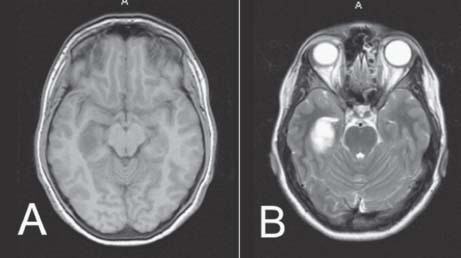
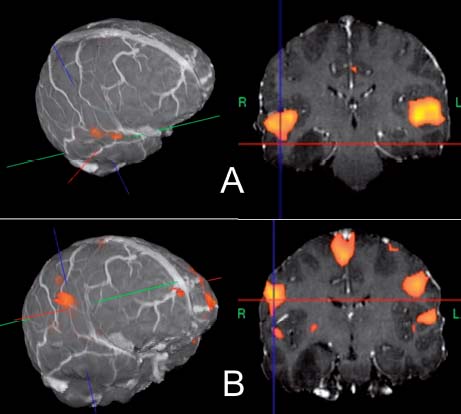
Case 16 Eloquent Cortex Low-grade Glioma Fig. 16.1 (A) T1- and (B) T2-weighted axial magnetic resonance images of the brain at the level of the temporal lobe. Fig. 16.2 Functional magnetic resonance imaging (fMRI) demonstrating bilaterality of (A) listening and (B) speech areas in the brain.
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
< div class='tao-gold-member'>
16 Eloquent Cortex Low-grade Glioma
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree


