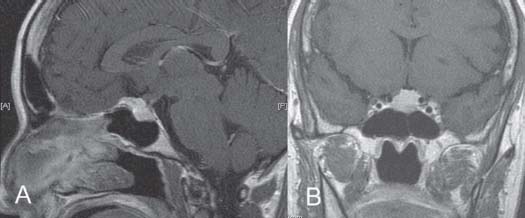
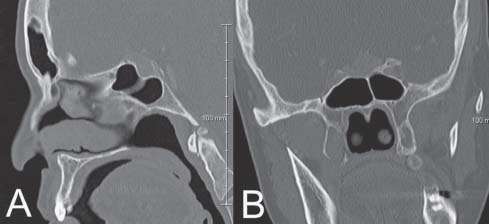
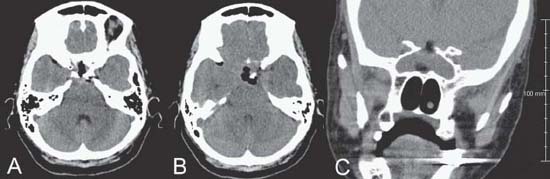
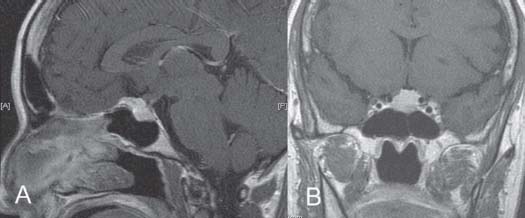
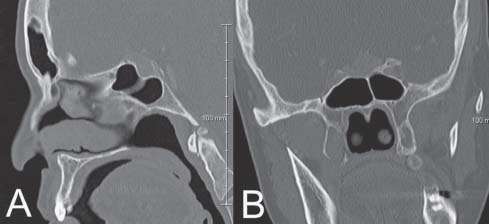
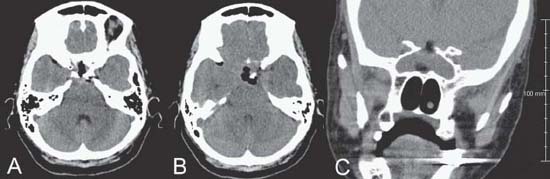
Case 12 Pituitary Adenoma Remi Nader and Marc-Elie Nader Fig. 12.1 (A) Sagittal and (B) coronal T1-weighted magnetic resonance images with contrast demonstrating lesion at the level of the sella. You obtain a computed tomography (CT) scan (Fig. 12.2) after having referred your patient to your otolaryngology colleague. The endocrinology workup reveals no abnormalities. The ophthalmologist confirms your examination findings. The patient wants to have this lesion treated. You elect to proceed with a transnasal transsphenoidal approach to resect this tumor. Your otolaryngology colleague helps with the exposure. After opening the dura, you notice that the mass behind the dura appears firm and yellowish. You send a small biopsy piece to pathology for a frozen section and you are told that this may be meningioma, normal pituitary, or adenoma. The pathologist is not able to give you an exact diagnosis based on frozen section. You then elect to remove whatever portion can be safely removed, without applying any tension on the carotid arteries or the diaphragm sella. However, you notice a small opening in the right cavernous sinus that you pack with fibrin glue at the end of the case. You also do notice a cerebrospinal fluid (CSF) fistula at the end of your resection. You were able to achieve ~80–90% resection. You were also able to remove the suprasellar portion of the mass. You left behind a part that abuts the carotid arteries directly. The patient develops transient diabetes insipidus (DI) postoperatively that lasts ~4 days. After having received desmopressin acetate (DDAVP; 3 doses), her sodium levels drop from 150 meq/L to the upper 120s mEq/L within 72 hours. However, her mental status remains stable. You watch her another few days and the sodium and urine output normalize. She develops a partial oculomotor nerve palsy on the right side, 2 weeks postoperatively. You obtain a CT scan (Fig. 12.3). You are unable to obtain an MRI as the patient had a pacemaker placed prior to her surgery. She has an elevated white blood cell (WBC) count (20,000–25,000) and no fever. A lumbar puncture (LP) reveals 0 WBC and no organisms. After discharge, she presents 4 days later with headaches, nausea, increasing urine output, hypotension, and sodium level of 143 mEq/L. Fig. 12.2 (A) A computed tomography scan of the head with sagittal and (B) coronal reconstructions demonstrating the same lesion in the sella and the sphenoid sinus anatomy at that level. Fig. 12.3 (A) A computed tomography scan of the head with axial images through the sella, (B) suprasellar, and (C) coronal reconstruction. Intrasellar and suprasellar air and fat graft are visualized. No intracranial hematoma or hydrocephalus is seen.
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
12 Pituitary Adenoma
Case 12 Pituitary Adenoma Fig. 12.1 (A) Sagittal and (B) coronal T1-weighted magnetic resonance images with contrast demonstrating lesion at the level of the sella. Fig. 12.2 (A) A computed tomography scan of the head with sagittal and (B) coronal reconstructions demonstrating the same lesion in the sella and the sphenoid sinus anatomy at that level. Fig. 12.3 (A) A computed tomography scan of the head with axial images through the sella, (B) suprasellar, and (C) coronal reconstruction. Intrasellar and suprasellar air and fat graft are visualized. No intracranial hematoma or hydrocephalus is seen.
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


