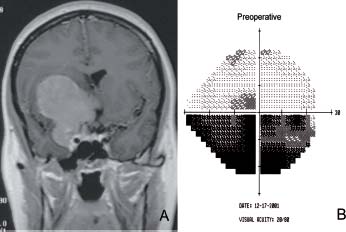
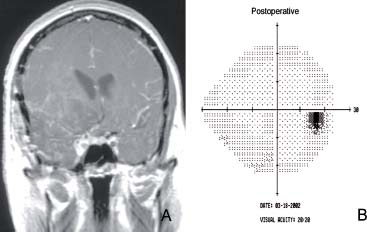
Case 9 Clinoidal Meningioma Fig. 9.1 (A) T1-weighted postcontrast coronal magnetic resonance image showing a 7 cm enhancing mass arising from the anterior clinoid process and compressing the chiasm laterally and superiorly. (B) Visual field examination is shown on the right and reveals an inferior arcuate visual field defect. Fig. 9.2 (A) Postoperative T1-weighted postcontrast coronal magnetic resonance image showing gross total resection of the tumor with minimal residual within the cavernous sinus. (B) Postoperative visual field examination is shown on the right and reveals resolution of the defect.
 Clinical Presentation
Clinical Presentation
 Questions
Questions
 Answers
Answers
< div class='tao-gold-member'>
9 Clinoidal Meningioma
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree


