33 Anterior Cervical Discectomy
I. Key Points
– Appreciation of the surgical anatomy of vital structures (carotid, esophagus, recurrent laryngeal nerve) during approach is essential.
– To decrease incidence and severity of dysphagia, endotracheal cuff pressure can be decreased during the retraction phase of the surgery. Additionally, intermittent relaxation of the retraction can be utilized.
II. Indications
– Symptomatic herniated nucleus pulposus
• Radiculopathy (after failed conservative therapy)
• Myelopathy
– Cervical spondylosis with radiculopathy or myelopathy
– Ossificationoftheposteriorlongitudinalligamentwithmyelopathy
– Cervical fracture with instability
III. Technique
– Place patient in supine position, arms tucked at sides.
• May use horseshoe headrest with weight strap (7 to 10 lb)
• May use foam doughnut head holder with shoulder retraction using thick tape
• Intravenous (IV) bag placed longitudinally between shoulder blades to provide mild head extension
– Localize with fluoroscopy or utilize landmarks (cricoid cartilage approximates C5-C6).
• If fluoroscopy is used, the incision is marked parallel to the disc space.
• If multilevel procedure is performed, favor the incision placement at the rostral disc space.
• A transverse incision 3 cm in length is adequate for single-level procedure; a longitudinal incision along the anterior border of the sternocleidomastoid is preferable for a procedure with three or more levels.
– Incision is made and the platysma undermined; the plane medial to the sternocleidomastoid muscle is identified and bluntly dissected with a finger or blunt instrument in a rostral-to-caudal direction (Fig. 33.1). The omohyoid muscle overlies the C6 level and can be divided.1
– The carotid is then palpated and the plane medial to the carotid and lateral to the trachea and esophagus is developed by blunt dissection in the rostral-to-caudal direction.
– The spine is then palpated, the prevertebral fascia is entered, and the disc level is confirmed by x-ray or fluoroscopy.
– Hand-held Cloward retractors are used to retract and provide protection medially (the trachea and esphogaus) and laterally (the carotid sheath), while the longus colli muscles are mobilized with Bovie electrocautery (Bovie Medical Corp., Clear-water, FL). The midline is marked on the vertebral body to facilitate alignment of the cervical plate.
– Self-retaining retractor (Trimline [Medtronic, Memphis, TN] or equivalent) is placed underneath the longus colli. The endotracheal tube cuff may be mildly depressurized at this point.
– Disc annulectomy is performed with a number 15 blade scalpel; additional disc removal is performed with a pituitary rongeur. The cartilaginous end plate is removed from the bony end plate with curettes. Carefully remove the lateral disc demarcated by the uncovertebral joint.
– Osteophytes/calcified disc fragments are drilled down to the posterior longitudinal ligament (PLL), the angle of drilling follows the angle of the disc space as seen with intraoperative radiographs or fluoroscopy. Take care not to drill away the bony end plate.
– The PLL is defined and first entered with a fine-angle nerve hook; it is identified by round longitudinal fibers. It is resected further with fine Kerrison punches. The dural plane is now evident.
– Allograft, autograft, or polyetheretherketone (PEEK)/carbon fiber cages filled with bone may be sized and placed into the disc space.2 Temporary sizers are introduced into the intervertebral space with head traction to assess the correct interbody spacer size.
– An anterior cervical plate is placed aligning the midline with previous mark.
– The wound is irrigated with saline (for non–bone morphogenic protein [BMP] cases).
– A small subfascial drain may be placed.
– Closure of platysma is done with interrupted 2.0 Vicryl (Ethicon, a Johnson & Johnson company, New York) and the subcutaneous layer with interrupted 3.0 Vicryl. Skin is closed with a subcuticular running 4.0 monocryl suture.
– Steri-strips (3M, St. Paul, MN) may be used for skin.
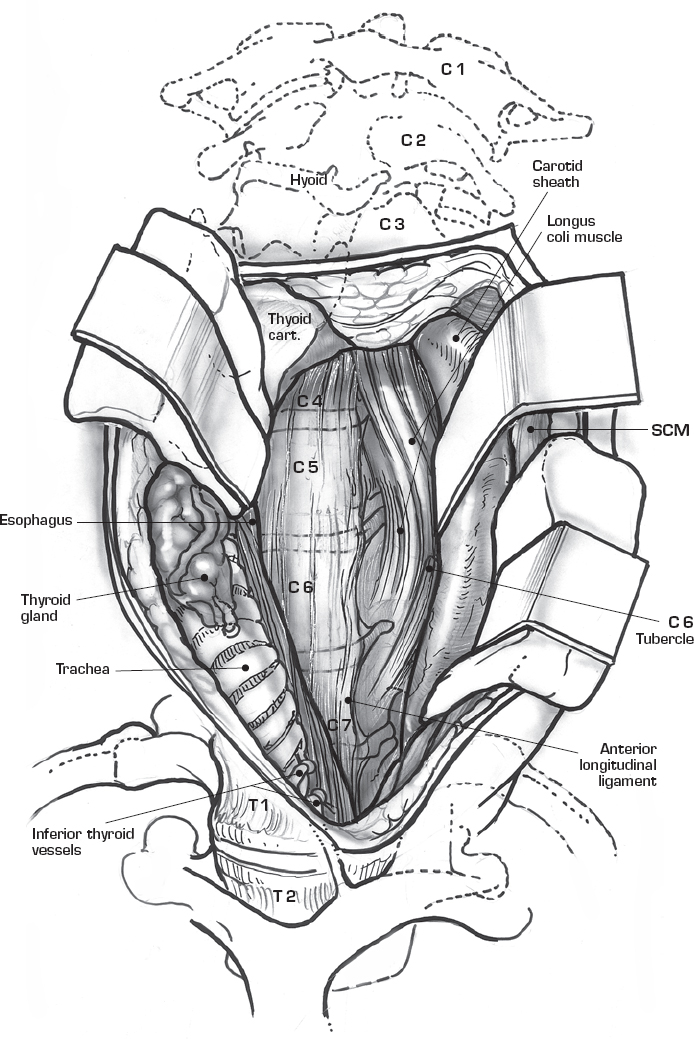
Fig. 33.1 Anterior exposure to cervical spine. (From Haher R, Merola A, Surgial Technique for the Spine, Thieme; pg. 73, Fig. 15-1B.)
IV. Complications
– Nerve root injury (C5 nerve root palsy in up to 5%)3
– Spinal cord injury (especially in myelopathic patients; avoid hyperextension)
– Wound hematoma (higher in multilevel cases; may be mitigated by drain placement)
– Hoarseness
– Dysphagia (due to edema or recurrent laryngeal nerve palsy)
– Esophageal perforation
– Carotid or vertebral artery injury (0.3%)
– Pseudarthrosis (2 to 20%)
V. Postoperative Care
– Decadron may be given for 24 hours to decrease soft-tissue edema.
– Use soft cervical collar for comfort (single level) and hard collar for immobilization (multilevel cases).
– Postoperative antibiotics for 24 hours
– May be discharged the same day with 6-hour observation in recovery unit
VI. Outcomes4
– Anterior cervical discectomy and fusion (ACDF) is a successful procedure when performed given the right indications.
– Adjacent-level disease occurs at a rate of around 2% per year in patients undergoing one-level ACDF.
VII. Surgical Pearls
– For patient counseling, ACDF is not fully effective in patients with predominant neck pain.
– The surgeon must know the course of the recurrent laryngeal nerve (RLN) to avoid injury during surgery. On the right, the RLN loops around the right subclavian artery, and the left RLN loops around the arch of the aorta. It runs within the tracheoesophageal groove, where sharp dissection in the paratracheal muscles or prolonged retraction against an inflated endotracheal tube may cause injury. Injury causes hoarseness, cough, aspiration, mass sensation, dysphagia, and vocal cord fatigue. Studies have not demonstrated a difference in RLN injury when comparing right and left anterior cervical exposure.
– Indirect decompression by removal of central disc material and restoration of disc space height by an interbody graft may be used for a laterally herniated disc; however, the definitive procedure is to remove all lateral disc demarcated by the uncovertebral joint. It is important to achieve a direct decompression of a laterally herniated disc.
Common Clinical Questions
1. What is the course of the recurrent laryngeal nerve, and what symptoms would be manifested by a recurrent laryngeal nerve injury?
2. What measures can be undertaken to minimize the risk of dysphagia in ACDF?
3. Destruction of vertebral body end plates during discectomy may cause:
A. Subsidence of interbody
B. Cervical kyphosis
C. Plate failure
D. Successful fusion
E. All of the above
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







