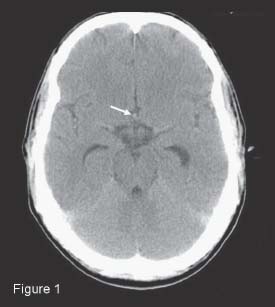
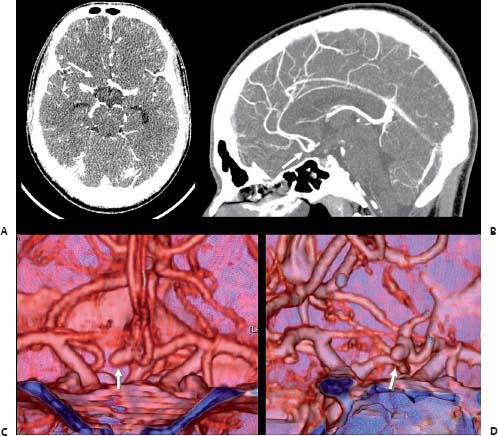
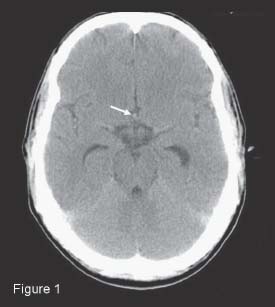
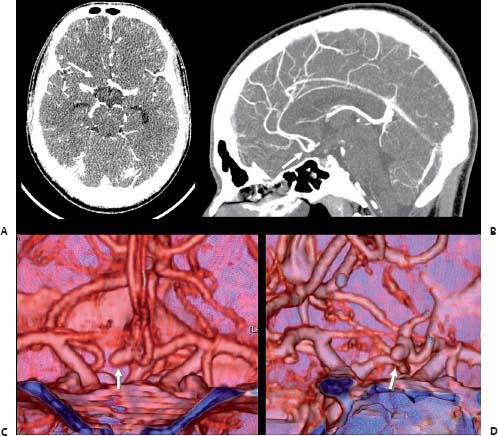
Case 31 Unruptured Anterior Communicating Artery Aneurysm Yasser I. Orz Fig. 31.1 Computed tomography scan of the head showing hyperdensity in the interhemispheric fissure (arrow). Fig. 31.2 (A) Axial and (B) sagittal contrast-enhanced T1-weighted magnetic resonance angiography images, with three-dimensional reconstructions (C) anteroposterior and (D) oblique views.
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
31 Unruptured Anterior Communicating Artery Aneurysm
Case 31 Unruptured Anterior Communicating Artery Aneurysm Fig. 31.1 Computed tomography scan of the head showing hyperdensity in the interhemispheric fissure (arrow). Fig. 31.2 (A) Axial and (B) sagittal contrast-enhanced T1-weighted magnetic resonance angiography images, with three-dimensional reconstructions (C) anteroposterior and (D) oblique views.
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


