschke et al., 2004].
Neuroimaging frequently reveals diffuse or focal brain edema in infants with neonatal herpes simplex encephalitis, a disease that differs pathogenetically from herpes simplex encephalitis of older children in most instances [Bale and Miner, 2005; Kimberlin, 2004]. Neonatal herpes simplex encephalitis usually results from hematogenous transmission of the virus to brain, whereas herpes simplex encephalitis in older individuals usually reflects reactivation and neural transmission of herpes simplex virus.
Several other viral-induced CNS disorders have relatively pathognomonic neuroimaging features. MRI can detect focal abnormalities of the basal ganglia in children with Japanese or Epstein–Barr virus encephalitis [Maschke et al., 2004], and patients with neuroinvasive West Nile virus infections can have imaging abnormalities of the substantia nigra, brainstem, or spinal cord [Maschke et al., 2004]. In acute disseminated encephalomyelitis (ADEM), a condition that mimics virus encephalitis, MRI reveals multifocal areas of T2 prolongation involving the white matter of the cerebrum, cerebellum, and brainstem. The sensitivity of MRI exceeds that of CT in ADEM [Rust, 2000] a condition that often responds to corticosteroid therapy. MRI in other forms of viral encephalitis can be normal; reveal diffuse, nonspecific changes of edema or inflammation; or have focal abnormalities that mimic herpes simplex virus encephalitis [Baskin and Hedlund, 2007]. Children with aseptic meningitis typically have normal brain parenchyma when studied by CT or MRI.
Infants with suspected intrauterine viral infections should be evaluated by CT initially because small intracranial calcifications, a common feature of intrauterine infection, can be detected better by this imaging modality than by MRI or ultrasonography [Bale, 2009; Baskin and Hedlund, 2007]. In addition, most hospitals can perform CT without sedating young infants. These infants may benefit from a subsequent MRI study, however, to identify coexisting brain abnormalities, such as lissencephaly-pachygyria, periventricular leukomalacia, or cortical dysplasia, that are missed or poorly characterized by CT. CT or MRI may reveal hydrocephalus, hydranencephaly, or cystic encephalomalacia in infants with intrauterine or perinatal viral infections.
Microbiologic Evaluation
The diagnostic techniques available to the clinician include serology, cell culture, immunohistology, and molecular methods, such as PCR (Table 81-2). Serology provides indirect evidence of infection because it depends on the host to mount an antibody response specific to the etiologic agent. Certain infections, such as those resulting from Epstein–Barr, lymphocytic choriomeningitis, and West Nile viruses, usually are identified by serologic studies, and others, such as La Crosse, eastern and western equine, St. Louis, and Japanese encephalitis viruses, can be diagnosed rapidly by immunoglobulin M (IgM) antibody capture methods.
Table 81-2 Preferred Diagnostic Methods for Selected Viral Infections of the Nervous System
| Agent | Neonatal Infection | Non-Neonatal Infection |
|---|---|---|
| Herpes simplex virus | Cultures of CSF; swabs of nasopharynx, conjunctivae, and skin lesions; serum and CSF PCR | CSF PCR |
| Cytomegalovirus | Cultures of urine and saliva | Cultures of urine, saliva; serum and CSF PCR |
| Varicella zoster virus | Difficult by any method | Culture of skin vesicle fluid, immunohistology, CSF PCR |
| Epstein–Barr virus | – | Acute and convalescent sera; CSF PCR |
| Human herpesviruses 6, 7, 8 | – | CSF PCR |
| Enteroviruses | Serum and CSF PCRs | Serum and CSF PCRs |
| Arthropod-borne encephalitis viruses | Virus-specific IgM | Virus-specific CSF or serum IgM; CSF PCR; acute and convalescent sera |
| Rabies virus | – | Virus culture, serum IgG after day 15; immunohistology of skin biopsy; CSF PCR |
| Lymphocytic choriomeningitis virus | Serologic studies of infant and mother | Acute and convalescent sera; CSF PCR |
| Human immunodeficiency virus 1 | Plasma PCR | Serologic studies; Western blot; plasma and CSF PCR |
CSF, cerebrospinal fluid; PCR, polymerase chain reaction.
Cell culture provides direct evidence of infection by detecting viral pathogens in CSF, blood, or other body fluids, although cell culture is gradually been supplanted by molecular methods of detecting viruses, such as PCR. Viruses that lend themselves to detection by cell culture include the herpesviruses (especially cytomegalovirus and certain herpes simplex virus infections), enteroviruses, adenoviruses (a rare cause of CNS infection), HIV, and rabies virus. Cultures of CSF or mucosal surfaces often yield virus in neonatal herpes simplex virus infections [Kimberlin, 2004], but infectious virus can be detected in the CSF in less than 5 percent of herpes simplex virus encephalitis cases in children and adolescents. Consequently, PCR has become the gold standard for evaluating infants and children with suspected herpes simplex virus encephalitis or meningitis, especially as laboratories employ molecular detection methods with high sensitivity and specificity [Mitchell et al., 1997; Whitley and Gnann, 2002]. Specific immunohistologic detection of herpes simplex virus and varicella zoster virus has supplanted the nonspecific and insensitive Tzanck preparation.
PCR allows diagnosis of infections with the herpes simplex viruses, cytomegalovirus, enteroviruses, JC virus, human herpesvirus 6, rabies virus, varicella zoster virus, and HIV-1, and can also be used to detect nonviral agents that cause intrauterine infection, encephalitis, or aseptic meningitis [Huttunen et al., 2009; Read et al., 1997]. PCR detects herpes simplex virus DNA in the CSF in most cases of herpes simplex virus encephalitis or meningitis in infants, children, or adolescents [Domingues et al., 1998; Kimberlin et al., 1996; Lakeman and Whitley, 1995; Mitchell et al., 1997; Read et al., 1997]. The specificity of PCR in herpes simplex virus encephalitis approaches 100 percent, whereas the sensitivity ranges from 75 percent in neonates to 95 percent or greater in children or adolescents [Johnson, 1996; Kimberlin, 2004]. Although PCR has an analytical sensitivity and specificity (i.e., the ability to detect viral DNA consistently in “spiked” CSF samples) that approaches 100 percent for many viruses, the clinical sensitivity of CSF PCR is unknown for many viral CNS infections, given the absence of appropriate gold standards against which to compare PCR. Consequently, clinicians must use sound clinical judgment, especially when making decisions regarding the initiation or discontinuation of antiviral therapy.
Overview of Treatment
Therapy for CNS viral infections must be tailored to illness severity, the suspected agent, and the availability of specific antiviral medications. Numerous nonviral conditions can produce clinical signs that mimic signs of viral CNS infection. Children with life-threatening viral diseases, such as herpes simplex virus encephalitis, require hospitalization in a skilled nursing unit, such as a pediatric intensive care unit, which can provide frequent assessment of the child’s responsiveness and anticipatory monitoring for seizures and increased intracranial pressure. Outcome of viral CNS infections varies according to the viral pathogen, the specific disorder, the child’s age, and availability of specific antiviral therapy (Table 81-3).
Table 81-3 Outcome of Selected Viral Central Nervous System Disorders
| Disorder | Mortality (%) | Morbidity (%) |
|---|---|---|
| HERPES SIMPLEX VIRUS* | ||
| Congenital infection | 10 | 100 |
| Neonatal encephalitis | <10 | 40 |
| Non-neonatal encephalitis | <10 | 40 |
| CYTOMEGALOVIRUS | ||
| Symptomatic congenital | 5 | 95 |
| Encephalitis-AIDS | >50 | High |
| ENTEROVIRUS | ||
| Aseptic meningitis | Negligible | Negligible |
| Encephalitis | Negligible | ≤10 |
| TOGAVIRUSES | ||
| Eastern equine encephalitis | 40 | 50 |
| Western equine encephalitis | 10 | 15 |
| RUBELLA VIRUS | ||
| Symptomatic congenital | 5 | 90 |
| FLAVIVIRUSES | ||
| Japanese encephalitis | 40 | 50 |
| St. Louis encephalitis | 10 | 20 |
| West Nile virus | 5 | 33 |
| BUNYAVIRUSES | ||
| La Crosse encephalitis | Negligible | ≤15 |
| PARAMYXOVIRUSES | ||
| Measles encephalomyelitis | 20 | 50 |
| Subacute measles encephalitis | 80 | 100 |
| SSPE | 100 | – |
| Rabies virus† | Nearly 100 | – |
| LYMPHOCYTIC CHORIOMENINGITIS VIRUS | ||
| Symptomatic congenital | 40 | 80 |
| Aseptic meningitis | Negligible | Negligible |
| RETROVIRUSES‡ | ||
| HTLV-I | Variable | 100 |
| HIV | Variable | Variable |
AIDS, acquired immunodeficiency syndrome; HIV, human immunodeficiency virus; HTLV-I, human T-cell lymphotropic virus type I; SSPE, subacute sclerosing panencephalitis.
* Assumes appropriate management with acyclovir. Rates for untreated cases are higher.
† Survival reported in <10 persons (total) with symptomatic rabies [American Academy of Pediatrics, 2009].
‡ Outcomes related to current management.
Supportive Care
Children or adolescents with optic neuritis, myelitis, inflammatory vasculitis, or acute disseminated encephalomyelitis often benefit from corticosteroid therapy. The successful treatment of optic neuritis in adults serves as a model for the pharmacologic treatment of several inflammatory/immune-mediated conditions in childhood or adolescence. Children can receive 2 weeks of daily corticosteroids, beginning with a short course of high-dose methylprednisolone intravenously (e.g., 15 mg/kg/day divided equally every 6 hours for 3–5 days), followed by prednisone orally (e.g., 1–2 mg/kg/day for 7–10 days). Some authorities have utilized a short (3–5 days only), high-dose corticosteroid regimen, consisting of 15–20 mg/kg/day of methylprednisolone intravenously in equally divided doses every 6 hours [Tenembaum et al., 2007]. Children with postviral Guillain–Barré syndrome may improve after intravenous immunoglobulin [Abd-Allah et al., 1997; Jansen et al., 1992].
Specific Viral Infections
Herpesviruses
Herpes Simplex Virus
Clinical features
Most humans acquire herpes simplex virus type 1 by oral transmission during childhood [Chayavichitsilp et al., 2009; Corey and Spear, 1986]. Primary herpes simplex virus infections are frequently asymptomatic, although some children experience vesicular pharyngitis or gingivostomatitis, a condition associated with fever, diminished oral intake, drooling, and herpetic lesions of the face and mouth. By contrast, herpes simplex virus type 2, usually acquired by sexual contact, causes genital lesions in young adults [Corey and Wald, 2009]. In children, herpes simplex virus-induced neurologic infections can be due to primary or reactivated infections, whereas most herpes simplex virus-induced disease after age 30 years, whether due to herpes simplex virus type 1 or type 2, reflects reactivated infection.
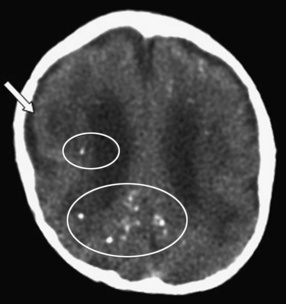
Neonatal herpes simplex virus infection, most often due to herpes simplex virus type 2, can be categorized as (1) skin, eyes, and mouth disease; (2) disseminated disease; or (3) encephalitis, affecting approximately 43 percent, 23 percent, and 34 percent of herpes simplex virus-infected infants, respectively [Corey and Wald, 2009; Kimberlin, 2004; Malm, 2009; Whitley et al., 1988]. Neonatal herpes simplex virus disease usually begins with nonspecific clinical features (poor oral intake, behavioral change, or fever), as early as the first day of life, but more often in the second or third weeks [Kimberlin, 2004; Koskiniemi et al., 1989]. Neonatal herpes simplex encephalitis produces focal or generalized seizures, paralysis, apnea, and lethargy or coma [Bale and Miner, 2005; Kimberlin, 2004; Koskiniemi et al., 1989; Malm, 2009; Whitley et al., 1988]. Herpes simplex encephalitis in neonates can be accompanied by pneumonitis, hepatitis, or disseminated intravascular coagulopathy, but one-third of infants with neonatal herpes simplex virus encephalitis have disease restricted to the CNS [Koskiniemi et al., 1989]. Approximately two-thirds of infants have a vesicular rash. The infection can be rapidly fatal, with multiorgan system failure, or be associated with apnea, impaired bulbar function, and intractable seizures. Approximately 5 percent of infants infected with herpes simplex virus acquire the virus in utero and display a relatively characteristic pattern of physical signs consisting of microcephaly, cataracts, intracranial calcifications (Figure 81-4), intrauterine growth retardation, and vesicular rash or other skin lesions [Grose, 1994; Hutto et al., 1987; Koch et al., 2009].
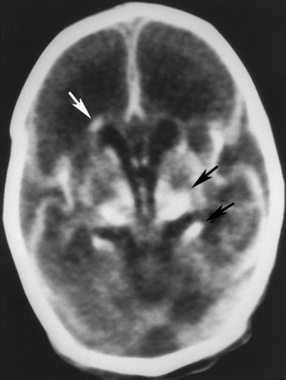
Fig. 81-4 Unenhanced computed tomography scan of an infant with congenital herpes simplex virus infection.
(From Souza IE, Bale JF. The diagnosis of congenital infections: Contemporary strategies. J Child Neurol 1995;10:271.)
In older children or adolescents, herpes simplex encephalitis, typically herpes simplex virus type 1, begins nonspecifically with headache, fever, malaise, vomiting, and behavioral changes [Hsieh et al., 2007]. Focal neurologic signs, such as hemiparesis, dysphasia, or visual field defects, appear subsequently in most patients. Seizures affect approximately 40 percent of patients with biopsy-confirmed herpes simplex encephalitis; seizures can be generalized but are more often partial [Whitley et al., 1982]. Focal abnormalities reflect the predilection of herpes simplex virus for infecting frontotemporal brain regions, but other areas of the brain can be affected [Leonard et al., 2000]. The clinical course of herpes simplex encephalitis can be rapidly progressive, with coma and intractable seizures, or indolent, with memory loss and behavioral disturbances.
In addition to causing necrotizing encephalitis, herpes simplex virus has been linked to Bell’s palsy by detecting herpes simplex virus type 1 DNA in facial nerve tissues or in the geniculate ganglia [Burgess et al., 1994]. Herpes simplex virus also has been associated with primary or recurrent aseptic meningitis (Mollaret meningitis) [Bergström et al., 1990]. Common clinical manifestations of herpes simplex virus-associated aseptic meningitis include fever, photophobia, vomiting, and headache, but children with herpes simplex virus-induced meningitis usually lack herpetic lesions of the skin or mucosal surfaces [Rathore et al., 1996]. Although children with herpes simplex virus type 1 meningitis can recover uneventfully without therapy [Rathore et al., 1996], acyclovir therapy should be administered. Herpes simplex virus infection also has been associated with a necrotizing myelopathy in childhood, although it more commonly occurs in adults with reactivated herpes simplex virus infections [Ellstein-Shturman et al., 1976].
Diagnosis
Neonates with herpes simplex virus infections may have elevated serum transaminases, direct hyperbilirubinemia, and laboratory features of disseminated intravascular coagulopathy [Kimberlin, 2004; Koskiniemi et al., 1989]. The CSF in neonatal herpes simplex encephalitis reveals a lymphocytic pleocytosis and elevations of the protein content; the CSF glucose can be normal or mildly low. MRI and CT usually reveal diffuse edema during the acute stage, and later exhibit atrophy, parenchymal calcification, or cystic encephalomalacia [Tien et al., 1993; Vossough et al., 2008]. MRI can reveal a “watershed” distribution of abnormalities [Vossough et al., 2008]. EEGs are frequently abnormal in infants with encephalitis, revealing slow background activity and paroxysmal discharges that occasionally are periodic [Mikati et al., 1990].
Herpes simplex virus infection of the newborn can be confirmed by isolating virus from CSF, skin lesions, or mucosal surfaces of the eye, oropharynx, or rectum, or by detecting herpes simplex virus DNA in CSF or serum by using PCR. In a retrospective analysis of CSF samples accumulated by the National Institutes of Health–Collaborative Antiviral Study Group, herpes simplex virus DNA was detected by PCR in the CSF of 93 percent of the infants with disseminated infection, 76 percent of infants with encephalitis, and only 24 percent of infants with skin-eyes-mouth disease [Kimberlin et al., 1996].
Because older infants, children, and adolescents with herpes simplex virus encephalitis rarely have systemic signs of infection, neurodiagnostic and CSF PCR studies have major roles in establishing the diagnosis [Mitchell et al., 1997; Whitley and Lakeman, 1995; Whitley et al., 1982]. MRI may indicate unilateral or bilateral abnormalities consisting of T2 prolongation in the temporal lobe or insula, and enhancement of the insula, temporal cortex, and cingulate gyrus on T1-weighted, gadolinium-enhanced images [Schroth et al., 1987; Tien et al., 1993]. Focal abnormalities involving other cortical regions, including parietal or occipital lobes, can be observed, however, in atypical cases of herpes simplex encephalitis [Schlesinger et al., 1995]. EEGs, abnormal in approximately 80 percent or more of patients, reveal focal or diffuse slowing and epileptiform discharges that can be periodic and lateralizing.
In National Institutes of Health–Collaborative Antiviral Study Group studies of adults, herpes simplex virus DNA was detected in the CSF of 98 percent of patients with biopsy-proven herpes simplex virus encephalitis, whereas only 6 percent of biopsy-negative patients had herpes simplex virus DNA in CSF [Lakeman and Whitley, 1995]. These results, as well as results from other laboratories, indicate that the sensitivity and specificity of PCR in herpes simplex virus encephalitis of children or adolescents exceed 90–95 percent [Mitchell et al., 1997; Read et al., 1997]. None the less, clinicians must use caution when interpreting the results of CSF PCR studies for herpes simplex virus, especially when negative. Full courses of acyclovir may be necessary when clinical features, especially MRI findings, are compatible with herpes simplex virus encephalitis but CSF PCR studies are negative.
Treatment and outcome
Infants with herpes simplex virus infections should receive acyclovir, 20 mg/kg every 8 hours for 14 days in skin and mucous membrane infections, and 20 mg/kg every 8 hours for 21 days in disseminated infections or encephalitis [Bale and Miner, 2005; James et al., 2009; Kimberlin et al., 2001b; Whitley et al., 1986, 1991a, b]. CSF PCR should be obtained at 21 days in the latter infants, and if the PCR remains positive for herpes simplex virus DNA, acyclovir should be continued for another 7 days. Children with herpes simplex virus encephalitis should be treated with 20 mg/kg every 8 hours for 21 days, and adolescents can receive 1500 mg/m2 for 21 days. Potential side effects include tremulousness, hematuria, and reversible nephropathy. The drug is very well tolerated, although complete blood counts and serum creatinine levels should be monitored during prolonged courses of acyclovir. Although favorable outcome after neonatal or childhood herpes simplex virus infections correlates with the early initiation of acyclovir, sequelae are common, even after appropriate medical management.
All acyclovir-treated infants with skin, eye, and mouth infections with herpes simplex virus survive, and nearly all such infants have no long-term sequelae of their infections, other than the propensity to have recurrent herpetic skin lesions [Kimberlin et al., 2001a]. As many as 30 percent of the infants with disseminated neonatal herpes simplex virus infections die, however, despite appropriate therapy, and 20–30 percent of the survivors have sequelae ranging from mild (speech delay or mild motor delay) to severe (spastic quadriparesis or severe developmental delay). Neonates with encephalitis have less than 10 percent mortality, but approximately 40 percent of the surviving infants have severe sequelae, despite acyclovir therapy [Kimberlin et al., 2001b]. Infants who survive herpes simplex virus encephalitis can have permanent pseudobulbar palsy with mutism and feeding difficulties (Figure 81-5). Infants with congenital herpes simplex virus infections generally have poor prognoses [Grose, 1994; Hutto et al., 1987]. Potential sequelae of herpes simplex virus encephalitis in children and adolescents consist of partial and generalized seizure disorders, developmental delay, cerebral palsy, language and memory dysfunction, behavioral abnormalities, and motor deficits [Hsieh et al., 2007; Kimberlin et al., 2001a, b; Whitley et al., 1991b].

Fig. 81-5 Unenhanced computed tomography scan of a young child who survived herpes simplex virus encephalitis.
Relapse or persistence of symptoms in herpes simplex virus encephalitis, associated with fever, lethargy, headache, and movement disorder, can develop despite appropriate initial management and acyclovir therapy [Barthez-Carpentier et al., 1995; Gutman et al., 1986]. Such children require repeat CSF PCR studies for herpes simplex virus, MRI, repeat treatment with acyclovir, and corticosteroid therapy if imaging results suggest acute disseminated encephalitis. Because of the substantial morbidity associated with neonatal and childhood herpes simplex virus encephalitis, on-going studies are evaluating the role for prolonged suppressive therapy with acyclovir in neonates with herpes simplex virus infections [James et al., 2009; Kimberlin, 2004].
Cytomegalovirus
Clinical features
Infection with cytomegalovirus, a ubiquitous member of the herpesvirus family, has been associated with several childhood neurologic conditions, including intrauterine infection; infantile spasms; Guillain–Barré syndrome; and encephalitis, myelitis, or retinitis in immunosuppressed hosts, especially persons with AIDS [Bale, 1999; McCutchan, 1995]. Approximately 1 percent of infants excrete cytomegalovirus at birth, and the virus is acquired steadily thereafter throughout life. Young children who attend daycare centers, adults who have contact with young children, and persons with multiple sexual partners acquire cytomegalovirus at annual rates of 8–25 percent or more, considerably higher than the background infection rates of 2–5 percent per year [Demmler, 1991; Murph and Bale, 1988]. Children acquire cytomegalovirus by contact with persons who shed cytomegalovirus in urine or saliva, and by transfusion of blood products or transplantation of organs from cytomegalovirus-seropositive donors [Demmler, 1991].
At birth, 0.4–2.5 percent of newborns shed cytomegalovirus in urine or saliva, indicating congenital infection [Demmler, 1991; Malm and Engman, 2007]. Approximately 90 percent of cytomegalovirus-infected infants are asymptomatic at birth. Although sensorineural hearing loss develops subsequently in 7–10 percent of these infants [Fowler et al., 1997], they rarely have other CNS complications. The remaining 10 percent of infants with congenital cytomegalovirus infection have hepatomegaly, splenomegaly, jaundice, petechial or purpuric skin rash, intrauterine growth retardation, microcephaly, or chorioretinitis [Boppana et al., 1997; Demmler, 1991; Malm and Engman, 2007].
Cytomegalovirus has been linked to infantile spasms, usually in infants with intrauterine infection. Immunocompetent children or adolescents with cytomegalovirus infections can have a mild, self-limited encephalitis [Studahl et al., 1992] or Guillain–Barré syndrome. The latter disorder begins with paresthesias and causes weakness that usually begins in the lower extremities. Affected children can have bilateral facial paresis, respiratory failure, or cardiac dysrhythmias. Symptoms of a cytomegalovirus-induced mononucleosis syndrome [Horwitz et al., 1986] – malaise, low-grade fever, or headache – may precede or accompany the onset of Guillain–Barré syndrome.
Patients immunocompromised by AIDS, malignancy, transplantation, or immunosuppressive therapy are at risk for cytomegalovirus-induced retinitis, encephalitis, myelopathy, and Guillain–Barré syndrome-like disorders. Given the demographics of AIDS, most reported patients with cytomegalovirus retinitis, encephalitis, or myelitis are adults between the ages of 20 and 50 years [Holland et al., 1994; Jacobson, 1997]. Immunocompromised infants or children, especially those with HIV infection, are at risk for retinitis, colitis, pneumonitis, and CNS complications of cytomegalovirus infections [Darin et al., 1994].
Diagnosis
The diagnosis of intrauterine cytomegalovirus infection can be established by assaying urine or saliva using the shell vial cell culture method. PCR can detect cytomegalovirus DNA in urine, saliva, or serum, but the shell vial assay is sensitive and cost-effective [Demmler et al., 1988]. Cytomegalovirus DNA can also be detected by PCR analysis of dried blood spots obtained from newborn infants, but the sensitivity of this detection method does not exceed that of urine or saliva assay [Atkinson et al., 2009]. Common, nonspecific laboratory features of congenital cytomegalovirus infections include thrombocytopenia, direct hyperbilirubinemia, and elevated serum transaminases [Demmler, 1991].
CT scans reveal intracranial calcifications (Figure 81-6) in 25–50 percent of symptomatic infants [Boppana et al., 1997; Pass et al., 1980]. Hydranencephaly, atrophy, lissencephaly, schizencephaly, and cerebellar hypoplasia also can accompany congenital cytomegalovirus infections [de Vries et al., 2004; Iannetti et al., 1998], and white-matter abnormalities are commonly seen when congenitally infected infants undergo brain MRI [van der Knapp et al., 2004]. Approximately 50 percent of symptomatic infants have abnormal auditory-evoked responses, indicating sensorineural hearing loss [Boppana et al., 1997; Pass et al., 1980; Rivera et al., 2002].
Infection in older infants or children can be established by isolating cytomegalovirus from urine, saliva, or circulating leukocytes; by detecting cytomegalovirus-specific antigens in circulating leukocytes; or by detecting cytomegalovirus DNA in CSF, serum, or urine [Clifford et al., 1993]. Some patients with cytomegalovirus infection have elevated serum transaminases or hematologic abnormalities, such as leukopenia, anemia, or thrombocytopenia. CT or MRI may reveal abnormalities of the brain or spinal cord consisting of demyelination or inflammation involving cortical or periventricular regions [Miller et al., 1997].
Treatment and outcome
Infants who survive symptomatic intrauterine cytomegalovirus infections often have permanent neurodevelopmental sequelae consisting of mental retardation, seizure disorders, behavioral disturbances, visual impairment, and sensorineural hearing loss [Boppana et al., 1997; Malm and Engman, 2007; Pass et al., 1980]. Because hearing loss can be progressive, even after silent, intrauterine cytomegalovirus infection, infants with known congenital cytomegalovirus infection require serial audiometry at frequent intervals during infancy and childhood [Fowler et al., 1997]. Infants with abnormal CT scans are more likely to have adverse neurodevelopmental outcomes [Boppana et al., 1997; Noyola et al., 2001].
Although intrauterine cytomegalovirus infection cannot currently be prevented by vaccination, recent studies suggest that a vaccine based on glycoprotein B, a major immunogenic protein of human cytomegalovirus, can reduce the risk of maternal infection [Pass et al., 2009]. Ganciclovir, an antiviral drug closely related to acyclovir, provides some benefit to infants with congenital cytomegalovirus disease. A controlled trial of ganciclovir indicated that prolonged courses of ganciclovir, 10–12 mg/kg/day for 42 days, can improve hearing outcomes [Kimberlin et al., 2003]. Based on these encouraging data, ganciclovir should be considered for infants with congenital cytomegalovirus disease, given the high risk of sensorineural hearing loss in such infants. Bone marrow suppression and line infections can be potential adverse effects of prolonged intravenous therapy. Studies of oral therapy, using the prodrug valganciclovir, are on-going.
Immunocompromised children with invasive cytomegalovirus disease, especially retinitis, should receive ganciclovir, beginning with 5 mg/kg intravenously twice daily for approximately 14 days. Long-term maintenance therapy, using 5–10 mg/kg/day, is required in persons with cytomegalovirus retinitis and HIV infection [Jacobson, 1997]. Complete blood counts and renal function should be monitored frequently. Outcome of acquired cytomegalovirus infection depends greatly on the immunocompetence of the infected host. Patients who are immunosuppressed by AIDS or transplantation have increased risks of death during systemic or CNS cytomegalovirus infections. By contrast, most children with normal immune systems generally recover from acquired cytomegalovirus infections without lasting sequelae. The prognosis of cytomegalovirus-induced Guillain–Barré syndrome in immunocompetent children is comparable with that of Guillain–Barré syndrome resulting from other causes.
Varicella Zoster Virus
Clinical features
Varicella zoster virus, the cause of chickenpox (varicella) and shingles (zoster), has been associated with several neurologic conditions in children, including acute ataxia, myelitis, stroke, postherpetic neuralgia, Bell’s palsy, Ramsay Hunt syndrome, aseptic meningitis, encephalitis, congenital varicella syndrome, and Reye’s syndrome [Gilden, 2004; Weller, 1983]. These conditions can affect immunocompetent or immunocompromised hosts, although immunosuppressed hosts, such as patients with HIV/AIDS or hematologic malignancies, have greater risks of severe, invasive varicella zoster virus infections. Certain conditions, such as varicella-induced ataxia or Reye’s syndrome (rarely seen, currently), occur almost exclusively in immunocompetent children.
Chickenpox, the illness associated with primary varicella zoster virus infection, peaks among children between the ages of 5 and 9 years and occurs more often in winter months. The virus spreads by aerosolization and respiratory transmission; children are contagious during the interval encompassing 2 days before and 5 days after the onset of the chickenpox rash. The incubation period averages 14 days. After primary infection, the virus enters a latent stage in sensory ganglia and can reactivate, causing zoster or shingles [Gilden, 2004]. Consequently, zoster more commonly affects the elderly or persons with immunocompromising conditions. Zoster can occur, however, in otherwise healthy children or adolescents [Guess et al., 1985]. Less than 0.1 percent of otherwise healthy children with chickenpox experience neurologic complications. Acute cerebellar ataxia, the most common complication, begins approximately 10 days after the onset of the rash, although ataxia preceding the rash or after varicella vaccination has been reported [Sunaga et al., 1995]. Truncal ataxia, dysmetria, vomiting, and irritability are common clinical features. The ataxia, often maximum at onset, frequently inhibits independent ambulation, and nystagmus can be present [Connolly et al., 1994]. The precise pathogenesis of ataxia after varicella, although presumed to be immune-mediated, has not been fully elucidated.
Other varicella zoster virus-related neurologic complications are uncommon. Reye’s syndrome, a now-rare disorder characterized by pernicious vomiting, coma, and increased intracranial pressure, can be prevented by avoiding aspirin therapy in children or adolescents with chickenpox or influenza. Varicella encephalitis, another rare complication of either varicella or zoster, usually appears 3–7 days after the onset of the rash and produces headache, fever, seizures, coma, or paralysis [Gilden, 2004; Hausler et al., 2002]. Myelitis causes urinary retention or incontinence, paraparesis, and sensory abnormalities [Rosenfeld et al., 1993]. Ramsay Hunt syndrome, an uncommon complication of zoster in childhood, consists of acute facial palsy, pain, unilateral hearing loss, and occasionally other cranial palsies in association with zoster of the ear or neck [Grose et al., 2002]. Children infrequently have postherpetic neuralgia.
Stroke [Askalan et al., 2001; Miravet et al., 2007; Sebire et al., 1999] or, rarely, herpes zoster ophthalmicus [Gilden, 2004; Leis and Butler, 1987] has been reported in children after varicella. Usually occurring within 4–8 weeks of varicella or zoster infection, these disorders produce focal deficits, headache, lethargy or somnolence, and occasionally seizures. The pathogenesis of stroke in these pediatric cases appears to reflect vasculopathy mediated by varicella zoster virus, as occurs in herpes zoster ophthalmicus and delayed infarction, a potential complication of varicella zoster virus reactivation in adults [Hilt et al., 1983]. The intrauterine varicella syndrome affects approximately 2–3 percent of the offspring of women who have chickenpox during their first or second trimesters of pregnancy [Alkalay et al., 1987; Brunnell, 1992; Grose, 1994]. The characteristics of this disorder include intrauterine growth retardation, cicatricial skin lesions in a dermatomal distribution, eye abnormalities (chorioretinitis, cataracts, optic atrophy), limb hypoplasia, and neurologic abnormalities (hydrocephalus, microcephaly, seizures, or Horner’s syndrome) [Alkalay et al., 1987; Grose, 1994].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree