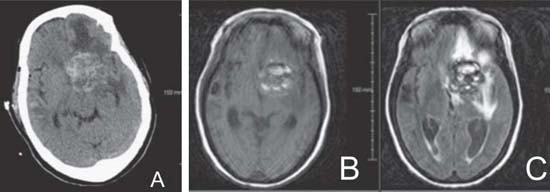
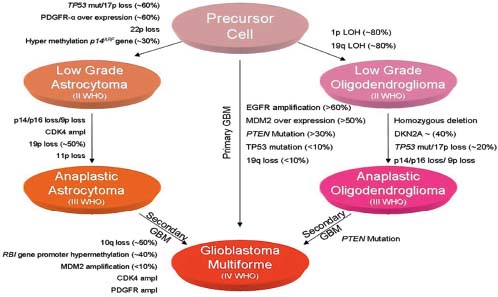
Case 15 High-grade Glioma Fig. 15.1 (A) Initial computed tomography (CT) brain without contrast obtained in the emergency room (ER). (B) T1-weighted and (C) fluid-attenuated inversion-recovery (FLAIR) magnetic resonance images of the brain obtained during initial workup. Note that the lesion does extend down to the hypothalamus (not shown in these images). Fig. 15.2 Summary of glioma progression pathways and genetic alterations. CDK4, cyclindependent kinase 4; EGFR, epidermal growth factor receptor; GBM, glioblastoma multiforme; LOH, loss of heterozygosity; MDM2, murine double minute 2; PDGFR, platelet-derived growth factor receptor; PTEN, phosphatase and tensin homologue gene; WHO, World Health Organization.
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
< div class='tao-gold-member'>
15 High-grade Glioma
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree


