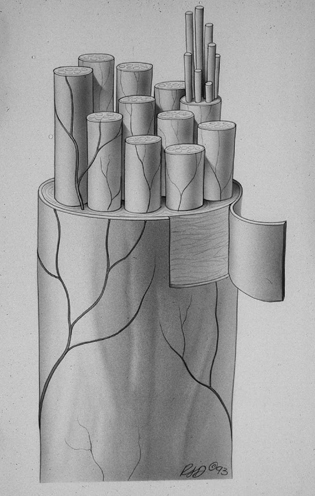
26 Acute Repair of Penetrating Nerve Trauma James T. Goodrich It is to be noted that if a nerve is cut lengthwise, it is possible to heal it by the following treatment. Steep earthworms in oil and place the oil, warmed over the fire, upon the wound three or four times with no other medications. If it is cut obliquely, it will not heal well with the foregoing treatment, and if it is completely cut obliquely, it will scarcely consolidate at all.1 This surgical therapy for an injured nerve was offered in the latter half of the twelfth century in an early Salernitan surgical manuscript, based on the writings of Roger of Salerno (Fig. 26-1). The original manuscript, interestingly, was purchased by Harvey Cushing in the 1920s and now resides in the Yale Medical School Historical Collection. Fortunately we have improved on our techniques of nerve repairs from this earlier era. The concept of what constitutes a nerve and its function is a recent development. The origins began in the eighteenth century with the early theories on “irritability.” The hypothesis that a nerve has the potential to regenerate was not developed until the serendipitous findings of William Cruikshank were published in 1795.2 Cruikshank’s primary interest was in understanding the influence of the vagus nerve on the heart. To study this problem he cut the vagus nerve in each of several animals. Later, he observed “sprouting” from the proximal ends of the severed nerves. He concluded that a nerve could actually “regenerate.” These findings provoked an outburst of controversy in the scientific community,3 which led to a delay in publication of his report because the editors believed his findings were incorrect. In some ways little has changed; controversy still awaits the adventurous surgeon who attempts to review the recent literature on the treatment and timing of peripheral nerve injury. The “correct” point of view is often difficult to determine. To avoid adding to such confusion, this chapter is based on the author’s experience in an urban population in which the frequency of penetrating injury is nontrivial. For the sake of perspective, prevailing views of the state of the art in peripheral nerve surgery are presented. This chapter’s primary emphasis is management of penetrating nerve injury in the acute setting, but for the sake of completeness, the chapter also reviews the principles of treatment for penetrating injury for which delayed surgery is indicated. Figure 26-1 A leaf (26 verso) from the “Bamberg Surgery,” a twelfthcentury manuscript, formerly owned by Harvey Cushing. (From Corner GW. On early Salernitan surgery and especially the “Bamberg surgery.” Bull Inst Hist Med 1937;5:19. Reproduced courtesy of the Yale Medical School Historical Library.) The aim of any peripheral nerve repair is coaptation of neural elements in the most anatomically accurate fashion achievable (Fig. 26-2). The nerve axon is enclosed within a sheath of perineurium, and in turn multiple axons form the fascicle. Anatomical studies have indicated that an adult human peripheral nerve can contain as many as 10,000 axons. Often not appreciated by surgeons is the fact that axons do not follow a direct, linear pathway but rather often cross over and anastomose at several points along the pathway. Another important concept concerns segregation of motor and sensory components. In the proximal portion of the nerve the motor and sensory units are diffusely scattered, and it is only distally that they segregate into discrete motor and sensory components. The surgeon must keep these concepts in mind; they explain the principle that exact matching of two cut ends of a nerve is theoretically impossible.4 Figure 26-2 Anatomy of a peripheral nerve. Sunderland’s pioneering work on peripheral nerve injury defined the key determinants of the outcome of peripheral nerve repair5: This list enables the surgeon to appreciate how little intervention one can offer, namely, only timing and technique. All else depends on the natural response of the nerve to the injury. Although a number of techniques and medications have been tried to alter and improve the response to a nerve injury, in actual fact we have really accomplished little in improving the natural outcome of the repair. In the initial evaluation of the injured nerve it is important to determine the mechanism of the injury. An incision by glass or a knife is easier to repair than one caused by a missile (bullet, shrapnel, etc.). Sharp penetrating injuries, unless contaminated, are almost always dealt with acutely (24 to 48 hours). If the cause of injury is a missile injury, the ballistic details should be worked out along with the path of the injury. The pressure waves from a bullet going through soft tissue cause various injuries. The blast effect initially paralyzes the nerve totally, leading to a neurapraxia and axonotmesis (to be discussed in further detail). Many patients with such injuries recover on their own, and short of bleeding or large compressive hematoma, acute intervention is not indicated. If the impact of the missile is sufficiently disruptive, then intraneural fibrosis can develop, causing neural conduction deficit, and later intervention (e.g., neurolysis, interposition nerve graft) will be required. It has been our experience that a missile injury is less likely to cause permanent nerve injury than a nerve incision by a knife or glass. In any peripheral nerve repair the only elements the surgeon can control with any modicum of success are the alignment of the severed nerves, including the fascicles, the tension at the suture line (which should be minimal), and the risk of infection; after that the forces of nature take over. Thus the surgeon can deal only with the technical details, and involvement in the biological process of recovery is restricted to understanding the principles that enhance recovery. Our laboratory has investigated the use of immunosuppression by means of cyclosporine in an effort to reduce internal fibrosis and to reduce rejection of homologous grafts. Growth factors, several medications, and electrical field stimulation have also been tried, though reported success has been at best marginal. Fibrin glue, different suture materials, and various conduits have also been tried but have met with only limited success. The optimal environment for a regenerating nerve has yet to be determined, though several laboratories are working to this end. The surgeon should always keep in mind a simple concept: an injured nerve should be considered, not a degenerating element, but rather a regenerating process. Discovering ways to enhance the environmental milieu to enhance regeneration is the penultimate goal. However, even with this last concept in mind, in the present state of the art, surgical technique and treatment planning remain the only elements within the surgeon’s control. A review of the surgical literature reveals an extensive number of various classifications have been introduced to describe different types of nerve injuries. It is important that the surgeon who reads such reports be familiar with the terminology and concepts associated with each of these classifications. Some might argue that the classification systems have been overemphasized, but for purposes of this chapter two useful ones are presented. In 1943 Seddon introduced a classification that is still used by most individuals interested in nerve repair.6 Its terminology has become fundamental in the peripheral nerve repair literature: Neurapraxia: a temporary disruption of nerve conduction associated with minimal injury, with usually just local ischemic demyelination Axonotmesis: moderate injury characterized by interruption of axons and their myelin sheaths. The endoneural tubes remain intact, allowing the regenerating axons to regain their peripheral connections. Neurotmesis: severe injury where a nerve has been completely disrupted or is so severely disrupted spontaneous regeneration cannot occur. As a result of wallerian degeneration and neuroma formation it is impossible for axons to regenerate distally. In 1951 Sunderland enlarged the classification using a grading system, taking into consideration more of the intraoperative surgical correlatives7 (Table 26-1). Other classifications have been proposed over the years whose details are beyond the scope of this chapter. For those interested in reviewing other classifications the article by Gentili and Hudson8 gives an excellent breakdown of several of the classifications and their electrophysiological correlates. Mackinnon and Dellon also provide an excellent review of various classifications and their anatomical correlates; these are presented in a diagrammatic format.9 See Table 26-2.
Anatomy
Basic Considerations of Peripheral Nerve Repair
Classification of Traumatic Nerve Injuries
| Classification | Description |
| Grade 1 | Loss of axonal conduction |
| Grade 2 | Loss of continuity of axons with intact endoneurium |
| Grade 3 | Transection of nerve fiber (axon and sheath) with intact perineurium |
| Grade 4 | Loss of perineurium and fascicular continuity |
| Grade 5 | Loss of continuity of the entire nerve trunk |
Source: Sunderland S. A classification of peripheral nerve injuries producing loss of function. Brain 1951;74:491–510.
| Magnification (microscope or loupes) with adequate illumination |
| Comfortable sitting position with adjustable arm rest |
| Electrophysiological monitoring for both recording and stimulation |
| Spring-loaded needle holders |
| Diamond or sapphire knives (ophthalmic cataract knives also useful) |
| 8–0 nylon for epineural repair |
| 10–0 nylon for fascicular repair |
Repair Techniques
A key concept to any nerve exploration is that the nerve should always be exposed from above and below the injury first, with the dissection of the injury site deferred until last. Blunt dissection is contraindicated because of the unacceptable torsion forces that can be exerted on the injured nerve. A no. 15 or no. 11 blade is the best instrument for the dissection. We have also added the use of disposable ophthalmic cataract knives; these are very sharp and come in several sizes and shapes. Electrophysiological monitoring is essential. Both stimulation and recording of nerve action potentials (NAPs) are key to mapping out the repair. The nerve needs to be fully dissected so that recording leads can be easily placed for monitoring. Not often appreciated is the concept that the surgeon has to be on the watch for any large feeding vessels and attempt to preserve this blood supply. Additional ischemia can easily occur to an already injured nerve secondary to removal of the nutrient blood supply.
Epineural Repair
An epineural repair technique (Fig. 26-3) requires, as the initial step, preparation of the nerve ends. In an acutely transected nerve, such as in a knife injury, the nerve ends develop a “mushroom” (i.e., the contents of the nerve herniate out). This mushrooming nerve has to be trimmed back to the epineurium. An additional guide is to analyze the surface vascularity pattern on the nerve. This pattern can act as a visual guide to anatomical alignment. Once the alignment has been determined, two 8–0 nylon sutures are placed in the epineurium, 180 degree apart. The two nerve ends are juxtaposed, taking care that tension is minimal. In some cases, further dissections of the nerve ends are needed to further relax the individual elements. Once the ends have been approximated and the tension checked, several 9–0 or 10–0 nylon sutures are placed in the epineural plane, taking care to place them through full-thickness epineurium without injuring the underlying fascicles. After the wound is closed the limb is splinted for 3 to 4 weeks to prevent undue tension on the nerve anastomosis. Repairs of this type are particularly useful in nerve injuries due to a sharp instrument leaving clean-cut edges.
Although epineural repair is an excellent technique, Edshage discussed problems that may complicate healing.10 It is often possible to fashion an anatomical anastomosis whose external appearance is quite satisfactory. However, internally fascicles may be disrupted, buckled, and poorly aligned. The gaps left behind often fill with connective tissue and in turn block neural regeneration. Despite this, the epineural repair remains a satisfactory closure. It must be repeated that magnification, illumination, and attention to fascicular alignment remain critically important.
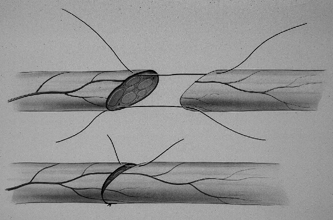
Figure 26-3 An epineural repair. Note the attention to the surface vascular details in the subsequent realignment.
Fascicle Repair
In recent years fascicle repair (Fig. 26-4) has become the most popular among peripheral nerve surgeons. The technique was introduced in 1953 by Sunderland11,12 but only became technically feasible with the introduction of the operating microscope in the mid-1960s by Smith.13 Fascicle repairs require patience, high magnification, and good microinstrumentation. This is the best form of repair in cases in which only a few large fascicles are identifiable. We particularly recommend this technique for repairing the distal portion of a nerve where severed components can typically be mobilized and juxtaposed with minimal tension. It is also useful when the nerve is partially severed and some fascicles remain intact. In delayed repair of a nerve with disrupted fibrotic ends that require resection with foreshortening of the fascicles, an interfascicular graft is more appropriate (see later discussion).
Technique
After both ends of the nerve have been identified, preliminary dissection is performed to assure they are sufficiently mobile to be approximated without tension. The superficial epineurium must be excised 3 to 4 mm to expose the fascicles. The fascicles that are to be anastomosed are then dissected from the surrounding interfascicular connective tissue. Using a 10–0 nylon suture with a small needle (typically, 50 mm) a full bite of perineurium is taken, using care not to injure the underlying fascicles. If the sutures break, the tension is too great. Occasionally, the fascicles will mushroom out and need to be trimmed back to the perineurium before closure. If the fascicles cannot be identified, as occurs occasionally, an epineural repair is performed.
Group Fascicle Repairs
This technique is similar to that of fascicle repair, but instead of isolating individual fascicles, groups of fascicles are selected for repair. In these cases, typically, interposing fascicular epineurium is present and it is in this plane the dissection is performed.
Interfascicular Nerve Grafting-Nerve Grafts
Nerve grafts have waxed and waned in popularity. With refinement in techniques and a better understanding of when to use them, they have proved effective. Clinical studies by Millesi, Samii, and others have popularized the use of nerve grafts.14–18 Some surgeons have been opposed to the concept of grafting, questioning how a proximal nerve should cross a devascularized and devitalized tissue and make connection with a degenerating distal trunk. It is beyond the scope of this chapter to review studies of graft physiology; the interested reader is referred to the work of Millesi, Samii, and others.14–18 The fact is, grafts do work, and often well. The key restricting issue in the use of grafts is the length. Several studies have clearly shown that the longer the graft the less desirable the result.19–21
In recent years there have been several attempts to devise artificial conduits for regenerating nerves. Although the preliminary results have been somewhat positive in the animal models, such has not proven to be the case in human repairs. Our experiences with these artificial conduits have not been so positive and we await better materials.
Useful Donor Sites for Graft Repairs
Nerves That Have Been Identified as Potential Donor Sites
- Sural nerve By far the most popular donor nerve is the sural nerve. It is easy to locate and provides a long graft (typical 20 to 30 cm), and its removal causes minimal morbidity. It is easily located just behind and below the lateral malleolus; by “gently” tugging on the nerve, it can be seen in outline and followed up the calf.
- Superficial radial nerve This nerve was once frequently used, but the risk of partial sensory loss to the hand has made it acceptable only as a last resort.
- Medial or lateral cutaneous nerve of the forearm
- Lateral cutaneous nerve of the femur
- Medial cutaneous nerve of the arm
- Superficial radial nerve This nerve was once frequently used, but the risk of partial sensory loss to the hand has made it acceptable only as a last resort.










