Figure 30.1. A schematic illustration of the brain enclosed inside the dura/cranium. ∆Pc denotes transcapillary hydrostatic pressure; Ponc plasma oncotic pressure; PA arterial inflow pressure; RA arterial resistance; RV venular resistance; Pout pressure just retrogade to the venous collapse; and ICP intracranial pressure. The magnitude of subdural venous collapse depends on the difference between ICP and PV. The existence of a venous collapse means that the change in ICP in any direction is greater than the imbalance between Pc and Ponc creating the change in ICP, and that the brain is protected hemodynamically from PV variations (see text for details).
According to these principles, vasogenic brain edema can be counteracted by reducing hydrostatic capillary pressure and by normalizing the lowered plasma oncotic pressure. The first can be accomplished by reducing arterial pressure from the commonly raised levels towards normal values (see below) and, the second, by increasing the plasma oncotic pressure by colloid infusions. Note that the limit for adequate arterial pressure is lower in the sedated patient in a horizontal position than in the awake mobile patient. The hydrostatic capillary pressure will vary more with the arterial pressure in the injured brain with depressed autoregulation than in the normal brain.
Reducing arterial pressure with antihypertensive treatment should only be initiated from a normovolemic state (see below) and only with drugs which do not induce cerebral vasodilation, which per se will increase intracranial blood volume and ICP. Drugs with beta1-selective antagonistic, alpha2-agonistic and angiotensin II antagonistic effects are therefore recommended. Moderate head elevation can be used, if necessary, to reduce the hydrostatic capillary pressure from the arterial side. Plasma oncotic pressure can be normalized with albumin infusions (see below). In contrast to the hydrostatic transcapillary filtration effect, the oncotic absorbing effect is independent of the brain’s autoregulatory capacity. Note that the reduction in brain edema following a shift in the balance between the hydrostatic and the oncotic pressure towards absorption is slow, and it may take several hours before any signs of ICP reduction will appear.
As mentioned above, normal ICP (about 10 mmHg) is always higher than extradural venous pressure, creating a passive venous collapse just inside the dura (venous outflow resistance, Figure 30.1). The magnitude of the collapse depends on the difference between ICP and the extradural venous pressure. By an automatic passive adaptation of the degree of venous collapse to the difference between ICP and extradural pressure, the brain is protected hemodynamically against venous pressure variations [6,8]. For example, it is because of this passive mechanism that brain circulation is not influenced on the venous side by head elevation or the use of positive end-expiratory pressures (PEEP) in the ventilator. Therefore, PEEP has no side effects on venous drainage and should always be used in head-injured patients to prevent atelectasis. The initial reduction in ICP following head elevation can be explained by a blood volume reduction on the arterial side and to some extent from the gravitational force in the spinal canal, but not by an increase in venous drainage. A more long-term ICP-reducing effect of head elevation can be explained by the reduction in hydrostatic capillary pressure when arterial inflow pressure to the brain is reduced, analogous to the effect of antihypertensive treatment.Osmotherapy given in a single bolus dose of hypertonic saline can be used as a life-saving means to prevent an incipient brainstem herniation, while awaiting the effect of other ICP-reducing measures. Mannitol should not be used due to its adverse rebound effect on brain edema.
30.4 Decompressive Craniotomy and Other Surgical Measures
Evacuation of hematomas and focal lesions may reduce the release of inflammatory substances and result in less edema. Decompressive craniotomy will offer extra space to the brain, reducing the risk of herniation. Decompressive craniotomy, however, also causes a loss of transcapillary counterpressure when ICP is reduced which, in the injured brain with a disrupted BBB, will result in transcapillary filtration with the risk of herniation through the cranial opening. Transcapillary filtration may also explain the slow recovery in ICP from the lowered value often seen soon after the operation. These adverse effects can be counteracted by preventing unnecessarily high arterial pressure and by maintaining normal plasma oncotic pressure. Also, the ventricular collapse sometimes seen after CSF drainage can be explained by the induced imbalance between transcapillary hydrostatic and oncotic pressures, and the loss of CSF will be replaced by brain edema with an increased risk of brainstem herniation. Continuous CSF drainage, therefore, must be done with great caution and, when performed, done under computed tomography (CT) control of the ventricular volumes.
30.5 Microcirculation Around Contusions
According to the analogy to Ohm´s law, tissue perfusion relies on perfusion pressure and vascular resistance. The vascular resistance of the penumbra zone depends on several factors, such as the vasoconstrictor state of vessels, degree of micro-occlusion and wall adherence of various blood cells. This means that blood flow to the penumbra zone can be improved by increasing CPP and by decreasing its vascular resistance. According to the fourth power relationship between radius and resistance as formulated in Poiseuille’s law, even small variations in vessel radius may result in large variations in vascular resistance in areas with increased resistance, such as the penumbra zone. It follows then that a relatively small decrease in the radius of a vessel or an increase in the degree of micro-occlusion/adherence in the penumbra zone will result in a large decrease in perfusion. Therefore, it is much more important for the perfusion of the penumbra zone to minimize vascular resistance than to maintain a high CPP. The paragraphs below deal with different measures to improve penumbra zone perfusion.
30.6 Maintenance of Normovolemia to Improve Cerebral Microcirculation
Hypovolemia compromises cerebral circulation via an alpha-mediated effect secondary to activation of the baroreceptor reflex. As shown experimentally in piglets, hypovolemia has a great adverse impact especially on the traumatized brain [10]. Prevention of excessive baroreceptor reflex activation, and the concomitant catecholamine release by keeping the patient normovolemic, is probably the most important measure to preserve microcirculation of the penumbra zone. Preservation of normovolemia under a generally increased permeability is, however, a sophisticated task, as explained below.
Unless adequately treated with intravascular volume substitution, head trauma patients will develop hypovolemia due to increased permeability in most body organs and a reduced recirculating capacity of the lymphatic system in the unconscious immobile patient. The transcapillary escape rate (normal, 5-7% of total plasma volume per h) may increase significantly above the level of the lymphatic capacity, which will increase the interstitial protein concentration in combination with tissue edema.
When using a crystalloid solution as plasma volume expander, the infused volume must be much greater than that when using a colloid solution, as crystalloids are distributed quickly throughout the whole extravascular space, resulting in general tissue edema. More importantly, the crystalloid solution will also be distributed to the interstitial space of the injured brain with a disrupted BBB, aggravating the brain edema. Furthermore, plasma oncotic pressure cannot be maintained when crystalloid solution is used as plasma volume expander.
Normal endogenous plasma protein albumin has become the dominating colloid in severe head injury because of the potential risk with synthetic colloids of coagulation disturbances and increased intracranial bleedings, and because albumin is the only colloid that allows measurement of its plasma concentration. Plasma concentration also gives a measure of plasma oncotic pressure. Like other colloids, albumin also improves a compromised microcirculation. As will be described below, albumin has side effects mainly related to transcapillary leakage. But when used in combination with an otherwise proper therapy, protein leakage can be limited to the extent that normovolemia can be maintained with the use of moderate volumes of albumin without inducing severe side effects.
30.7 Arterial Pressure and Plasma Volume Expanders
A crucial component in the Lund therapy is to avoid hypertension with the use of antihypertensive drugs and the avoidance of vasopressors, so as to prevent or counteract brain edema. According to the 2-pore theory for transvascular fluid exchange [11], the magnitude of transcapillary leakage at increased microvascular permeability in the rest of the body depends on the hydrostatic capillary pressure – the larger the hydrostatic capillary pressure, the larger the leakage of plasma to the interstitium and vice versa. The principles of the 2-pore theory are illustrated in Figure 30.2 and will be described below. The capillary membrane has small pores permeable only to small solutes, while there are a few (about 20,000 times fewer) large pores also permeable to proteins at the venous side of the capillary network and in the venules. This means that the hydrostatic filtration force is the only force inside the large pore. In brief, the higher the hydrostatic pressure, the greater the loss of plasma fluid to the interstitium. Accordingly, the need for plasma volume substitution to maintain normovolemia will be lower in situations of low than of high arterial pressure, also resulting in less interstitial edema. It is known that vasopressor-induced increases in arterial pressure will increase the transcapillary loss of plasma fluid and proteins. This effect was confirmed in a recent study on the rat which showed a drastic increase in plasma volume loss following treatment with noradrenalin at a state of increased permeability [12].
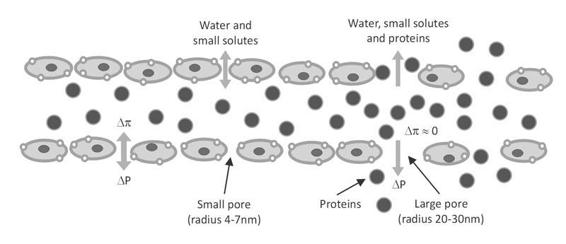
Figure 30.2. The principles of the 2-pore theory for transcapillary fluid exchange in the body (not the brain). The capillary membrane with its numerous small pores and its few large pores at the venous side of the capillary network. While the transcapillary hydrostatic and the oncotic pressure balance each other across the small pores according to the Starling fluid equilibrium, the hydrostatic filtration force is the only force acting across the large pore, as the oncotic pressure is equal on both sides of the membrane for the large pore. Plasma proteins are lost mainly via convection following the fluid stream through the large pore. This means that an increase in hydrostatic capillary pressure will increase the loss of plasma proteins (see text for details).
Most likely, due to its effect on hydrostatic capillary pressure, overtransfusion will increase the loss of plasma fluid to the interstitium, as shown experimentally in the rat, and should therefore be avoided [13]. The need for albumin transfusions can also be reduced by increasing the recirculating lymphatic capacity of proteins with a more effective physiotherapy and by keeping a relatively normal hemoglobin concentration (see below).
30.8 Albumin and Erythrocytes as Blood Volume Expanders
There are no studies evaluating the effect of blood transfusion to maintain normovolemia in patients with severe head injury. The need for plasma substitution, however, will be lower when the hemoglobin concentration is normal than when it is low, because a low hemoglobin concentration indicates that the loss of red blood cells must be replaced by a similar large volume of plasma to avoid hypovolemia. A low hemoglobin concentration raises the risk of larger transcapillary leakage of plasma to the interstitium. It has also been shown in the dog [14] and the rat that the loss of plasma volume to the interstitium is larger at a low than at a normal hemoglobin concentration. This is in accordance with our clinical experience where we noted less need for albumin at normal than at low hemoglobin concentrations and that the frequency of undesired hypotensive periods were markedly reduced. Modern research has also shown that optimal oxygenation of the brain occurs when the hemoglobin concentration is close to normal [15]. Most likely, net oxygen delivery to the brain is higher at a normal than at a low hemoglobin concentration in spite of the higher blood viscosity. There are arguments for the use of red blood cell transfusions to achieve normal hemoglobin values, and the Lund therapy recommends erythrocyte transfusions up to a lowest hemoglobin concentration of 12 g/dl. To reduce the side effects associated with blood transfusion, leukocyte-depleted blood and a short storage time of the blood are strongly recommended.
According to the principles described above, normovolemia cannot be achieved in spite of large volumes of albumin infused under acceptance of low hemoglobin concentrations and acceptance of a high arterial pressure, and especially when using vasopressors. Large volumes of albumin infusion do have side effects, which most likely can be related to an increased loss of plasma to the interstitium as a result of vasopressor therapy. This may explain, at least partly, why outcome with albumin was not better than with 0.9% saline [16]. However, when used correctly as a part of the Lund therapy, albumin is most likely the best plasma volume expander available today for severely head-injured patients. This is not only because of its endogenous nature or that the volumes of albumin needed are relatively small to maintain normovolemia, but also because it preserves a relatively normal oncotic pressure. Serum albumin levels were recently shown to be a favourable predictor of outcome after severe head injury [17]. Therefore, albumin is recommended as the main plasma volume expander in the Lund therapy. Higher concentrations of albumin (20-25%) are to be preferred, as higher concentrations have a relatively better plasma volume expanding effect and smaller transcapillary leakage. Furthermore, the peak concentration of albumin following a fast infusion will cause a larger transcapillary leakage of albumin than when albumin is given more slowly over a longer period of time.
30.9 How to Determine Whether Intravascular Volume is Adequate
No doubt, the probability of maintaining normovolemia is much higher with normal hemoglobin and albumin values than with low values – in fact, there are great difficulties to maintain a normovolemic condition with low hemoglobin/albumin concentrations. It is no guarantee, however, that the patient is normovolemic even when hemoglobin and plasma albumin (protein) concentrations are normal. A blood pressure below acceptable values in spite of relatively normal hemoglobin and albumin concentrations indicates that the patient is still hypovolemic. In an isolated head injury, this rarely indicates the need for vasopressors. In such a situation, normalization of blood pressure with further infusion of erythrocytes, perhaps in combination with albumin infusion, will confirm whether the patient is hypovolemic or not. Hypovolemia is the main cause of hypotension in most head-injured previously healthy patients. It must be stated from the principles described above, however, that we cannot fully normalize the intravascular volume whatever the blood volume expander given without inducing side effects such as interstitial accumulation of fluid and proteins, but the side effects will be minimized with use of the therapeutic principles of the Lund therapy. In this respect, avoidance of vasopressors and the use of antihypertensive therapy and transfusion to a relatively normal hemoglobin concentration hold special importance.
30.10 Other Measures to Improve Cerebral Microcirculation
Vasoconstrictors may compromise perfusion of the penumbra zone in analogy with baroreceptor reflex activation during hypovolemia, and they may also compromise microcirculation in other body organs such as the intestine, the kidney and the lung, triggering the development of the acute respiratory distress syndrome (ARDS). The use of noradrenalin, a proinflammatory drug, to increase arterial blood pressure under a hypovolemic condition may have severe adverse effects not only on brain circulation, but also on the perfusion of other body organs. Unless otherwise motivated by specific reasons, as in patients with paraplegia or those with severe sepsis, the Lund therapy does not include vasopressor therapy, vasoconstrictors or inotropic support. Beta-stimulating inotropic drugs may increase ICP through their cerebral vasodilating effects and their hydrostatic capillary pressure-increasing effect. The veno-vasoconstrictor drug dihydroergotamin was previously a component of the Lund therapy to reduce intracranial blood vlolume and ICP, but is no longer recommended due to its potential peripheral circulatory side-effects [6].
Stress-induced increases in sympathetic discharge and concomitant catecholamine release may compromise cerebral circulation of the penumbra zone. Antistress therapy is therefore an important part of the Lund therapy. Antistress therapy can include the use of sedatives and analgetics and the avoidance of awakening tests. Also, recommended antihypertensive treatments with beta1-antagonists and alpha2-agonists may have antistress properties, and beta1-antagonists may protect the heart against stress-induced microinfarctions.
Besides its metabolically-induced vasoconstriction and ICP-reducing effects, barbiturate treatment is also effective as antistress therapy. However, the traditional use of barbiturate therapy in high doses up to a burst suppression electroencephalographic (EEG) pattern and over several days leads to severe cardiovascular, electrolyte and pulmonary complications. High fever is also a common sequela of this therapy perhaps due to pulmonary complications. Barbiturates given in lower doses and over a limited period of time, however, are safe and are accepted in the Lund therapy as antistress and ICP-reducing therapy.
It is a well-established recommendation that hyperventilation should be avoided in order to avert hyperventilator-induced vasoconstriction. Short-term hyperventilation can still be of value to break a persistent ICP plateau wave or an incipient brainstem herniation while waiting for other ICP-reducing measures to take effect.
30.11 Arterial, Plasma Oncotic and Cerebral Perfusion Pressure
The optimal arterial pressure is the pressure at which transcapillary hydrostatic and oncotic forces are balanced (no transcapillary filtration). But, simultaneously, there must be an acceptable perfusion of the brain. The higher the plasma oncotic pressure, the higher the arterial pressure (CPP) can be used without transcapillary filtration. A normalized plasma oncotic pressure will allow a higher arterial pressure without filtration, resulting in better perfusion of the penumbra zone compared to a low plasma oncotic pressure.
The lower the vascular resistance of the penumbra zone, the better the perfusion and the oxygenation at a specific CPP. Therefore, a lower arterial pressure can be accepted for preventing the development of vasogenic brain edema under normovolemia and normal hemoglobin concentrations than under hypovolemia and low hemoglobin concentrations. The coupling between ICP, arterial pressure and CPP (CPP = mean arterial pressure – ICP) means that a low arterial pressure does not necessarily imply a low CPP, as a lower arterial pressure means a lower ICP.
The Lund protocol is not a CPP-targeted therapy. In principle, any CPP values in the range of 50-75 mmHg in an adult are acceptable, providing the principles of the Lund therapy are followed. Our experience is that CPP stays in the range of 60-70 mmHg in most adult patients treated according to the principles described in this chapter. CPP values in the range of 50-60 mmHg may appear and it may be necessary to reduce a markedly raised ICP; such values are acceptable only if cerebral perfusion is optimized as described above. In children, CPP is lower since arterial pressure is lower in children, and CPP values as low as 38-40 mmHg can be accepted in small children but, once again, only with use of the ICP and perfusion-targeted therapy presented in this chapter. A significantly raised ICP in a state of high CPP values despite antihypertensive treatment can be reduced by intensifying antihypertensive treatment and/or by head elevation.
In a large series of adult head-injured patients treated according to the Lund protocol, the interstitial milieu of the penumbra zone was analyzed with the microdialysis technique [18]. The study showed that the interstitial lactate/pyruvate ratio and the glycerol and glutamate concentrations decreased after initiation of the Lund therapy, and this in spite of a simultaneous reduction in CPP following antihypertensive therapy. A reduction in the lactate/pyruvate ratio reflects improved oxygenation, a reduction in glycerol and glutamate reflects less cell damage. In this study, CPP was reduced to 60-70 mmHg in the majority of patients, and the microdialysis results strongly indicated that perfusion of the penumbra zone was improved in spite of the lowered CPP.
30.12 Body Temperature Control
There is a general consensus that fever worsens outcome after severe head injury and that active cooling has neuroprotective effects. This has resulted in the marketing of equipment for active cooling. However, we still lack any randomized studies showing beneficial effects of active cooling after severe head injury. The two randomized studies performed so far, one in adults and one in children, instead showed a trend toward worse outcome in the patient groups treated with active cooling [19,20]. It may be that active cooling has adverse effects in addition to beneficial neuroprotective effect and that the net effect is not predictable.
Lowering of body temperature via active cooling below the thermostat level in the brain induces increased stress and shivering, with increased sympathetic discharge and release of catecholamines to restore the temperature back to its previous level. This may further compromise penumbra zone perfusion. Active cooling to temperatures below normal will also induce coagulation disturbances, with the risk of aggravating contusional and other intracranial bleedings. It has been suggested that the adverse effects of active cooling can be referred to the warming period. The reasons may be related to an increase in intracranial blood volume and an increase in hydrostatic capillary pressure due to a vasodilator effect induced by the increase in temperature. Unlike the situation after cardiac arrest, there are potential negative effects of active cooling after severe head injury, and especially cooling to temperatures below normal, which may explain the lack of improved outcome in the studies performed so far. Physiologically, a better alternative than active cooling would be to normalize a persistently raised body temperature by acting on the thermostat pharmacologically. A bolus dose of steroids can be used for this purpose. Due to the documented side effects of long-term treatment of severe head injury with steroids (the MRC CRASH study), steroid treatment should be limited to a single dose. Paracetamol can also be used, but its temperature-reducing effect is small, and it may have adverse prostacyclin-inhibiting effects.
The best way to prevent fever is to counteract its causes. Fever can be avoided or reduced by lowering the risk of pneumonia by minimizing atelectasis with general lung support and recruitment, the use of PEEP, inhalation and bagging. Furthermore, avoidance of proinflammatory vasocontrictors and high-dose barbiturate therapy are important measures to prevent fever in head-injured patients. Fever can also be reduced with the use of enteral instead of parenteral nutrition and by avoidance of overnutrition.
30.13 Nutrition
Nutrition should be adapted to provide the basal energy need without overnutrition, as too much energy supply cannot be utilized in these highly catabolic patients and results in an adverse increase in body temperature. From measurements of the metabolic rate in deeply sedated head-injured patients we have estimated an energy demand of 15-20 kcal/kg/day in the adult. The nutritional requirement per kg body weight in head-injured patients varies with age: it is higher in children than in adults; therefore, it should be adapted to age.
30.14 Clinical Application
A short summary of the main guideline principles is given in Table 30.1.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|




