Case 52 Other Penetrating Intracranial Trauma
Domenic P. Esposito
- A 27-year-old man presents to the emergency room (ER) with a history of being struck in the head with a blunt object.
- The initial Glasgow Coma Scale (GCS) in the ER is 15.
- There are no focal neurologic deficits.
- A computed tomography (CT) scan is obtained and shown in Fig. 52.1.
Fig. 52.1 Computed tomography scan of the head with (A) scout image, (B) axial, and (C) sagittal views, showing depressed skull fracture in the occipital area.
Fig. 52.2 Magnetic resonance imaging (MRI) of the brain with coronal T2-weighted (A) and sagittal T1-weighted (B) images showing the depressed skull fracture with underlying brain contusions. Magnetic resonance venography (C) showing disruption of the posterior portion of the superior sagittal sinus.
< div class='tao-gold-member'> Clinical Presentation
Clinical Presentation Questions
Questions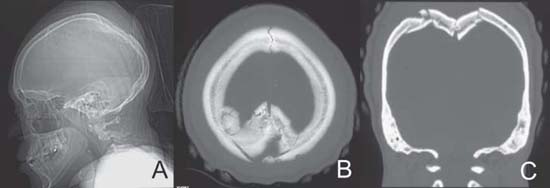

 Answers
Answers


