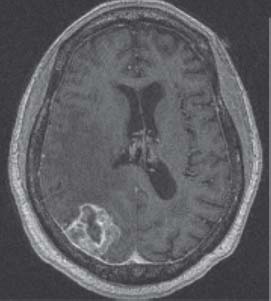
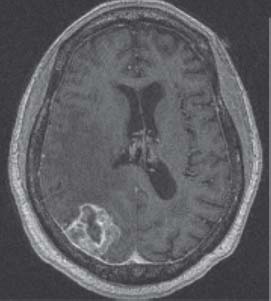
Case 17 Single Brain Metastasis Joseph A. Shehadi and Brian Seaman Fig. 17.1 Computed tomography (CT) scan of the brain without contrast. Fig. 17.2 T1-weighted magnetic resonance image (MRI) of the brain, axial cut with contrast. The patient’s left-sided weakness improved significantly with steroids. CT of the chest, abdomen, and pelvis was unremarkable. The bone scan failed to reveal evidence of skeletal lesions. Surgical intervention was sought to establish a histologic diagnosis and alleviate mass effect for symptom relief and improvement in quality of life. The patient underwent a right parietal craniotomy utilizing Stealth MRI guidance, two-dimensional ultrasonography, and intraoperative electrocortical mapping. A gross total resection was achieved. Pathology revealed metastatic squamous cell carcinoma. Postoperatively he was treated with hyperfractionated WBRT. Further investigation revealed the primary to be esophageal carcinoma. Chemotherapy was initiated consisting of 5-fluorouracil and cisplatin. The patient died 7 months later secondary to extracranial disease progression.

 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
17 Single Brain Metastases
Case 17 Single Brain Metastasis Fig. 17.1 Computed tomography (CT) scan of the brain without contrast. Fig. 17.2 T1-weighted magnetic resonance image (MRI) of the brain, axial cut with contrast.

 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


