13 Anatomy for Needle Electromyography
Upper Extremity
Median Nerve
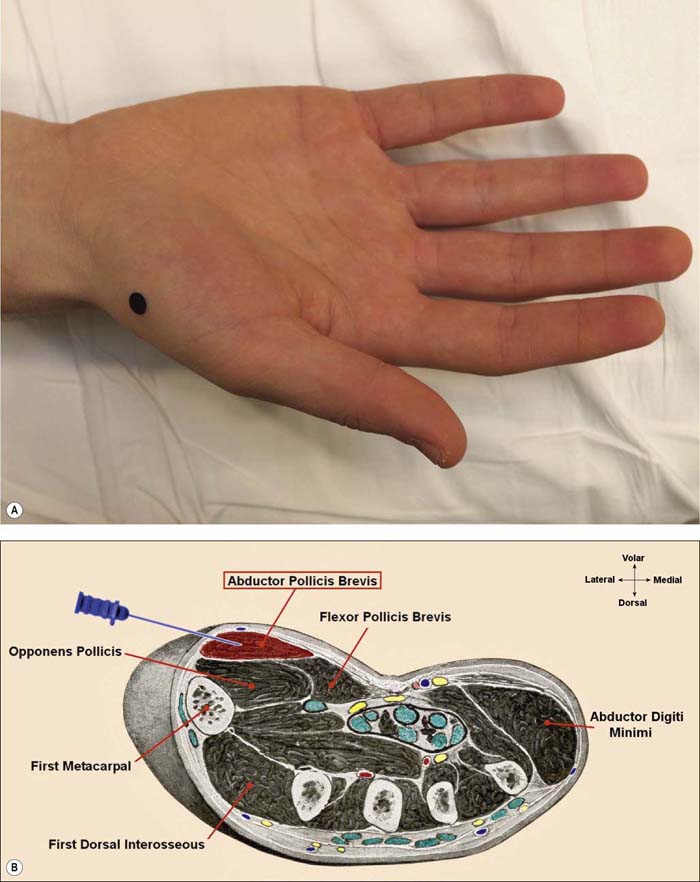
Abductor Pollicis Brevis (APB) (Figure 13–1A,B)
Key Clinical Points:
• The APB is the best median muscle to sample distal to the carpal tunnel.
• May be abnormal in carpal tunnel syndrome, proximal median neuropathies, lower trunk/medial cord plexopathy, thoracic outlet syndrome, C8–T1 radiculopathy, and distal polyneuropathy.
• Spared in anterior interosseous nerve syndrome.
• The APB often is perceived as more painful to sample than other intrinsic hand muscles.
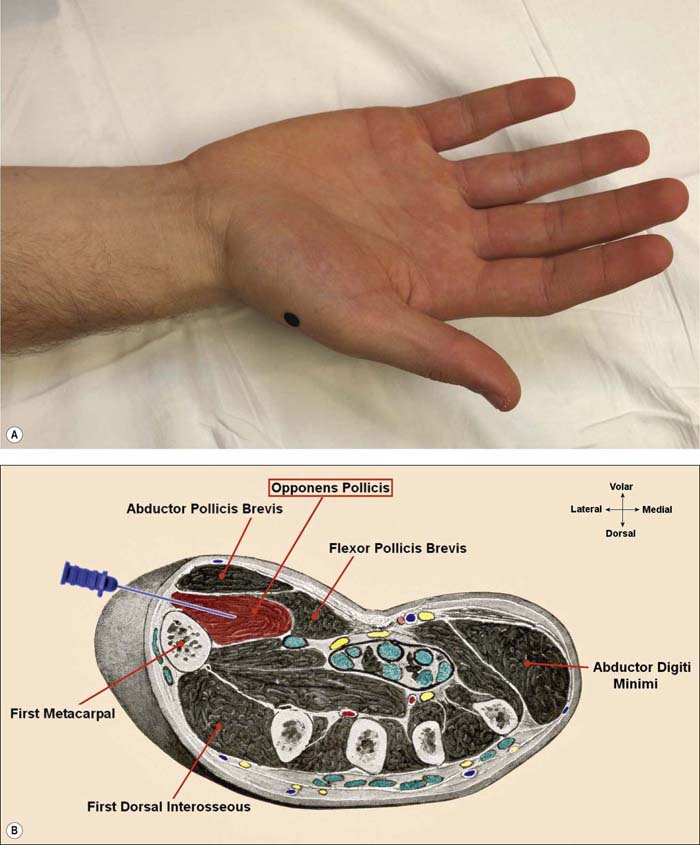
Opponens Pollicis (OP) (Figure 13–2A,B)
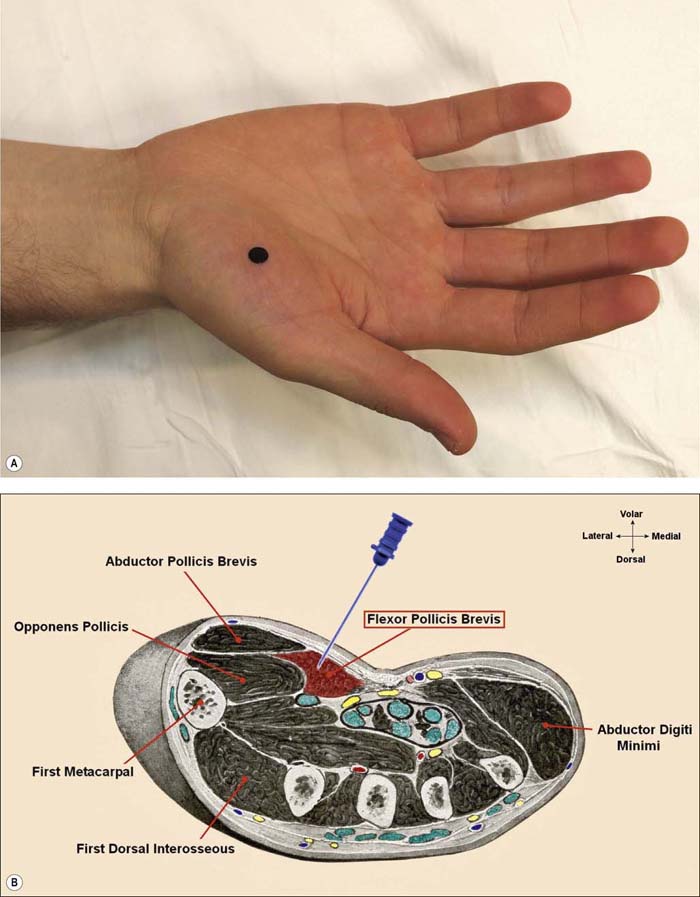
Flexor Pollicis Brevis (FPB) (Figure 13–3A,B)
Key Clinical Points:
• Sampling this muscle is often perceived as more painful than the APB.
• The superficial head usually is median innervated; the deep head usually is ulnar innervated.
• Innervation varies widely in normal subjects. In some individuals, both heads are median innervated; in others, both are ulnar.
• Because of normal anatomic variation, abnormalities should be interpreted with caution when trying to separate median from ulnar lesions.
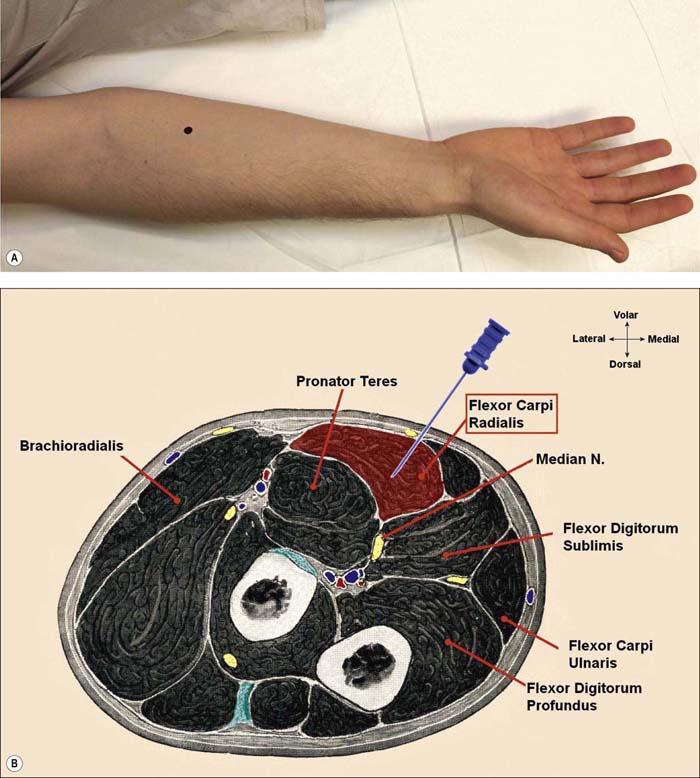
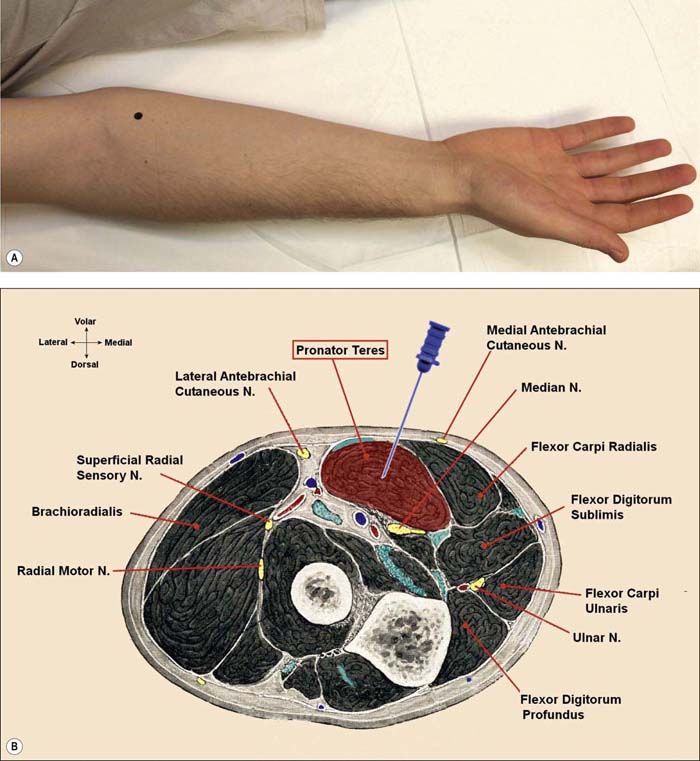
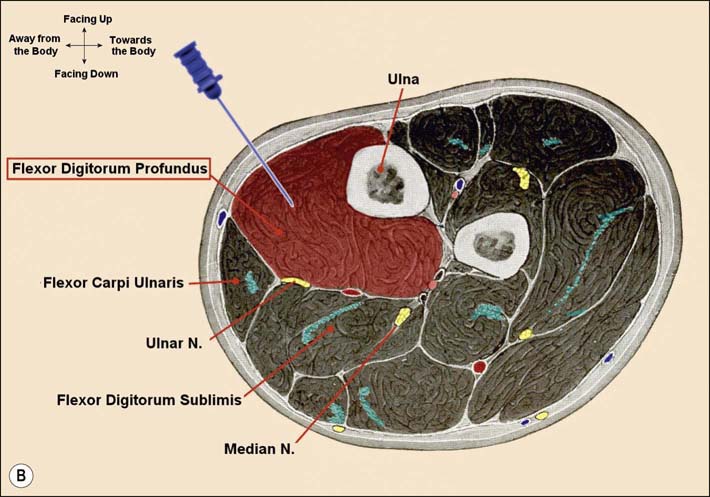
Flexor Digitorum Profundus to Digits 2, 3 (FDP 2, 3) (Figure 13–6A,B)
Key Clinical Points:
• Deeper layers are median-innervated (anterior interosseous nerve) to digits 2 and 3.
• Superficial layers are ulnar-innervated to digits 4 and 5.
• Median slips (deep) are difficult to study. The individual muscle slip can be identified by having the patient flex one finger at a time.
• The median FDP may be abnormal in anterior interosseous nerve syndrome or proximal median neuropathies.
Cross-section Anatomy Key Points:
• Caution: when placing the needle this deep, the main ulnar nerve is within reach of the needle. To avoid the ulnar nerve, the needle should be angled medially toward the body. Indeed, this muscle is best avoided unless it is needed to establish the diagnosis (e.g., anterior interosseous neuropathy).
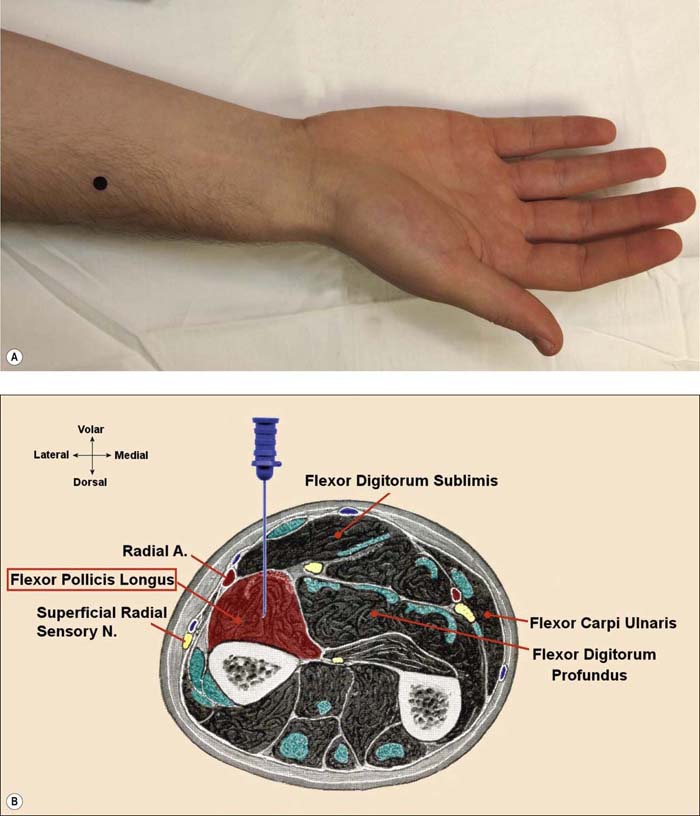
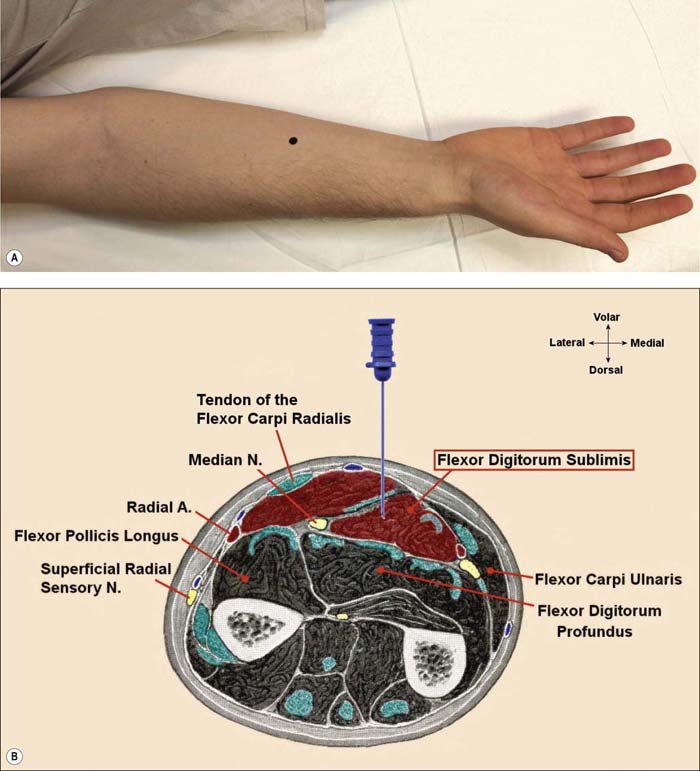
Flexor Digitorum Sublimis (FDS) (Figure 13–7A,B)
Cross-section Anatomy Key Points:
• The FDS supplies digits 2–5. The slips to different fingers can be determined by placing the needle slightly lateral or medial to the original location, and having the patient move individual fingers.
• If the needle is too deep, it will be in the FDP.
• Caution: if the needle is placed in the midline and too deeply, it may reach the median nerve.
• More difficult muscle to localize than other proximal median muscles (e.g., FCR and PT).
Ulnar Nerve
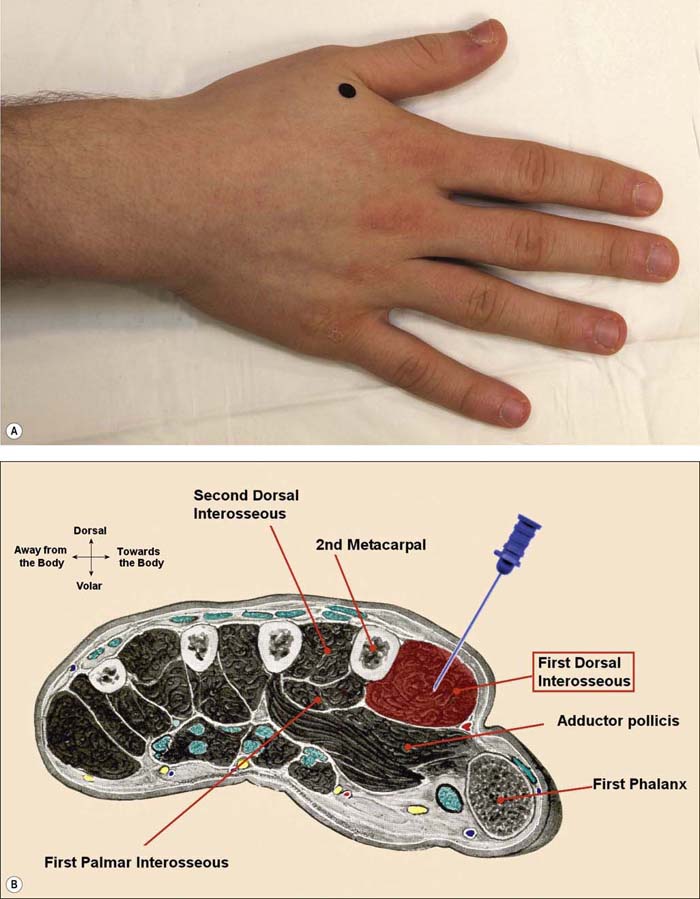
First Dorsal Interosseous (FDI) (Figure 13–10A,B)
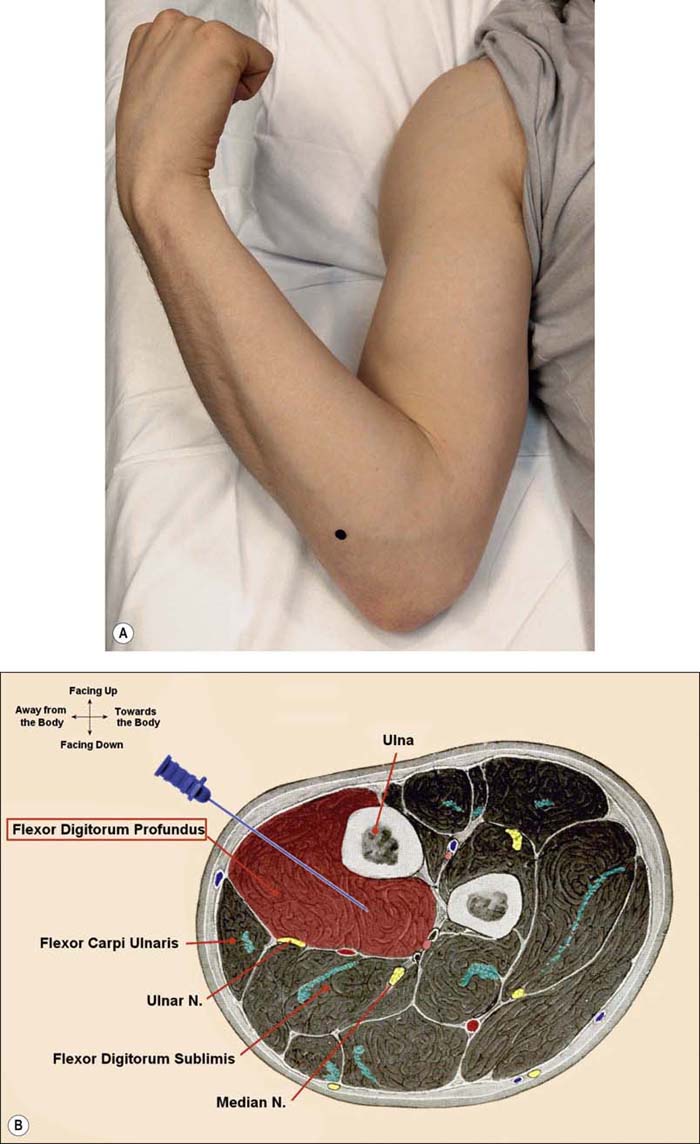
Flexor Digitorum Profundus to Digits 4, 5 (FDP 4, 5) (Figure 13–12A,B)
Key Clinical Points:
• Superficial layers are ulnar-innervated to digits 4 and 5.
• Deeper layers are median-innervated (anterior interosseous nerve) to digits 2 and 3.
• Ulnar slips (superficial) are easy to study. The individual muscle slip can be identified by having the patient flex one finger at a time.
• The ulnar FDP often is involved in ulnar neuropathy at the elbow.
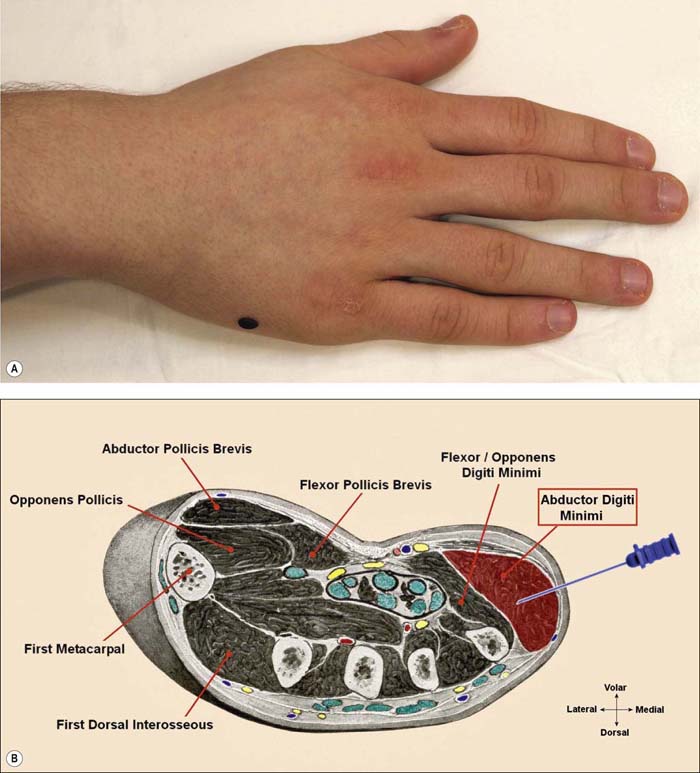
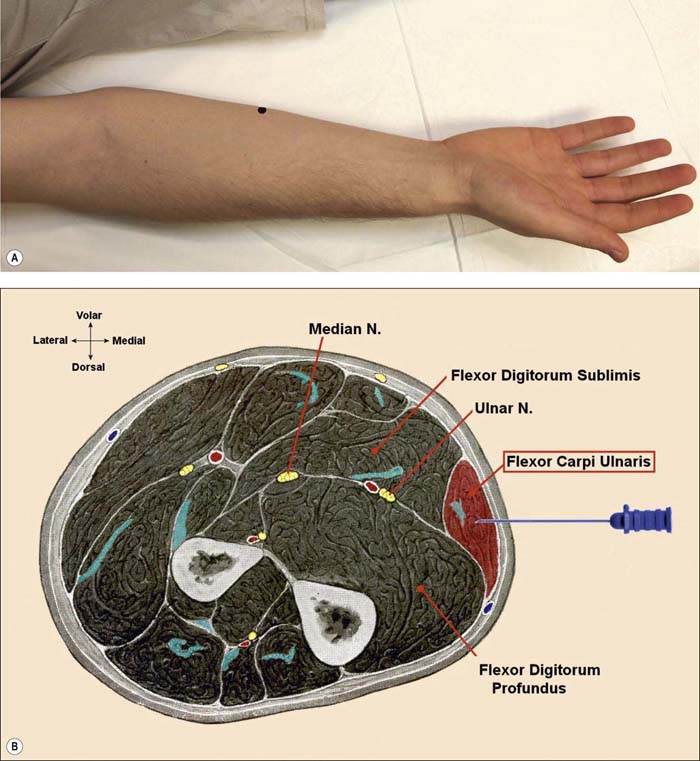
Flexor Carpi Ulnaris (FCU) (Figure 13–13A,B)
Key Clinical Points:
• To ensure the proper needle location, ask the patient to spread his or her fingers. During fifth-finger abduction, the FCU contracts to fix the pisiform bone, the origin of the ADM.
• The FCU muscle is very superficial and thin.
• The muscle often is spared in ulnar neuropathy at the elbow, especially in mild cases.
Radial Nerve
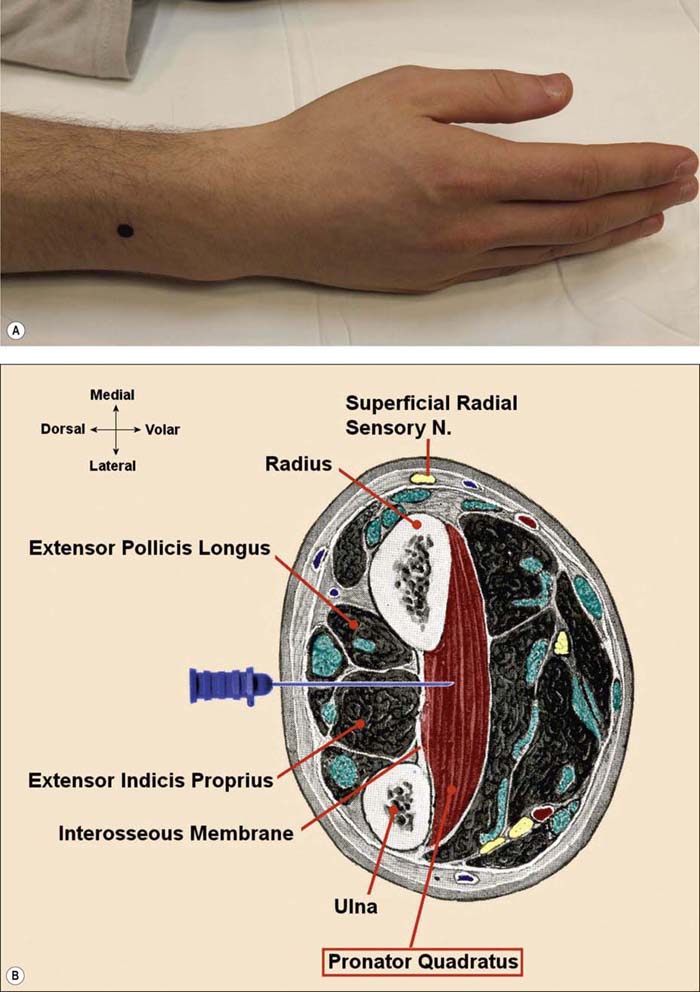
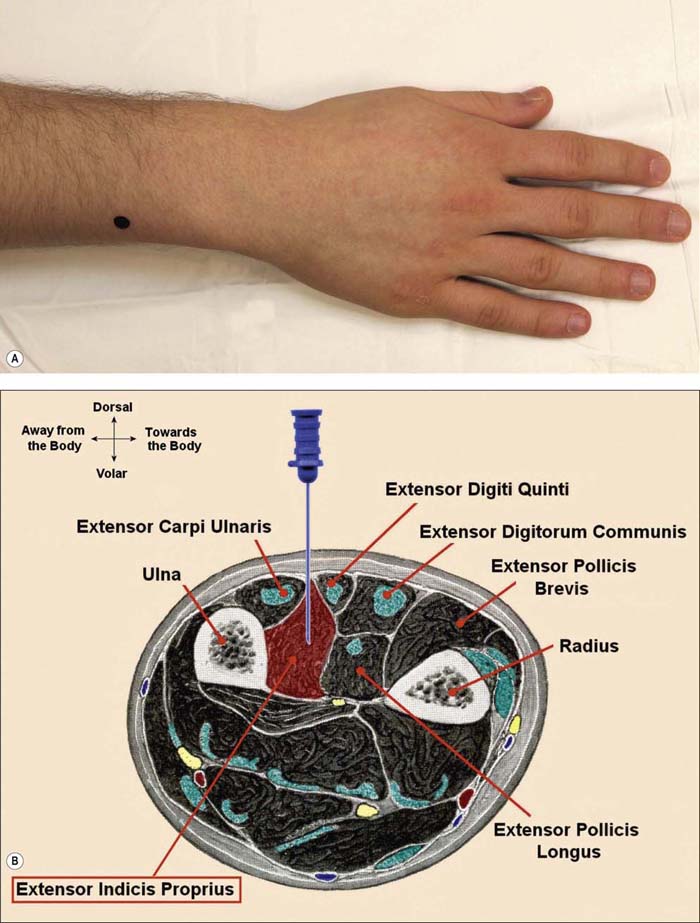
Extensor Indicis Proprius (EIP) (Figure 13–14A,B)
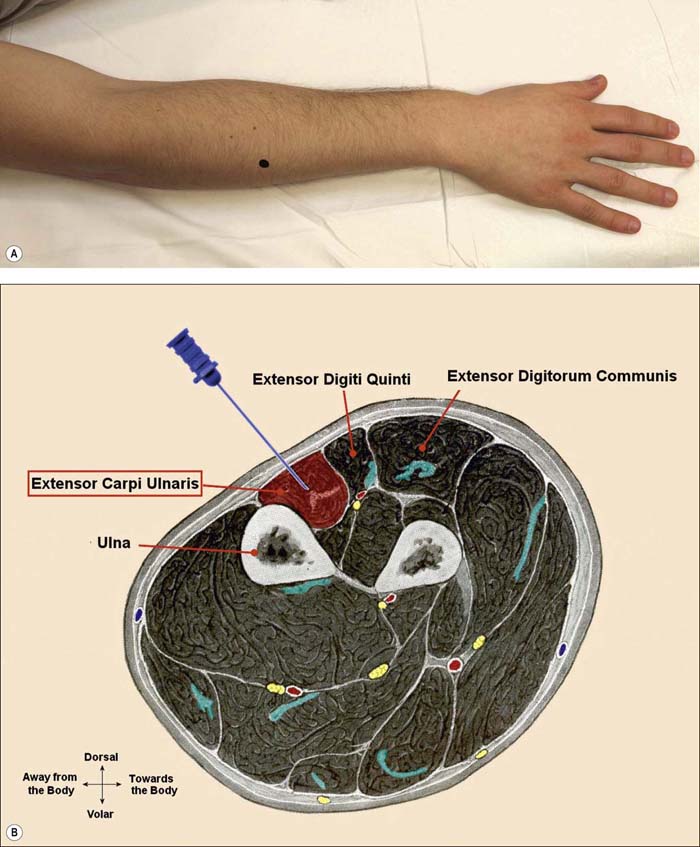
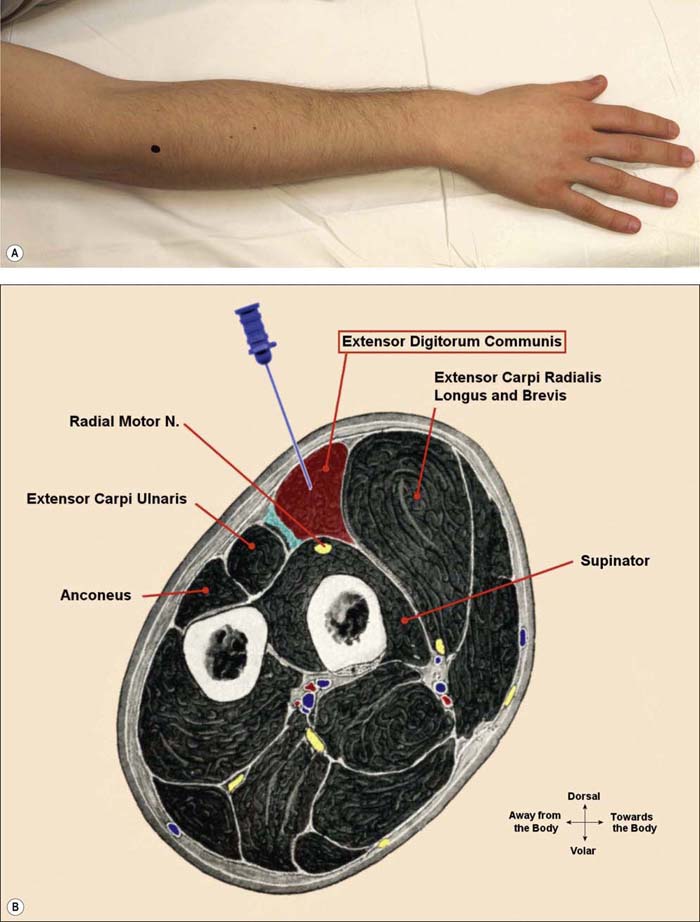
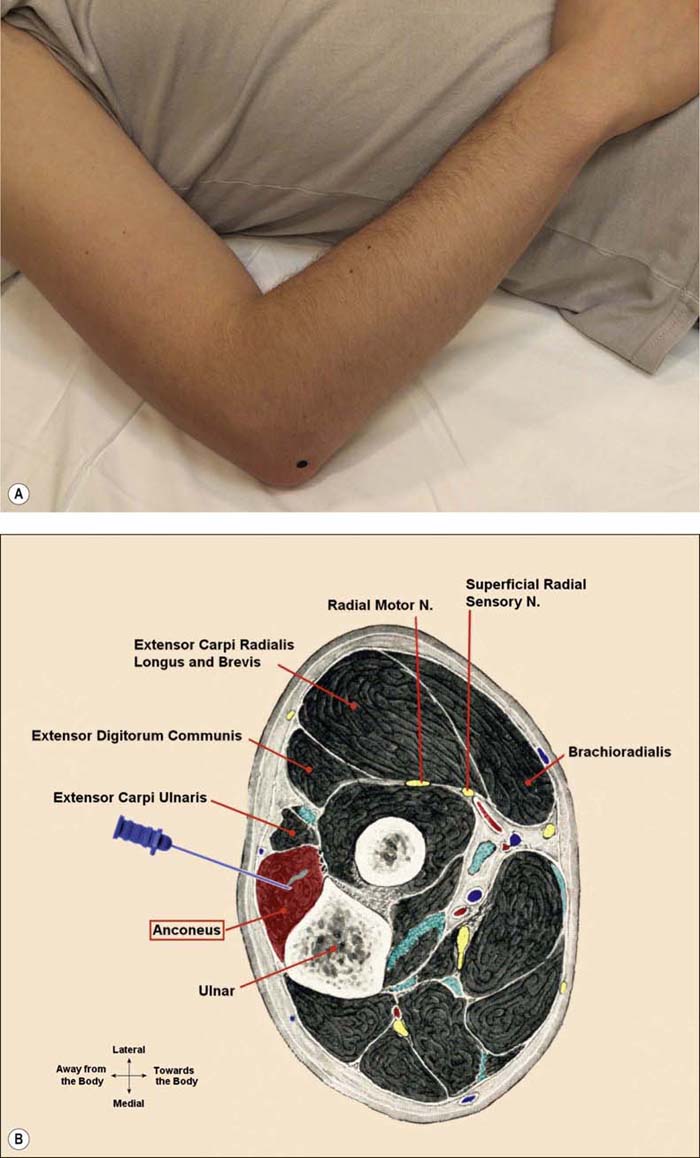
Extensor Digitorum Communis (EDC) (Figure 13–16A,B)
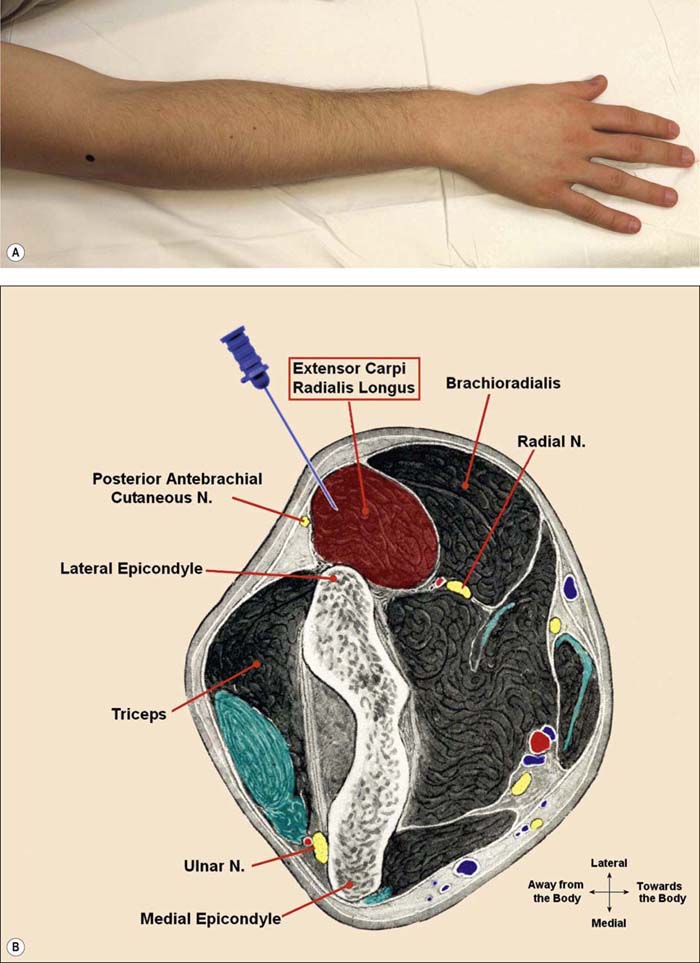
Extensor Carpi Radialis–Long Head (ECR–LH) (Figure 13–17A,B)
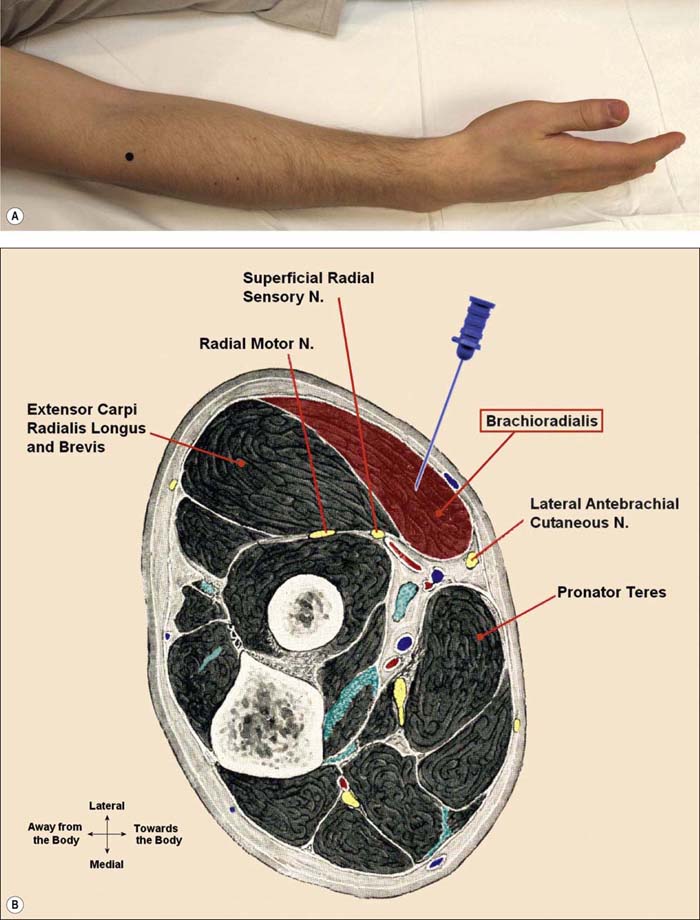
Brachioradialis (BR) (Figure 13–18A,B)
Musculocutaneous Nerve
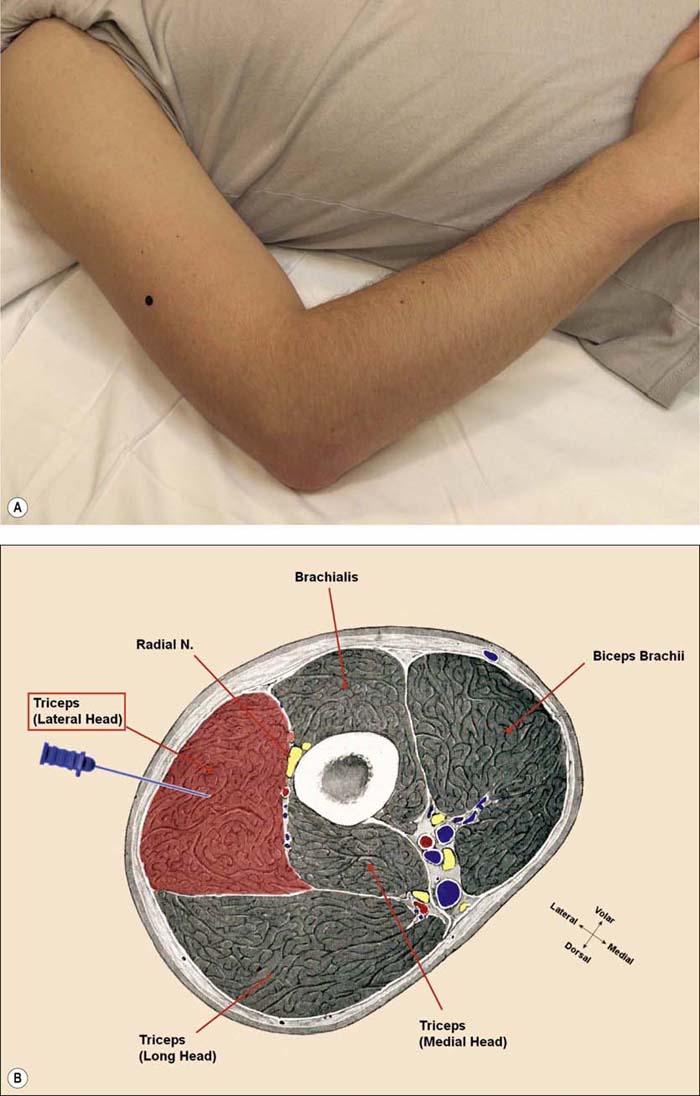
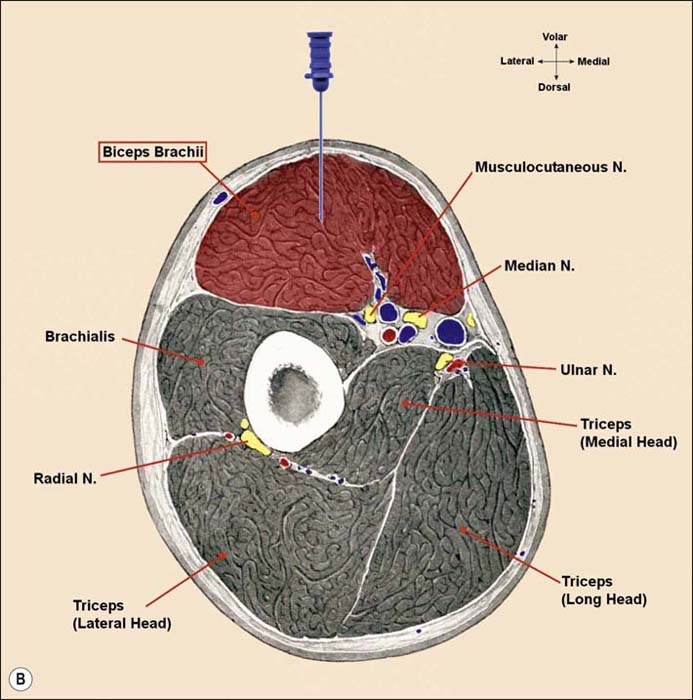
Biceps Brachii (BB) (Figure 13–21A,B)