Chapter 155 Anterior Approaches for Multilevel Cervical Spondylosis
Pathophysiology of Multilevel Cervical Spondylosis
Cervical radiculopathy and myelopathy are phenomena that are based on a compressive insult to the spinal cord and nerves. These can be either continuous or repetitive in nature. Degenerative phenomena, which ultimately result in the restriction of the spinal canal diameter and exit foramen narrowing, are part of a cascade that includes disc dehydration and loss of height with buckling of ligaments and periosteum and the formation of osteophytes and both bony and ligamentous hypertrophy. In addition, ossification of the posterior longitudinal ligament (OPLL) can occur. Although these processes are mainly responsible for a static compression and reduction of the canal, in cases where joint laxity predominates, varying degrees of listhesis during flexion-extension and rotation movements can lead to transitory compressions, which, in the long run, can lead to repetitive insults of the spinal cord long before becoming overt deformities. In the presence of significant osteophytes, the draping of the cord over these bony prominences with movement may account for a dynamic insult in the absence of instability.1–3
Myelopathy thus seems to develop from direct pressure insult. The hypothesis of hypoperfusion of the cord due to vascular compression, such as compression of the anterior spinal artery, seems appealing; however, no animal studies carried out on the topic seem to have confirmed the involvement of such a mechanism.4
Once myelopathic signs manifest, the history of CSM is characterized by progression.5,6 Only a minority of patients with myelopathic signs deteriorate rapidly. Given that the prognosis and postoperative outcome seem to correlate directly with the preoperative deficits and functional status, however, excessive waiting before proceeding with decompressive surgery does not appear to be justified as long as the general condition of the patient is favorable.7,8
Recently, the concept of origin of degenerative changes in spine has been speculated to be related to muscle weakness related facetal overriding.9,10 Facetal “retrolisthesis” could be a primary event rather than a secondary phenomenon. The pathologic events related to degeneration could be related to facetal overriding, rather than primary disc space reduction or loss of “water-content” of the disc. Facetal distraction, as proposed by Goel et al, has been successfully used as an alternative modality of treatment of single and multiple-level cervical and lumbar degeneration.11,12 The treatment has been identified to result in restoration of intervertebral distances and neural foraminal and spinal canal diameter. The treatment has been shown to result in increase of neural and spinal canal dimensions and restoration of disc space height and disc “water content”. Surgery is done without removal of any part of disc, bone, and ligament and aims at arthrodesis of the spinal segment.
Diagnosis
Clinical Features
The patient with multilevel cervical spondylosis (MCS) presents with a heterogeneous array of findings that show either polyradicular involvement or findings suggestive of cervical myelopathy. Difficulty in walking due to stiffness of the legs is a primary symptom that suggests myelopathy and, when present, can have diagnostic significance. Paresthesia and weakness of the limbs are dominant symptoms, but radiating pain in the hands can be less frequent. Long-standing dull pain at the nape of the neck is common. Apart from a thorough neurologic examination, the patient should also be examined and questioned for subtle signs that might not be identified in simple strength, sensation, and reflex assessments. Initial signs of myelopathy might be difficulty in fine finger movements such as buttoning a shirt or writing. These may not be accompanied by any other deficits and can thus be overlooked if the patient is not specifically asked about them. The “myelopathy hand,” which is characterized by sensory disturbances without any particular radicular distribution, clumsiness, and interosseous wasting, is also a warning sign in the absence of the possibility of peripheral polyneuropathy.13,14
Imaging Features
MRI is the best available imaging procedure for assessing the spinal cord and other soft-tissue structures, such as discs, ligaments, and capsules, that can be at the origin of compressive phenomena. It will also show compression of the spinal cord and nerves due to bony structures, but is less accurate in definition. Patients with impending or frank myelopathy due to compressive spondylosis show varying degrees of signal changes in the cord. These are hyperintense on T2-weighted images (T2WI) and hypointense on T1WI. Given that T2WI cord changes are more easily detected and appear earlier in the course of compressive myelopathy, MRI also has a prognostic value in that the finding of hypointensity on T1WI indicates a poorer prognosis when found preoperatively.15,16,
Computed tomography (CT) is the investigative modality of choice for the assessment of the bony spine. Although this is more relevant in trauma patients, where three-dimensional reconstructions on all planes show the exact relationships of the bony structures and potential fractures, it is not indispensable in most degenerative disease states. It can again be used in selected cases for assessment of bony conformation and osteophytes in particular, during preoperative planning, and postoperatively for the assessment of fusion and hardware position. When integrated with myelography, CT represents a good alternative to MRI if the latter is not available or feasible.17
Surgery for Multilevel Cervical Spondylosis
If appropriately selected, surgery for MCS is a very rewarding operation. Although the need for decompression of the cord from the osteophytic compression is necessary, the indication and methodology for fixation is a debated subject. Wide decompression of the cord by removal of the osteophytic bars should be the aim. The need to remove the vertebral bodies or to perform a corpectomy to remove the osteophytic bars is also a debated subject. However, the relative ease of performance of decompression by performing corpectomy has led several authors to recommend such an operative approach.
With the advent of anterior cervical spinal surgery after its original description by Smith and Robertson and Cloward over 50 years ago, the possibility of treatment solutions for the cervical spine have immensely expanded. It became possible to treat more complex pathologies from the front.18,19 Being able to access the anterior column of the cervical spine enables the surgeon not only to create a biodynamically sound construct in case anterior support is disrupted or lost but also to address a narrowed cervical spinal canal from the aspect where the majority of compressive phenomena originate, which is anteriorly.20 This is particularly true in the majority of cases of CSM, where anterior compression can be due to herniated discs, osteophytes of the posterior vertebral margins, or ossified posterior longitudinal ligaments (OPLLs). The anterior approach has therefore become the favorite route for removal of herniated cervical discs, relegating the posterior approach to the status of exception and feasible only in very selected cases or for simple foraminotomies.21,22
It is beyond the scope of this chapter to make a comparison in terms of efficacy and outcomes between anterior and posterior procedures for MCS. However, it should be mentioned that though no class I clinical trials have been conducted, the data derived from studies published in the literature on the topic seems to favor the anterior approach in the majority of cases.23–26 This seems to be attributable mainly to two facts: (1) As mentioned above, the majority of compression in MCS lies anteriorly in the spinal canal, and (2) the postlaminectomy membrane scars over the decompressed segments, leading to recompression and late deterioration after initial improvement.27 Laminoplasty techniques have been developed and have improved the outcomes achieved by using these procedures.28 Another problem is the kyphosing potential of multilevel laminectomy without fusion; however, this has been clearly established to be significant only in patients younger than 15 years.29,30
Techniques for Anterior Decompression in the Treatment of MCS
Anterior decompressive surgery for MCS can be divided into two groups: radical and conservative.
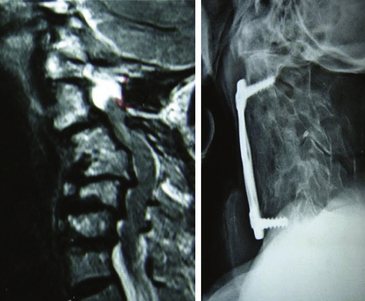
The radical surgical strategy entails maximum decompression with subsequent reconstruction by means of grafts and instrumented fusion. This can be done either by performing multilevel discectomies with extensive osteophytectomies or by performing corpectomies. Both procedures are widely used. The choice of the technique depends essentially on the individual case, the evaluation and experience of the surgeon, and his philosophical understanding. What the advocates of these techniques have in common is the belief that recreation of physiologic alignment and fusion of the operated segments are essential to providing a good long-term outcome (Fig. 155-1 and 155-2).
The following sections describe all these surgical techniques, together with their indications, advantages, and disadvantages. Common to all of them, apart from the oblique partial corpectomy according to George, is the exposure of the anterior cervical spine, which is discussed separately prior to the presentation of the individual techniques.
Exposure of the Anterior Cervical Spine
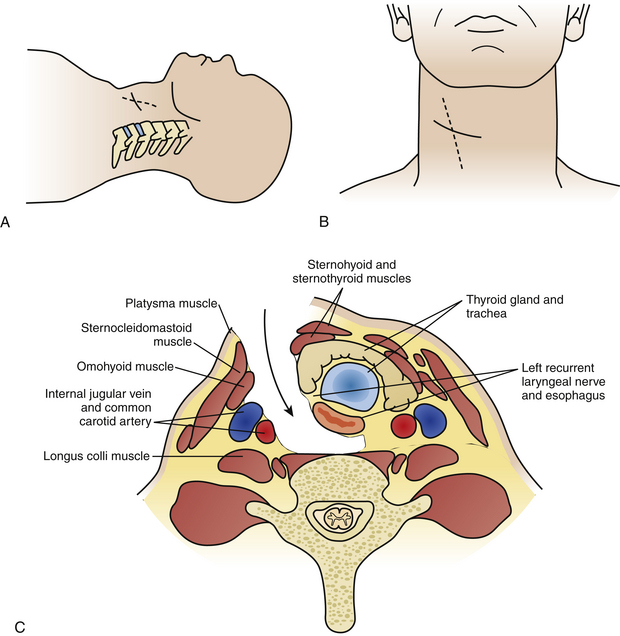
The incision on the chosen side of the neck is usually horizontal, either in a skin crease or along Langer’s lines. This can be as short as an inch, starting from the medial border of the sternocleidomastoid muscle (SCM) and extending medially for one-level procedures, and should be elongated in both directions when more spinal levels are to be exposed. Some surgeons prefer a vertically oblique incision that follows the medial border of the SCM, which has a cosmetically less favorable outcome and appears to be seldom necessary as long as some simple steps in the dissection procedure are observed (Fig. 155-3A, B).
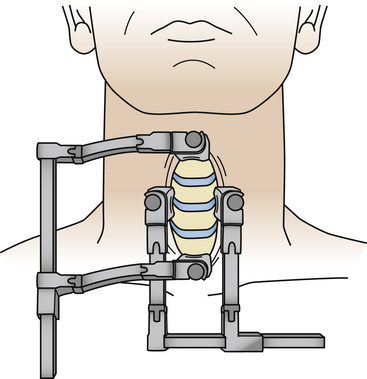
The next step is identification of the medial SCM border and opening of the investing fascia along the whole extent of the medial border with sharp dissection. Blunt finger or pledget dissection should now develop a plane reaching down, palpating the carotid artery, which generally is readily identified and left laterally. Thus the esophagus, larynx, and thyroid are left medially and the anterior aspect of the cervical spine is reached in one point (Fig. 155-3C). The retractor should be inserted underneath the longus colli muscles onto the vertebral body plane to avoid insertion and retraction between the esophagus and the trachea, as this is where the recurrent laryngeal nerve runs and can potentially be injured. A small aspect of the spine is thus exposed, and craniocaudal extension of the exposure is now necessary. This can be done by further blunt dissection, but for a long exposure sharp dissection often becomes necessary to divide the investing fascial layers. Care should be taken not to inadvertently cut the superior thyroid artery, which traverses at the C3 level, and the inferior thyroid artery, which traverses at the C7 level. They may be encountered especially in long exposures, but even then it is not frequently necessary to divide them.31 Should it become necessary, ligation of the vessel is advised prior to its division. The superior belly of the omohyoid will be encountered as a traversing structure during the development of a long craniocaudal plane, and a good dissection of this muscle usually permits its retraction either superiorly or inferiorly without the need to divide it. The prevertebral fascia is now divided and the longus colli muscles are lifted off the vertebral plane bilaterally to allow insertion of the self-retaining retractor blades. Craniocaudal retractor blades can be added for completion of the exposure (Fig. 155-4). Once the desired levels are thus exposed and confirmed by fluoroscopy, the decompressive procedure of choice can follow.
Complications and Pitfalls with the Exposure of the Anterior Cervical Spine
All complications inherent to the anterior approach are likely to be more pronounced in multilevel surgery because of the extent of the dissection and retraction. Recurrent laryngeal nerve injuries have been reported to make up about 17% of all neurologic injuries in anterior cervical surgery, with the majority being transitory.32 Injury to a recurrent nerve leads to paralysis of a vocal cord, with a hoarse voice and risk of aspiration. This risk is minimized by blunt dissection while avoiding excessive coagulation and overzealous retraction. Langenbeck retractors should be placed in contact with and exerting pressure on the vertebral plane much rather than in the tissues, and orthostatic retractor blades should be inserted under the longus colli muscles.33 When symptoms of hoarseness persist for more than 6 weeks, referral to an otolaryngologist should be made for assessment and evaluation of the vocal cords.34
Transient dysphagia has been reported to be as frequent as 8%,15 but injury to the esophagus is rare. If perforation of the esophagus occurs, however, it can be a life-threatening condition because of the high risk of infection, which can eventually lead to mediastinitis or vertebral osteomyelitis.35
Injury of the carotid artery and the jugular vein are uncommon and can be avoided by minimizing sharp dissection and the use of sharp-edged retractors. The other vessels that can be injured during the anterior approach are the superior and inferior thyroid arteries, which cross at C3 and C7, respectively. Careful extension of the dissection craniocaudally from the middle can quite easily identify the vessels and, if necessary, ligate and divide them. Injury of the vertebral artery is rare but has been reported to be as high as 3%.36
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree