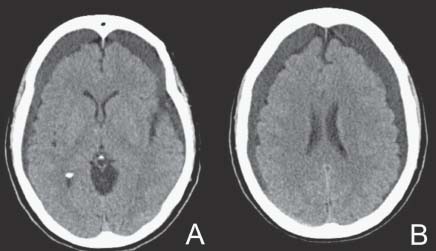
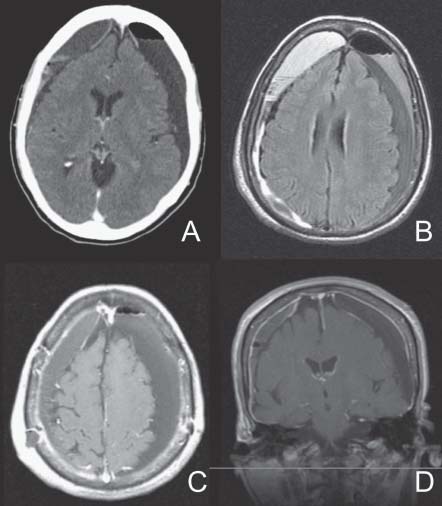
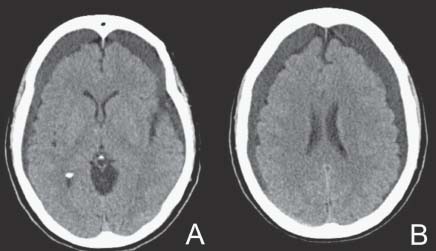
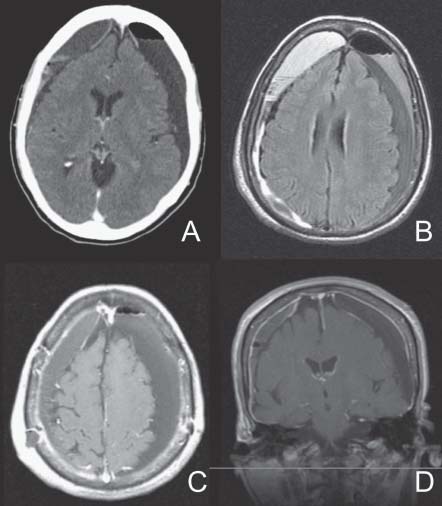
Case 45 Chronic Subdural Hematoma Remi Nader Fig. 45.1 (A,B) Computed tomography scan of the brain without contrast. The patient is on no anticoagulant or antiinflammatory medications. Her laboratory results including complete blood count, electrolytes, and coagulation profile are within normal limits. You had a discussion with the family about the treatment options and they opted for surgery. She does well from bilateral burr-hole evacuation of subdural hematomas, and is discharged home. However, she comes back 3 weeks later to your clinic. She now has some purulent discharge from the right posterior incision. She is somewhat somnolent and has a left hemiparesis slightly worse than the one she had immediately postoperatively.
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
45 Chronic Subdural Hematoma
Case 45 Chronic Subdural Hematoma Fig. 45.1 (A,B) Computed tomography scan of the brain without contrast.
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


