34 Anterior Cervical Foraminotomy
I. Key Points
– Spares disruption of the annulus fibrosus and avoids the need for interbody fusion
– Contraindicated in treating posterior pathology and centrally located anterior pathology
– Contraindicated in patients with evidence of instability
II. Indications
– Patients with cervical radiculopathy, myelopathy, or myeloradiculopathy
– Anterolateral pathology such as disc herniations or anterior osteophytes
– Lesions of the vertebral artery or foramen transversarium
– Progressive neurologic decline or failure of at least 3 months of conservative management
III. Technique
Operating Room Setup
– The operating room is set up in the same manner as for other anterior cervical approaches (e.g., anterior cervical discectomy and fusion [ACDF]).
– General endotracheal anesthesia is induced.
– The patient is placed supine with a shoulder roll to enhance cervical lordosis and access to the disc space. The patient’s arms are tucked at the sides and secured with appropriate padding to avoid ulnar nerve entrapment.
Exposure
– A transverse incision is made along a natural skin crease to avoid an aesthetically unacceptable scar.
– The subcutaneous tissues and platysma are carefully dissected until the strap muscles and carotid sheath are identified.
– The carotid sheath is retracted laterally and the esophagus and trachea retracted medially with Meyerding retractors.
– Fascial dissection is performed bluntly with a cotton-tipped probe.
– Prevertebral fascia is opened using either sharp dissection or monopolar cautery.
– Radiographic localization is performed to ensure exposure of the correct level.
– Meticulous hemostasis is maintained throughout the exposure.
– Self-retaining retractors are placed in the wound.
– An operating microscope is brought to the field.
Decompression
– The ipsilateral longus colli muscle is detached from vertebral body.
– The medial borders of the transverse processes of the superior and inferior vertebral body are exposed (Fig. 34.1).
– Uncovertebral joints are identified (Fig. 34.2).
– The inferior portion of the superior vertebral body constituting the uncovertebral joint is removed.
– Approximately 4 to 5 mm of the inferior vertebral body is removed.
– Bony removal continues until the posterior longitudinal ligament (PLL) is visible.
– Osteophytectomy or fragmentectomy is performed for full decompression of the impinged nerve root.
– A nerve hook may be used to ensure decompression.
Fig. 34.1 The area of interest between the superior and inferior vertebral body is outlined. Bony removal of the inferior border of the superior vertebral body is undertaken to reach the foramen.
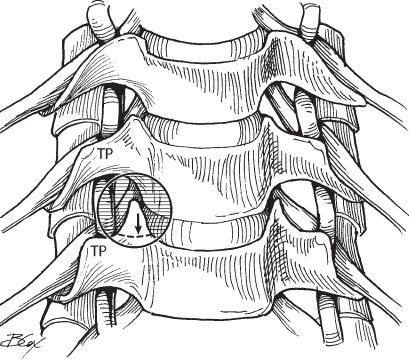
Fig. 34.2 Anterior exposure and approach for a patient with right C4-C5 foraminal stenosis. Arrow indicates the site of uncinate process take-down with 2 mm cutting burr (indicated by solid arrow within shaded circle). TP = transverse process. (From Vaccaro AR, Albert TJ, Spine Surgery: Tricks of the Trade 2nd ed, Thieme; pg. 55, Fig. 15.1.)
IV. Complications
– With the procedure in experienced hands, the complication rate has been reported at <5%.1–3
– Nerve root injury
– Spinal cord injury
– Cerebrospinal fluid (CSF) leak
– Recurrent laryngeal nerve injury
– Tracheal or esophageal injury
– Vascular injury (carotid artery, jugular vein, vertebral artery) (Fig. 34.3)
– Horner syndrome (sympathetic trunk injury)
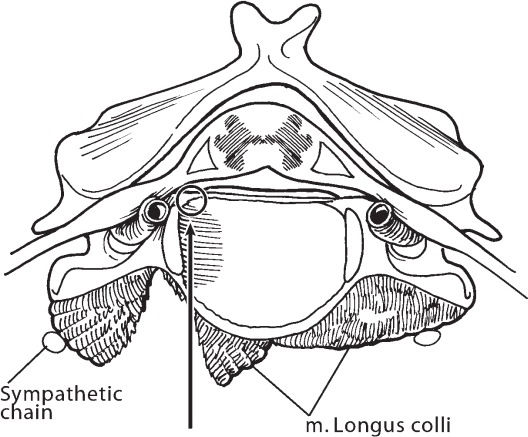
Fig. 34.3 Axial view of a vertebral body demonstrating approach for anterior foraminotomy. Operative approach includes drilling down through uncinate process to start point of foraminotomy. Special attention must always be paid to the nearby vertebral artery. (From Vaccaro AR, Albert TJ, Spine Surgery: Tricks of the Trade 2nd ed, Thieme; pg. 55, Fig. 15.2.)
V. Postoperative Care
– May be outpatient procedure or involve overnight observation
– A soft collar may be employed for comfort measures immediately after surgery, but patient should be weaned off and discontinue use shortly thereafter.
– Throat lozenges can be used to treat postoperative swallowing discomfort from esophageal irritation.
VI. Outcomes
– Jho and colleagues reported 79.8% resolution of symptoms in patients with radiculopathy.2
– For myelopathy, 27.5% experienced resolution of all symptoms, 52% showed improvement, and 20% were unchanged.1
VII. Surgical Pearls
– Proper setup and retractor placement is crucial to maximize visualization and prevent complications.
– Knowledge of the course of the vertebral artery is essential to prevent vascular injury.
– This approach is ideal for pathology located anterolateral to the neural elements.
– Minimal destabilization avoids the need for concomitant fusion.
Common Clinical Questions
1. The anterior foraminotomy may be utilized to address what type of pathology?
2. True or false: An arthrodesis procedure is necessary following anterior foraminotomy.
3. True or false: Outcomes for this operation are better for radiculopathy than for myelopathy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







