56 Anterior Lumbar Interbody Fusion (ALIF)
I. Key Points
– Anterior lumbar interbody fusion (ALIF) offers several potential advantages over other surgical approaches.
• The ability to perform a complete or subtotal discectomy
• Large surface area for fusion and structural grafting
• Favorable fusion environment (compression)
• Effective for anterior releases, particularly in the setting of high-grade deformity
• Posterior muscle sparing
• Indirect foraminal decompression
II. Indications
– Spondylolisthesis (typically grade I or II)
– Degenerative disc disease causing mechanical low back pain
– Postdiscectomy collapse with neural foraminal stenosis
– Treatment of posterior pseudarthrosis
– Treatment of post-laminectomy kyphosis
– Treatment of coronal and/or sagittal imbalance
III. Technique
– Place the patient supine on a regular operating table or a flat Jackson table.
– A bump under the sacrum will allow for increased lumbar lordosis.
– Slight Trendelenburg position will allow the abdominal contents to displace cephalad away from the surgical field.
– The operative level is identified with lateral fluoroscopy. This localizes the skin incision (critical for mini-ALIF approaches).
– A left transverse or longitudinal paramedian incision is made.
– The anterior rectus sheath is identified and divided in line with the skin incision.
– Blunt dissection is used to mobilize the rectus and to identify its lateral border.
– The lateral edge of the rectus abdominis muscle is retracted toward the midline, exposing the posterior rectus sheath (above the arcuate line) or, less commonly, the arcuate line and the preperitoneal space (below the arcuate line).
– The posterior rectus sheath–arcuate line is carefully divided in a superior-to-inferior direction and the preperitoneal space identified.
– Using blunt dissection, the peritoneum is mobilized off of the anterior and lateral abdominal wall and retroperitoneal blunt dissection is used to identify the psoas muscle.
– Hand-held retractors are advanced.
– The ureter, peritoneum, and abdominal contents are mobilized across the midline.
– The psoas muscle is released and then retracted laterally, allowing direct visualization into the disc space.
– With blunt dissection medial to the psoas muscle, the index disc space is identified and confirmed with a marker and fluoroscopy.
– Retractors are placed around the lateral annulus, first on the right side, retracting the abdominal contents and the iliac vein (Fig. 56.1).
– Once the disc space is confirmed, an annulotomy is made with either a knife or electrocautery.
– A Cobb elevator and curette are used to remove the cartilaginous end plates, carefully preserving the subchondral bone/end plate.
– Pituitary rongeurs are used to remove the disc fragments.
– An interbody graft (allograft, titanium, or polyetheretherketone [PEEK]) is appropriately sized to gently distract the disc space and contact the ring apophysis.
– The anterior rectus sheath is closed with nonabsorbable sheath. The posterior sheath does not require repair.
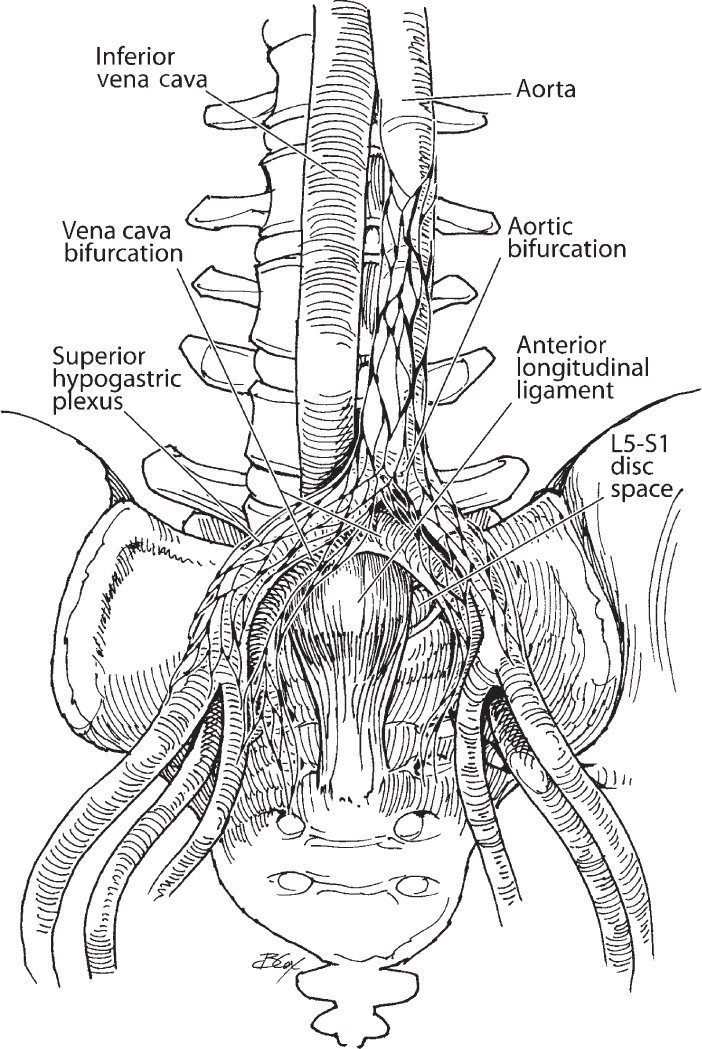
Fig. 56.1 Key anterior retroperitoneal structures.
– Iliac vein injury
– Ileus
– Retrograde ejaculation occurs secondary to injury to the superior hypogastric plexus (sympathetic chain). The superior hypogastric plexus provides innervation to the internal vesical sphincter. The reported incidence of retrograde ejaculation after ALIF varies widely in the literature, ranging from 0.4 to 5.9% of male patients.3,4
– Ureteral injury
– Deep vein thrombosis
– Abdominal hernia
– Rectus muscle paresis
V. Postoperative Care
– Patients are mobilized on the first postoperative day.
– Diet is advanced as tolerated starting on the first postoperative day.
– Discharge to home when patient meets discharge criteria (typically, ambulating, tolerating a diet, voiding, and adequate pain control on oral medications).
VI. Outcomes
– Satisfactory clinical outcomes can be anticipated in 70% of patients.5
– Fusion rates vary from 85 to 95% in most series and depend on whether autograft or bone morphogenetic protein (BMP) is used.6
– Interbody subsidence is an expected phenomenon and occurs in as many as 85% of cases, particularly stand-alone grafts.7
VII. Surgical Pearls
– Localize with fluoroscopy prior to making a skin incision.
– Trendelenburg position allows the abdominal contents to move cephalad out of the operative field. This position also decreases venous bleeding.
– Avoid the use of monopolar cautery around the sympathetic chain prior to the annulotomy.
– Take care not to violate the subchondral end plates.
Common Clinical Questions
1. What is retrograde ejaculation and how can the risk be minimized?
2. At what level does the aorta bifurcate, and why is that important for anterior spinal procedures?
3. List four indications for anterior lumbar interbody fusion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







