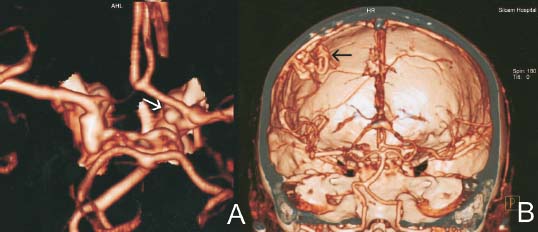
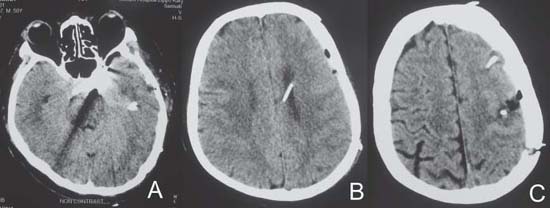
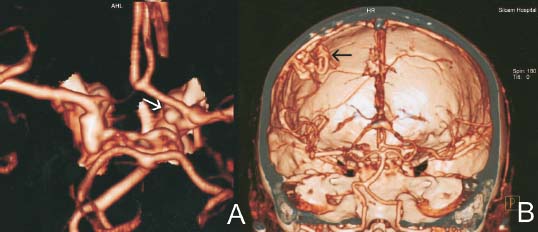
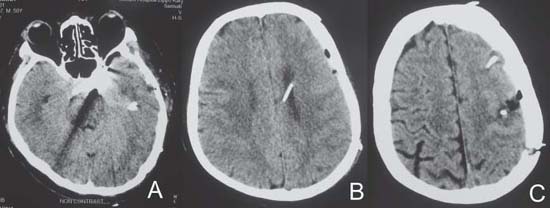
Case 35 Concomitant Arteriovenous Malformation and Aneurysm Julius July and Eka Julianta Wahjoepramono Fig. 35.1 Plain axial computed tomography scan of the head. Fig. 35.2 Three-dimensional reconstructed computed tomography angiogram showing (A) aneur ysm (white arrow) and (B) ar teriovenous malformation (black arrow). After the surgery, the patient had an excellent recovery. The partial left third nerve palsy did not resolve, however, no new neurologic deficits were noted. He was observed one night in the intensive care unit then moved to the ward. On the third day after the surgery, he developed slurred speech and a mild right-sided hemiparesis (power 4+/5). A CT scan was done (Fig. 35.3).

 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
35 Concomitant Arteriovenous Malformation and Aneurysm
Case 35 Concomitant Arteriovenous Malformation and Aneurysm Fig. 35.1 Plain axial computed tomography scan of the head. Fig. 35.2 Three-dimensional reconstructed computed tomography angiogram showing (A) aneur ysm (white arrow) and (B) ar teriovenous malformation (black arrow).

 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


