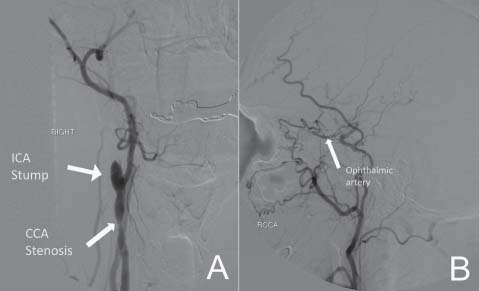
Case 41 Amaurosis Fugax with Carotid Occlusion Fig. 41.1 Magnetic resonance angiography of the neck revealing right internal carotid artery (ICA) stump. (LVA, left vertebral artery.) Fig. 41.2 Angiogram: (A) Right common carotid artery (CCA) injection showing internal carotid artery (ICA) distal stump (arrow) and CCA stenosis (arrow). (B) Selective external carotid artery injection showing communication between the internal and external circulation via the ophthalmic artery (arrow). (RCCA, right common carotid artery.)

 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
< div class='tao-gold-member'>
41 Amaurosis Fugax with Carotid Occlusion
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree


