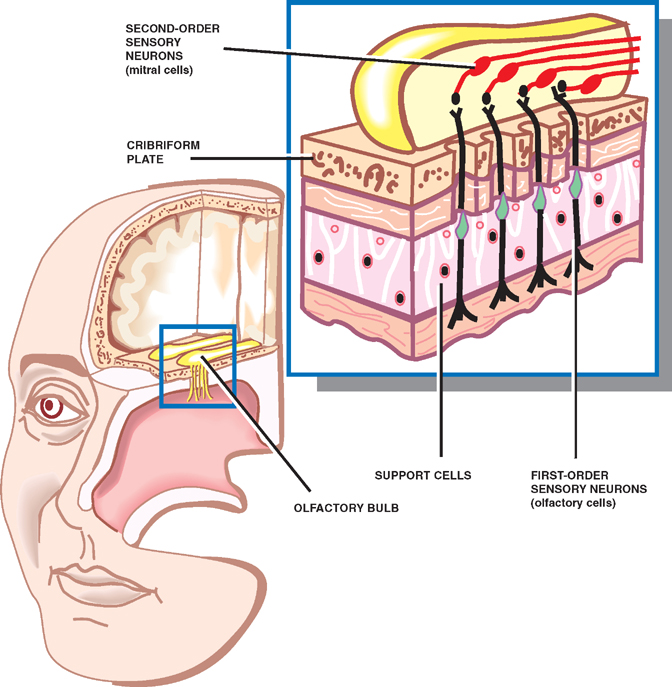
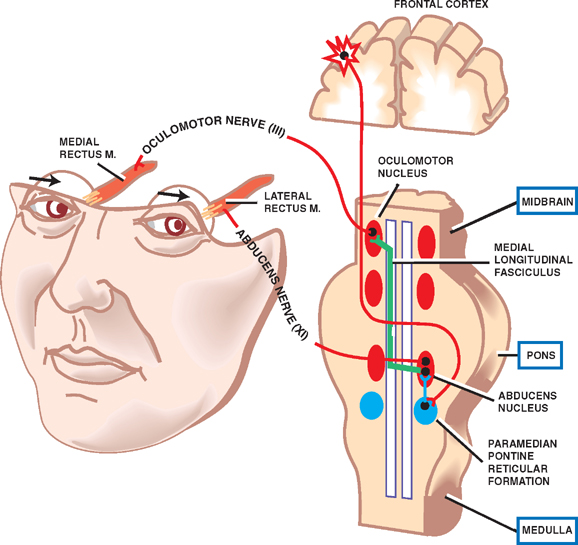
7 Cranial Nerves Because of the density of their distribution throughout the brainstem, their heavy cortical supply, and their ex-tracranial extension, the cranial nerves are sensitive indicators of both central and peripheral nervous system dysfunction. As such, an assessment of their integrity based on a knowledge of their anatomy is an important aspect of even a brief neurologic examination. Collectively, the cranial nerves serve three functions: Cranial nerves are identified by their functional components, which indicate their function (sensory or motor) and the embryological origin of the target organ they innervate (visceral or somatic). Five functional components are distinguished: somatic sensory, somatic motor, visceral sensory, visceral motor, and special sense, the latter of which includes vision (II), hearing (VIII), taste (VII, IX, X), and smell (I). On the basis of their functional components, cranial nerves are classified as purely sensory (I, II, and VIII), purely motor (III, IV, VI, XI, and XII), or mixed (V, VII, IX, and X). This chapter describes (1) the structure and function of the 12 cranial nerves, (2) the common signs and symptoms of cranial nerve dysfunction, and (3) the methods of cranial nerve testing. Subsequent chapters provide further discussion of the special senses, the somatic sensation of the face and head, and the autonomic nervous system. See Fig. 7.1. The first-order sensory neurons of the olfactory system reside in the nasal cavity. They transduce chemical stimuli into impulses that travel via unmyelinated central processes across the cribriform plate of the ethmoid bone to synapse on second-order sensory neurons that make up the olfactory bulb. Because the olfactory bulb is composed of secondary, rather than primary, sensory neurons, it is, strictly speaking, a central nervous system (CNS) tract and not a cranial nerve. Lesions of the olfactory nerve result from head trauma, tumors, tobacco smoking, and the common cold. Fig. 7.1 Olfactory nerve. See Fig. 7.2. Like the olfactory nerve, the optic nerve is not composed of primary sensory neurons and is therefore, strictly speaking, not a peripheral nerve but a CNS tract. Axons in this tract originate in retinal ganglion cells, which carry impulses generated in the photoreceptor cell layer (rods and cones) that are relayed by the intermediary bipolar cells. Projected ganglion cell fibers converge on the optic disc, turn dorsally, penetrate the sclera, and form the optic nerve. From the eyeball, the optic nerve exits the orbit through the optic canal to enter the middle cranial fossa, where it joins the contralateral optic nerve to form the optic chiasm. Central connections of the optic chiasm are described in Chapter 15. Fig. 7.2 Retina. See Fig. 7.3. The central retinal artery and vein pass through the ventral aspect of the optic nerve, which is surrounded by the three meningeal layers and bathed within the cerebrospinal fluid (CSF)-containing subarachnoid space. Because the optic nerve is confuent with the CSF, elevated CSF pressure secondary to elevated intracranial pressure is transmitted to the optic nerve and disc. The funduscopic picture that develops in this setting of increased intracranial pressure, known as papilledema, consists of (1) retinal vein engorgement and (2) blurring of the margins of the optic discs. In addition to increased intracranial pressure, the optic nerve is subject to a variety of pathological processes, including tumors and infections, as well as toxins such as methyl alcohol. Optic neuritis, a remitting relapsing infammatory process causing visual loss and pain, is a common complication of multiple sclerosis. Fig. 7.3 Pathophysiology of papilledema. See Fig. 7.4. The oculomotor nucleus is located in the midbrain at the level of the superior colliculus. Peripheral axons pass ventrally in the tegmentum of the midbrain. They penetrate the red nucleus and the cerebral peduncles to emerge between the posterior cerebral and superior cerebellar arteries in the interpeduncular fossa at the junction of the midbrain and the pons. After penetrating the dura, the oculomotor nerve courses laterally along the wall of the cavernous sinus and enters the orbit through the superior orbital fissure. At the orbital apex, the oculomotor nerve passes through the anulus of Zinn, which is the common tendinous origin of the extraocular muscles. Somatic motor components of the oculomotor nerve innervate the levator palpebrae superioris, which is responsible for the elevation of the upper eyelid, and four of the six extraocular muscles: the medial, superior, and inferior recti and the inferior oblique (the abducens nerve supplies the lateral rectus, and the trochlear nerve supplies the superior oblique). Fig. 7.4 Anatomy of oculomotor nerve (III). See Fig. 7.5. Visceral motor components, which originate in the Ed-inger-Westphal nucleus of the oculomotor complex, consist of preganglionic parasympathetic fibers. These fibers synapse in the ciliary ganglion on postganglionic neurons that form the short ciliary nerves. The short ciliary nerves supply the ciliary and constrictor pupillae muscles, which cause (1) curvature of the lens (accommodation) and (2) constriction of the pupils, respectively. Pupillary dilatation is induced by the sympathetic stimulation. The major functional components of the oculomotor nerve are summarized in Table 7.1. Fig. 7.5 Parasympathetic components of oculomotor nerve. Oculomotor nerve palsy is relatively common in clinical practice. It usually presents with the following signs and symptoms (Fig. 7.6): Oculomotor nerve palsy is associated with four pathological processes (Fig. 7.7): Fig. 7.6 Four clinical features of oculomotor nerve palsy. Fig. 7.7 Four common lesions of oculomotor nerve. The pupillary light refex involves a refex arc whereby a light stimulus elicits pupillary constriction. When light falls on the retina, impulses are generated that run along the optic nerve and tract to reach the ipsilateral pretectal nucleus. These impulses are passed on to the ipsilateral and contralateral Edinger-Westphal nuclei; from there they travel, via the ciliary ganglia, in preganglionic and postganglionic parasympathetic fibers to terminate in the constrictor pupillae. Impulses that cross the midline in their course from the pretectal region to the Edinger-Westphal nucleus constrict the contralateral pupil (indirect or consensual response); uncrossed impulses constrict the ipsilateral pupil (direct response). See Fig. 7.8. The accommodation refex occurs as a part of the adaptation of the eyes to near vision. It involves a complex arc whose afferent limb terminates in the visual cortex and whose efferent limb terminates in the constrictor pupillae, medial rectus, and ciliary muscles by way of the pretectal region. Visual responses include pupillary constriction (constrictor pupillae), ocular convergence (pretectal nuclei, motor nuclei), and an increase in the curvature of the lens (contraction of the ciliary muscle), respectively. Fig. 7.8 Lesions of pupillary light reflex. See Fig. 7.9. The trochlear nucleus is located in the midbrain just caudal to the oculomotor nucleus at the level of the inferior colliculus. After leaving the brainstem, the fibers of this nucleus pass through the cavernous sinus accompanying cranial nerves III, V1, V2, and VI and the internal carotid artery, to enter the orbit via the superior orbital fissure. The nerve then passes laterally to medially outside the anulus of Zinn, to innervate the superior oblique muscle. The superior oblique muscle causes inward rotation (intorsion) and downward movement of the ad-ducted eye. As compared with the other cranial nerves, two aspects of the anatomy of the trochlear nerve are exceptional: (1) it exits the dorsal (immediately caudal to the inferior colliculus), rather than the ventral, brainstem, and (2) its peripheral fibers decussate (in the superior medullary vellum) before they supply their target. Table 7.2 summarizes the major functional components of the trochlear nerve. Fig. 7.9 Anatomy of trochlear nerve (IV). See Fig. 7.10. Isolated paralysis of the trochlear nerve, an uncommon event, forces the eye to rotate upward and inward. Clinically, this results in vertical diplopia, which is made worse when the eye is directed downward and inward. Classically, such patients complain of difficulty while walking downstairs, the head often tilted down and toward the contralateral shoulder. Fig. 7.10 Trochlear nerve palsy. See Fig. 7.11. The abducens nucleus is located in the pons just beneath the fourth ventricle. Dorsally, it is surrounded by the facial nerve, which drapes around the abducens nucleus, forming a bulge in the fourth ventricle called the facial colliculus. After it emerges from the brainstem between the pons and the medullary pyramids, the abducens nerve courses through the cavernous sinus to enter the orbit via the superior orbital fissure. In the orbit, the abducens nerve passes through the anulus of Zinn to innervate the lateral rectus muscle. The lateral rectus muscle causes abduction of the eye. Table 7.3 summarizes the major functional components of the abducens nerve. Fig. 7.11 Anatomy of abducens nerve (VI). See Fig. 7.12. Isolated paralysis of the abducens nerve causes horizontal diplopia, forcing the affected eye to orient inward, (i.e., medial deviation of the eye). The affected patient turns the head horizontally toward the ipsilateral shoulder for forward vision. Fig. 7.12 Abducens nerve palsy. See Fig. 7.13. A combination of voluntary and involuntary eye movements allows us to find, fixate on, and track visible objects in space. Conjugate voluntary eye movements are initiated in the frontal eye field, which lies anterior to the motor cortex in Brodmann’s area 8 along the middle frontal gyrus. Frontal eye field fibers traverse the posterior limb of the internal capsule and the cerebral peduncle to terminate in the contralateral paramedian pontine reticular formation (PPRF), also known as the horizontal gaze center. PPRF neurons send axons in turn to the ipsi-lateral abducens nucleus and the contralateral oculomotor nucleus, the latter via the medial longitudinal fasciculus (MLF). The synchronous discharge that is produced in the ipsilateral lateral rectus and the contralateral medial rectus muscles results in voluntary conjugate horizontal gaze Activation of the left frontal eye fields results in conjugate horizontal gaze to the right. When rapid and precise, these voluntary conjugate eye movements are called saccades. Saccades permit the eyes to repeatedly sample the horizontal visual world to find and fixate on an object. A less characterized horizontal gaze center is located in the occipital lobe. This center permits voluntary smooth pursuit movements following objects moving in space. Fig. 7.13 Pathway for conjugate horizontal gaze. See Fig. 7.14. The palsies of conjugate horizontal gaze are divided into three clinically distinct abnormalities in conjugate gaze, based on the site of the responsible lesion. Thus (1) a supranuclear palsy is produced by a lesion that is located “above” the oculomotor nuclear complex, (2) a nuclear palsy is produced by a lesion that is located within the oculomotor nuclear complex, and (3) an internuclear palsy is produced by a lesion that is located in the midline between the oculomotor complex on either side. Supranuclear palsies involving the frontal eye field produce (1) ocular deviation in the direction of the lesion and (2) contralateral hemiplegia. Supranuclear ablation of right-sided cortical fibers in the frontal eye fields leads to unopposed action of left-sided fibers, which terminate on the right PPRF. These PPRF neurons project fibers, in turn, to the ipsilateral abducens nucleus as well as fibers that cross the midline in the MLF to reach the contralat-eral oculomotor nucleus. Activation of the left oculomotor nucleus and the right abducens nucleus evokes conjugate deviation of the eyes to the right, so that the patient “looks at his lesion.” Because corticospinal fibers located near the frontal eye fields may also be involved, a con-tralateral hemiplegia often accompanies the ophthalmo-plegia. In contrast to an ablative lesion, irritative stimulation of area 8, as occurs during an epileptic seizure, produces ocular deviation away from the affected side so that the patient “looks away from his lesion.” Fig. 7.14 Supranuclear palsies of conjugate horizontal gaze. See Fig. 7.15. A nuclear palsy involving the pons produces (1) ocular deviation away from the lesion and (2) contralateral hemiplegia. Interruption of right-sided PPRF fibers leads to unopposed activation of the left PPRF, which activates the left abducens nucleus and the right oculomotor nucleus, the latter via the crossed MLF. Activation of these nuclei results in conjugate deviation of the eyes to the left, so that the patient “looks away from his lesion.” Because corticospinal fibers located in the pons may also be involved, contralateral hemiplegia frequently accompanies the ophthalmoplegia. Fig. 7.15 Nuclear palsy of conjugate horizontal gaze. See Fig. 7.16. An internuclear palsy involving the MLF interrupts the oculomotor nucleus and results in loss of adduction of the ipsilateral eye. The contralateral eye often exhibits nystagmus (spontaneous rapid alternating movements). A lesion of the right MLF results in the left eye moving to the left (abduction), often with nystagmus, whereas the right eye cannot cross midline (i.e., cannot adduct). Bilateral MLF lesions are characteristically seen in patients with multiple sclerosis. Fig. 7.16 Internuclear palsy of conjugate horizontal gaze. See Fig. 7.17. The trigeminal nerve emerges from the brainstem at the level of the pons. It passes forward and laterally in the subarachnoid space from the posterior cranial fossa to the middle cranial fossa via Meckel’s cave over the petrous portion of the temporal bone. Functionally, it contains somatic sensory fibers, proprioceptive fibers, and somatic motor fibers. Somatic sensory fibers of cranial nerve V have their cell bodies in the trigeminal (gasserian) ganglion, which is situated in the middle cranial fossa. They innervate the skin of the face and forehead; the oral, nasal, and paranasal mucosa; and the teeth. In addition, they carry general sensory impulses from the anterior two thirds of the tongue (the posterior third is supplied by the glossopharyngeal nerve). Peripheral processes of these fibers are distributed in three divisions: the ophthalmic (V1), maxillary (V2), and mandibular (V3) branches, which exit the skull via the superior orbital fissure, the foramen rotundum, and the foramen ovale, respectively (mnemonic: standing room only). The ophthalmic and (sometimes) the maxillary divisions reach the skull via the cavernous sinus in company with cranial nerves III and VI and the internal carotid artery. Central processes of these sensory fibers continue into the brainstem, where they terminate on two trigeminal nuclei: the main sensory nucleus, which is responsible for light and discriminative touch, and the nucleus of the spinal trigeminal tract, which receives messages carrying pain and temperature information. Proprioceptive fibers are carried in the mandibular division of the trigeminal nerve. They bypass the trigemi-nal ganglion and continue into the brainstem to synapse directly on the mesencephalic nucleus. This nucleus may be viewed as a sensory ganglion that has been displaced into the brainstem because the cell body of the nucleus actually lies within the brainstem. Somatic motor fibers of cranial nerve V have their cell bodies in the motor trigeminal nucleus. Like the proprio-ceptive fibers, they are carried exclusively in the mandib-ular nerve. They innervate the muscles of mastication (the masseter, temporal, and pterygoids), the anterior digastric, the tensor tympani, and the tensor veli palatini muscles. As part of the jaw refex (contraction of the muscles of mastication in response to a tap on the slightly relaxed jaw), the mesencephalic nucleus projects collaterals to the motor trigeminal nucleus, providing proprioceptive information on the muscles of mastication. Table 7.4 summarizes the major functional components of the trigeminal nerve. Clinically, several disease states may involve the trigeminal nerve. Trigeminal neuralgia (tic douloureux) refers to paroxysms of lancinating facial pain of unknown etiology in the territory of one or more branches of the trigeminal nerve, most often a combination of V2 and V3. The etiology is most often due to vascular compression of the nerve, usually by a loop of the superior cerebellar artery. Herpes zoster virus may infect the trigeminal nerve (most frequently the ophthalmic division). This results in shingles and often postherpetic neuralgia with trigemi-nal pain. A vasculitis may also occur and may result in blindness.
The Olfactory Nerve
The Optic Nerve and the Retina

Papilledema

The Oculomotor Nerve

Parasympathetic Components


Oculomotor Nerve Palsy


The Pupillary Light Refex
Lesions of the Pupillary Light Refex
The Accommodation Refex

The Trochlear Nerve


Trochlear Nerve Palsy

The Abducens Nerve


Abducens Nerve Palsy

Conjugate Voluntary Horizontal Gaze
Supranuclear Palsies of Conjugate Horizontal Gaze

Nuclear Palsy of Conjugate Horizontal Gaze

Internuclear Palsy of Conjugate Horizontal Gaze

The Trigeminal Nerve

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








