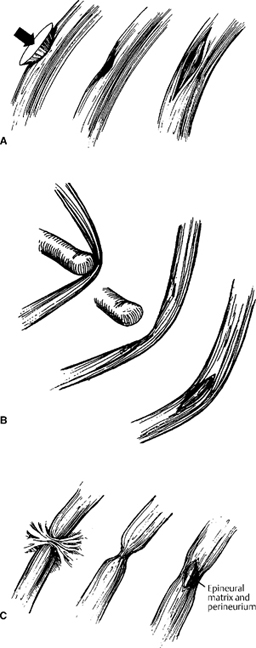
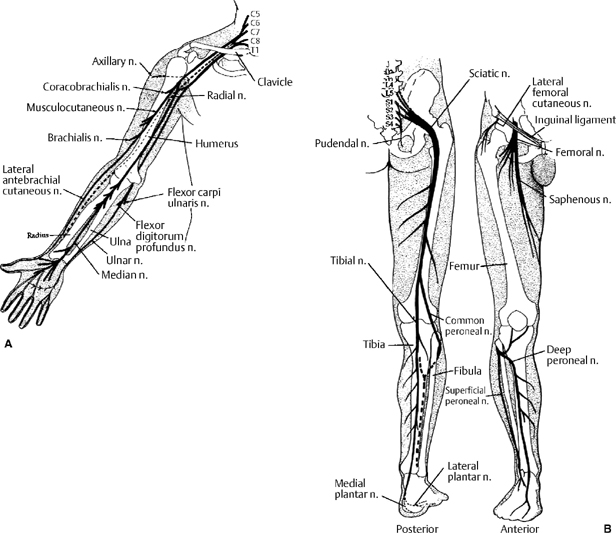
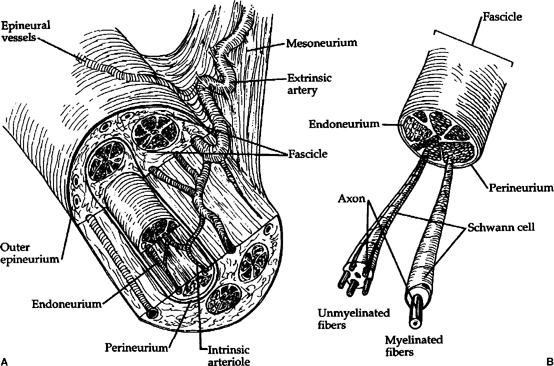
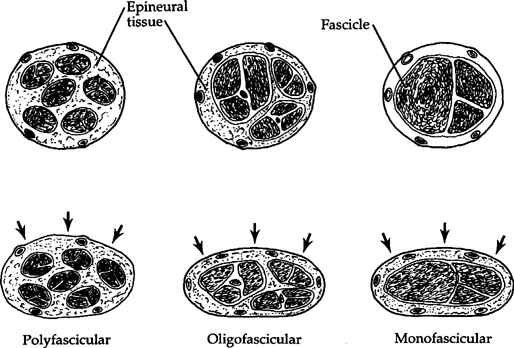
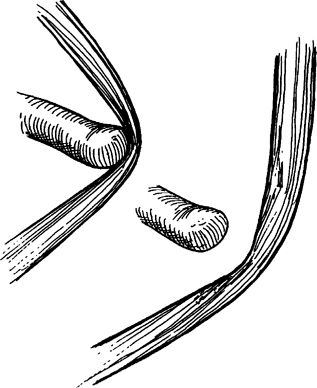
27 Acute Management of Compressive Peripheral Neuropathies Richard B. Rodgers and Mitesh V. Shah Compressive peripheral nerve injuries are very common. The evaluation of these injuries requires knowledge of the normal anatomy and physiology, as well as an understanding of the pathophysiology of nerve injury. Therefore, a brief overview of these concepts is included here. Typically, management is conservative, but occasionally operative intervention is indicated to preserve or improve function. As for any system in the body, the anatomy of the peripheral nervous system can be separated into gross anatomy and microscopic anatomy. Knowledge of the anatomical relationships of the major peripheral nerves to their surrounding structures, in addition to the motor and sensory function of those nerves, is crucial when dealing with nerve injuries (Fig. 27-1). However, a detailed discussion of the gross anatomy of the peripheral nervous system is far beyond the scope of this chapter, and the necessary information is readily available in many anatomy textbooks. One should also be aware of the existence of normal variants of the peripheral nervous system, such as the various anastomoses of the median and ulnar nerves, because these may play a role in the diagnosis and management of injury.1 A brief review of the microscopic anatomy and physiology is warranted because it directly relates to the pathophysiology and classification of peripheral nerve injury. Again, detailed information on this topic is readily available in many neurophysiology references. The basic subunit of a peripheral nerve is the individual axon. Axons are associated with Schwann cells that are responsible for production of the myelin sheath.2 Axons are bundled together in a background substance of collagen and reticulin fibers to form fascicles. This background substance and the Schwann cells make up the endoneurium. The perineurium surrounds the fascicle, and is made up of well-organized collagen fibers, which contribute to tensile strength of the nerve. The epineurium surrounds the perineurium and extends between the fascicles. It contains the blood supply of the nerve and varying amounts of connective tissue (Fig. 27-2).The number of fascicles in a nerve can vary from one (monofascicular) to many (polyfascicular) based on the individual nerve and its function (Fig. 27-3).3 The basic physiology of a peripheral nerve is based on ion gradients. Selective permeability of ion channels in the cell membrane allows an electrochemical potential difference between the inside of the nerve and the extracellular space. This potential difference allows transmission of an action potential using voltage-gated ion channels in response to a stimulus.4 The speed of conduction is based on the intrinsic properties of the nerve, specifically diameter and myelination. Larger-diameter fibers have lower resistance than smaller-diameter fibers, and therefore faster conduction. Myelin increases resistance but decreases capacitance, allowing fast conduction from node to node (saltatory conduction) with very little voltage attenuation of the action potential as it travels down the axon. Therefore, large-diameter axons that are highly myelinated have the fastest conduction velocities.3,5,6 The response of a given peripheral nerve to a compressive force is based on both extrinsic and intrinsic factors. Obviously the mechanism of nerve compression is a major component in determining the severity of injury. The intensity of the force applied, the duration of compression, and the length of nerve compressed are all crucial elements. The important intrinsic properties of the peripheral nerves that determine the response to compression include the fiber type, the amount of connective tissue and myelin within the nerve, and the vascularity of the nerve. Tissue injury occurs as the result of a combination of two major pathophysiological processes: direct structural trauma and interruption of the vascular supply. Portions of this chapter, including figures, are adapted with permission from: Robertson SC, Traynelis VC. Acute management of compressive peripheral nerve injuries. In: Loftus CM, ed. Neurosurgical Emergencies. Vol 2. Rolling Meadows, IL: American Association of Neurological Surgeons; 1994:313–326. Each peripheral nerve has a normal amount of elasticity. This elasticity is dependent on the structural composition of the nerve itself, as already described (Fig. 27-3). On average, a peripheral nerve will tolerate a stretch of -10% of its length without injury. Some nerves will tolerate less, and others up to 20%. Mechanical stretch or compression can directly disrupt the microstructure of the nerve, causing axonal or fascicular injury in an otherwise grossly intact nerve. Severe stretch can lead to macroscopic injury, including disruption of the perineurium or epineurium, and even discontinuity of the nerve itself (Fig. 27-4).7 Figure 27-1 (A) The course of major peripheral nerves in relation to skeletal structures of the upper and (B) lower extremities. Common sites of injury in the upper extremity include the clavicular region, midhumerus, medial epicondyle, and wrist. Common sites of injury in the lower extremity include the sciatic notch, inguinal ligament, femoral head, popliteal fossa, fibular head, and anterior tibia. (Reproduced with permission from the American Association of Neurological Surgeons, 5550 Meadowbrook Dr., Rolling Meadows, IL 60008; illustration from Neurosurgical Emergencies, Volume 2.) Ischemia can obviously cause injury to the peripheral nerve. Mild stretch will initially cause impairment of blood flow through the intrinsic plexus of the nerve by limiting venous return, and further stretch will limit arterial flow. Lack of venous drainage can be enough to cause significant hypoxia within the nerve. This leads to edema within the nerve, and raised intrafascicular pressures. Increased pressures can limit arterial flow within the nerve, increasing hypoxia, thereby completing the vicious circle of ischemic injury.8,9 Ischemia due to disruption of the extrinsic vascular supply can also occur and can be due to remote vascular injury or diminished flow in arterial supply and venous drainage from external compression (e.g., crushed limb or compartment syndrome).10 In general, heavily myelinated axons (and therefore larger-diameter nerve fibers) are more susceptible to injury than smaller-diameter axons with less myelin. This is partially due to the fact that Schwann cells, the source of myelin, are very sensitive to ischemia. They die and degenerate relatively quickly, leaving the basal lamina intact. This basal lamina can serve as a conduit for axonal regeneration and nerve regrowth if it is not disrupted by compressive forces. Nerve fibers with more fascicles are less susceptible to compressive forces due to the ability to redistribute those forces throughout the epineurium (Fig. 27-3). Figure 27-3 Examples of three different fiber types in the neutral state (top), and under compressive forces as depicted by arrows (bottom). The polyfascicular fiber can distribute compression throughout the epineurial connective tissue and therefore can tolerate greater forces. The monofascicular fiber is affected more severely by compression due to its relative lack of connective tissue. What is less obvious in the figure is the fact that more peripherally located fascicles are more susceptible to compression than those more centrally positioned. (Reproduced with permission from the American Association of Neurological Surgeons, 5550 Meadowbrook Dr., Rolling Meadows, IL 60008; illustration from Neurosurgical Emergencies, Volume 2.) Two popular classification systems for peripheral nerve injuries exist. Seddon initially classified peripheral nerve injuries based on the structure of the injured nerve. Shortly thereafter, Sunderland formulated a classification based more on the severity or degree of nerve injury. Both systems are commonly used, and it is important to remember that most peripheral nerve injuries cannot be purely classified into one category, and that there is considerable overlap11,12 (Table 27-1).
Anatomy and Physiology
Pathophysiology
Classification of Nerve Injuries
| Seddon | Sunderland |
| Neurapraxia: mild injury with reversible loss of function; may be complete or incomplete | First degree: loss of axonal conduction; completely reversible |
| Axonotmesis: complete interruption of axon with preservation of basement membrane, endo-, peri-, and epineurium; complete injury with distal wallerian degeneration; good potential recovery | Second degree: loss of axon continuity with preservation of endoneurium; good recovery |
| Neurotmesis: complete anatomical sever, or intact epineurium with internal disruption incompatible with recovery; complete injury; almost always requires surgical repair for any chance of recovery | Third degree: loss of axon and endoneurium, with preservation of perineurium; delayed incomplete recovery |
| Fourth degree: Loss of perineurium | |
| Fifth degree: Loss of epineurium (i.e., transected nerve) |
Evaluation of Compressive Peripheral Nerve Injuries
Although one must never lose sight of the value of the history and mechanism of the injury, the evaluation of a compressive nerve injury is usually based on three components: the physical examination, various imaging modalities, and electrophysiological testing. The physical examination is usually the most important aspect but sometimes is not reliable or must be delayed in the critically ill comatose patient. Obviously, life-threatening issues take precedence over limb function.
Examination
The examination of the patient with a peripheral nerve injury requires an adequate understanding of the anatomical relationships of the nerve to the surrounding structures and also detailed knowledge of the motor and sensory distributions of the nerve. Even in the uncooperative or comatose it is important to establish an initial exam, so that serial exams can be evaluated for an improvement or deterioration. In general, the limb or area being tested should be fully exposed, and in an ideal situation, comparison should be made with the unaffected side.13
Simple palpation of the nerve’s course can elicit pain at the site of injury and paresthesias distally. A Tinel’s sign can help determine the location of the injury, and, when present, has a fair amount of precision. However, the examiner must be aware that resting pain can radiate proximal to the injury, leading to false localization.14
The examination of motor function should be performed systematically. Motor function of each muscle group should be graded and compared with normal, usually on the well-known and utilized 0 to 5 scale. A detailed description of the motor examination of the extremities is beyond the scope of this chapter. The examiner must be cognizant of overlapping functions of muscles that may be innervated by different nerves, and specific maneuvers to isolate the function being tested. One must also be aware of compensatory movements that the patient may have adapted to overcome a deficit.13
The sensory examination should include tests of light touch, pain, and vibratory sensation. The examiner must be aware that there is significant overlap in sensory distributions of the peripheral nerves, and this overlap varies by modality. For example, the area of light touch perception of a nerve is larger than the area of sensation of painful stimuli.13 One must also be aware that the different sensory modalities have varied sensitivity to compressive injury. Disturbances in vibratory sensation occur early and with less severe compression, whereas two-point discrimination is usually the last modality affected before total sensory block.15
Electrophysiological Tests
When a peripheral nerve injury is suspected but the examination is unreliable, electrophysiological testing can be performed to help localize the injury and to assess the severity.16 These tests are not foolproof, and each has its benefits and limitations. The timing of these tests should be based on the clinical circumstances because there may be no electrophysiological changes in an injured nerve for 7 to 10 days postinjury. Neurapraxia will cause immediate changes, but less severe injuries may not show significant changes until wallerian degeneration has begun.14
Electromyography (EMG) is the study of electrical activity in the muscle in response to nerve stimulation. This is commonly called a “needle test” because it involves placing a needle electrode directly into the muscle being tested. A skilled electromyographer, usually a neurologist, can diagnose neuropathy based on the type of potentials recorded with muscle activity and can localize the neuropathy to specific peripheral nerve or root lesions. This test obviously requires extensive knowledge of the innervation order and patterns of the peripheral motor nerves. It is best performed after wallerian degeneration because early studies will not reveal denervation potentials. Fibrillations and positive sharp waves indicate acute denervation. Given that motor latencies and potentials differ with severity and time the EMG is best suited to predict the degree and duration of compression. It can also be helpful in assessing recovery because axonal sprouting changes the morphology of the motor unit signals (“nascent” potentials).17
Nerve conduction studies or velocities (NCVs) test the speed of electrical conduction in a peripheral nerve. This is performed with surface electrodes to stimulate and record the velocity and amplitude of conduction across a specific region of a nerve, and there are normal standardized values of these for the peripheral nervous system. It is best suited to specifically localize the area or even multiple areas of compression. The study will reveal focal slowing or conduction block across the area of injury, with a decrease in the amplitude of the sensory nerve action potential (SNAP). SNAPs are the most sensitive indicator of nerve compression.18 However, if the study is performed after significant wallerian degeneration, the conduction of the entire nerve may be slowed or even undetectable. Given that only larger fibers can be measured, it is not as good a test of severity because injury to smaller and slower fibers may go undetected.17 NCVs are usually performed in concert with EMG.
Somatosensory evoked potentials (SEPs) record the impulses from sensory stimulation to the central nervous system. Although they are designed to assess lesions of sensory pathways of the brain and spinal cord, they can be helpful in diagnosing a proximal peripheral nerve injury (e.g., root injury). They are not very specific due to dermatomal overlaps.
These testing modalities can obviously assist with the diagnosis of compressive neuropathy. However, they are probably of even more value in the assessment of recovery of function after a baseline study has been obtained, and are routinely repeated at various stages in the recovery process. SEPs, EMG, and nerve action potential recordings can also be utilized in the operating room during exploration of peripheral nerve injury to assist with localization and also to assess nerve function intraoperatively to guide decision making during the operation.17,19,20
Imaging
Imaging studies are usually obtained in trauma situations or in cases in which one suspects a mass lesion as a source of compressive neuropathy.
One of the most common causes of acute compressive neuropathy is extremity trauma, which is usually easily evaluated with plain x-ray films of the involved extremity. Fractures and joint dislocations rarely require any further study before appropriate treatment is initiated.
Magnetic resonance imaging (MRI) has largely supplanted computed tomography (CT) in the imaging of the soft tissues and nerves. Peripheral nerves can be identified and their courses followed on the imaging study. MRI is especially helpful in cases of peripheral nerve tumors, but it can be beneficial in the evaluation of nerve trauma. Sites of compression from a mass lesion or compartmental edema can be evaluated, and treatment can be directed at the cause of compression. Signal changes can be seen in the muscles after an injury that results in denervation. With high-resolution techniques, one can see signal change within the nerve itself at the site of injury. Although the technology is not evolved enough yet, there is potential for the ability of MRI to determine grade of injury, and therefore to determine prognosis with conservative management or need for surgery and potentially provide a noninvasive alternative to electrodiagnostic studies.21–24
Ultrasonography is emerging as a useful imaging technique both pre- and intraoperatively. Cross-sectional and longitudinal images are obtained easily, but interpretation by trained individuals is important.23
Angiography is performed when there is a vascular injury to an extremity, or if a pseudoaneurysm is suspected on examination (pulsatile mass, bruit, etc.). Myelography with or without CT can be helpful if a nerve root avulsion is suspected.