Chapter 152 Anterior Cervical Foraminotomy (Jho Procedure)
Microscopic or Endoscopic
The optimal surgical treatment of degenerative cervical spine disease that involves radiculopathy and/or myelopathy is the direct surgical removal of compressive pathology while preserving segmental motion. Historically, current cervical spine surgical techniques were introduced more than a half century ago as anterior approach (anterior cervical discectomy) and posterior approach decompression procedures. Although anterior cervical discectomy directly targets the compressive pathology, which usually consists of soft disc herniation or spondylotic stenosis, the approach also involves removing structural elements important for segmental motion—such as the anterior longitudinal ligament and nonherniated portions of the disc—for the sake of surgical exposure. In comparison, some posterior decompression techniques can preserve segmental motion, but in many cases they do not target the compressive pathology directly. To optimize the two surgical goals of directly removing compressive pathology while maximizing the preservation of segmental motion, anterior cervical foraminotomy techniques were developed and previously reported by the senior author as the “Jho procedure.”1,2
The Jho procedure was developed to overcome the deficits of classic anterior and posterior cervical procedures in selected patients to optimize the achievement of surgical goals. Microsurgical anterior cervical foraminotomy was first reported by H.D. Jho in 1996 under the minimally invasive concept of functional spine surgery, in which compressive pathology is directly removed via an anterior approach while the remaining disc and functioning motion unit is preserved without the use of implants or bone fusion.1 The originally reported technique for anterior cervical foraminotomy involved removing the uncovertebral juncture (the most lateral part of the intervertebral disc) to access the compressive pathology. Once the surgical access is made, the soft disc and/or bone spurs that compose the compressive pathology are excised. This surgical approach directly addresses the compressive pathology with access via the lateral portion of the spinal column and effective preservation of the anatomic structures so that segmental motion remains intact and bony fusion is not necessary.
Originally, the Jho procedure was performed under the operating microscope; hence the surgery was also called anterior cervical microforaminotomy.2 Several variations of the surgical technique gradually evolved to achieve surgical goals more efficiently while minimizing surgical impact to the spinal column and functioning motion unit. Because no precise terminology currently prevails to describe the evolution of surgical techniques, the term surgiology was coined to represent the progressive pursuit of scientific or artistic knowledge to improve a particular operative treatment. The loose derivation of this term is from roots defined by the Webster’s dictionary with “surgery” being “a) the treatment of disease, injury, or deformity by manual or instrumental operations, as the removal of diseased parts or tissue by cutting, b) an operation of this kind, c) the branch of medicine dealing with this” and the suffix “-ology” as “the science, doctrine, or theory of” something. Surgiology has historically been an inherent process with the tendency to result in the eventual elimination of ineffective surgeries and the improvement of effective techniques. The Jho procedure involving anterior cervical foraminotomy therefore underwent surgiologic refinement to result in four basic variations and use of the endoscope.
Further variations on this technique evolved from the concept that the trajectory from the skin incision to the surgical target in the sagittal plane of the cervical spine directs where a bone opening should be made to access the target pathology efficiently and effectively. Thus, surgical technique became tailored depending on the trajectory, as determined by the nature of the pathology and cervical anatomy. The surgiologic result was the progressive development of the following variations: 1) transuncal approach; 2) upper-vertebral transcorporeal approach; 3) lower-vertebral transcorporeal approach; and 4) anterior cervical foraminoplasty.3
Surgical Tools and Techniques
Endoscopes
The endoscopes we use are rod-lens endoscopes that are 4 mm in diameter and 18 cm in length. One set consists of five endoscopes: a 0-degree-lens endoscope, 30-degree lens angled toward the light source, 30-degree lens angled away from the light source, 70-degree lens angled toward the light source, and 70-degree lens angled away from the light source (Fig. 152-1) The 0-degree-lens endoscope is the basic working configuration used for most applications. Because the endoscope provides a wide-angle view, the 0-degree-lens endoscope usually provides adequate views for exposure at the nerve root as well as the spinal cord. However, the 30-degree-lens endoscope angled toward the light source can be used when a more-angled view toward the spinal cord is desired, and a 30-degree-lens endoscope angled away from the light source can be used when a more-angled view toward the nerve root at the neural foramen is desired.
Endoscope Lens-Cleaner
An endoscopic lens-cleansing device is required to keep the lens clear so that the surgeon can continually operate without interruption (Fig. 152-2). The device consists of a disposable irrigation tube that passes through an electric-powered motor. The endoscope is placed through a rigid tubular irrigating sheath, which is connected to the irrigating tube. The irrigation tube is connected to a saline bag, which is hung on a pole. This motor-powered irrigation device is controlled by a foot pedal to flush saline forward. When the foot pedal is released, the motor reverses its rotary direction and draws the saline back from the tip of an endoscope for 1 to 2 seconds. The forward flow of irrigating saline cleans the lens, and the reverse flow clears away water bubbles at the tip of the endoscope. Although this device is not yet ideal, it helps the surgeon significantly in the task of keeping the endoscope lens clean without removing the endoscope from the surgical site.
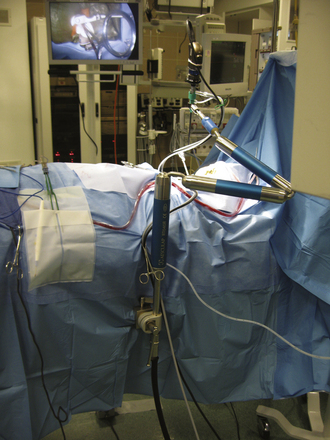
Endoscope Holder
Two different types of endoscope holders are available, but both are not yet ideal. One is a simple manual holder with multiple joints that can be tightened by hand, and the other is a holder with joints powered by nitrogen gas and controlled with a single button. Manual holders are inconvenient to maneuver with releasing, repositioning, and tightening; they also have limitations in flexibility for reaching certain positions. Nitrogen gas–powered devices are more expedient than manual types but are not as smooth as the operating microscope in releasing and locking at various positions. Currently, we use a Mitaka endoscope holder (distributed by Karl Stortz) for cranial applications and an Aesculap holder for spine applications (Fig. 152-3). The Mitaka holder is relatively bulky at the attachment shaft and has very narrow accessibility at the holding terminal; thus the endoscope holding terminal has to be appropriately positioned at the surgical area before tightening at the shaft joints. Because the holding terminal maneuverability of the Mitaka holder is superior to Aesculap, we like to use the Mitaka holder for cranial endoscopic surgery. The Aesculap holder has longer flexible arms compared to the Mitaka, but its holding terminal has a limited range of motion, even with custom modifications. We prefer to use the Aesculap holder for spine endoscopy, but holding terminals of both types of holders are not yet ideal for endoscopic spine surgery. Sagging of a few millimeters after release of the powerbutton is another suboptimal feature of the nitrogen-powered holders.
Endoscopic Surgical Instruments
Because the region of bone removal in anterior cervical foraminotomy requires high precision, a fine drilling device is required. We use a Midas telescoping tubular drill with a 2-mm diamond bit. The drill bit tip can be progressively extended as the depth of drilling advances. Other commercial drill products are available that have comparable systems. Bipolar forceps are shaped to accommodate the endoscopic surgical environment, and the blades of the bipolar forceps are parallel to each other, similar to a single-bladed instrument, once the blades are approximated. Various surgical curettes and other endoscopic instruments were customized and developed in order to function efficiently within the uniquely curved endoscopic surgical trajectory.
Surgical Technique
Surgical Exposure of the Uncovertebral Juncture
By palpating the transverse tubercles, the extent of the longus colli is identified. The longus colli is split just medial to the transverse tubercles rostral and caudal to the intervertebral disc level, being careful to avoid injury to the sympathetic trunk and fibers located laterally along the longus colli. A cervical retractor system is applied between the split longus colli muscle fibers to maintain exposure of the uncovertebral juncture. The original description mentioned sectioning of the medial part of the longus colli muscle, but this soon evolved to splitting the longus colli muscle, allowing its preservation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree