Chapter 176 Atlantoaxial Instability and Stabilization
The atlantoaxial junction is a delicate anatomic complex that involves an intricate relationship between the atlas and the axis to allow flexion, extension, rotation, and lateral bending.1 The interrelation of osseous, ligamentous, neural elements, and articulations make the atlantoaxial junction vulnerable to instability and potentially devastating neurologic complications. A myriad of surgical treatment options exist, ranging from fixation with and without dorsal surgical fusion and/or internal fixation using screw techniques and/or wiring techniques. This chapter reviews the different atlantoaxial fixation techniques, including their indications, limitations, and complications.
Anatomic Considerations in Treating C1 and C2 Injuries
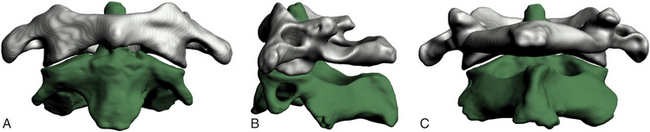
The atlas supports the globe of the head and has very unique anatomic characteristics that separate it from other vertebrae. It is essentially a bony ring without a body consisting of an anterior arch as well as two lateral masses connected to a posterior arch by two pedicles (Fig. 176-1). The longus colli muscles attach to the anterior arch via a small bony prominence, the anterior tubercle, which is a rudimentary vertebral body. The posterior aspect of the anterior arch has an indentation, the fovea dentis, to serve to accommodate the odontoid process of C2. The posterior arch joins together to form the posterior tubercle over the posterior midline. It is the attachment point for the posterior atlanto-occipital membrane and the rectus capitis posterior minor muscles. The upper aspect of the posterior arch contains the vertebral arteries within the sulcus arteriae vertebralis. The vertebral arteries travel within the sulcus medially before ascending to penetrate the dura. The lateral masses have large, concave superior surfaces to articulate with the occipital condyles. They are directed upward, medially, and backward and form a cup for the corresponding condyle. The inferior surfaces are circular and directed downward and medially to articulate with the superior articulating facet of C2 and form the zygapophyseal joints, which allows flexion-extension, side-bending, and rotational movements. The atlantoaxial joint is the articulation between C1 and C2 and has a range of motion in the transverse plane for rotation. This rotation is facilitated by the odontoid process, which acts as a pivot point for the rotation of C1. The transverse processes project farther laterally than the transverse processes on the adjacent cervical vertebrae. The apex of the transverse process can be felt through the skin between the mastoid process and the angle of the mandible.2 Several muscles attach to it. The superior obliques arise from the upper surface of the transverse process and extend to the occiput, and the levator scapulae, splenius cervicis, and the scalenus medius attach to the inferior and lateral surfaces of the transverse process. The inferior obliques extend from the inferior surface of the transverse processes to the spinous process of C2. The transverse processes also contain the transverse foramina. The atlantoaxial articulation is composed of three synovial joints: the paired lateral mass articulations and the central articulation between the dens and the anterior arch of C1 and the transverse ligament. The transverse ligament attaches just below the medial margin of each superior facet, stretching across the atlantal ring and dividing the vertebral foramen into an anterior part, which receives the dens, and a posterior part, which transmits the spinal cord. The transverse ligament is the major stabilizer at the C1-C2 level. The cruciform ligament consists of the superior and inferior longitudinal fasciculi, which extend to insert into the anterior foramen magnum and the posterior body of the axis, respectively. Other important ligaments include the anterior atlantoaxial ligament, which extends caudally to form the anterior longitudinal ligament in the subaxial spine; the posterior atlantoaxial ligament, which extends caudally to form the ligamentum flavum; the apical ligament, which connects the tip of the dens to the foramen magnum; and the alar ligaments, which extend from the lateral dens to attach to the occipital condyles.
Indications for Fixation
The indications for fixation are described in the following subsections.
Trauma
Because of the fragile nature of the bony and ligamentous components of the upper cervical spine, injuries to this region are common. The mechanisms of injury include flexion, extension, or compressive forces applied to the head during motor vehicle accidents, falls, or sports-related injuries. Trauma to the atlantoaxial complex can lead to significant instability and may require surgical fixation. Fractures of the dens are common injuries requiring fixation. In some cases, these fractures can be treated using an anterior approach, thus sparing motion; in other circumstances, a posterior approach may be indicated.
Odontoid Fractures
Classification
The most widely accepted classification for odontoid fractures is the Anderson and D’Alonzo classification, which is based on the fracture line.3 The criteria for the treatment algorithms for these types of fractures pertain to the fracture line, the amount of displacement, and a concurrent ligamentous injury. It is therefore imperative to perform computed tomography (CT) and MRI for evaluation. Type I is a stable avulsion fracture that involves the tip of the dens and, in general, leaves the ligamentous complex intact. Treatment involves the use of a cervical collar and symptomatic relief. However, it is imperative to evaluate the craniocervical junction with a flexion-extension dynamic study to rule out concomitant ligamentous injury and instability. Type II odontoid fractures are inherently unstable and occur at the junction of the C2 vertebral body and the dens. The treatment options and their union rate vary with the amount of displacement: With less than 6 mm displacement, external halo fixation carries a 93% union rate4; with 6 mm or more displacement or with comminuted fragments of the base of the dens (type IIa), the disunion rate is as high as 75% to 85% and internal fixation needs to be considered.4,5 Type II odontoid fractures can also lead to transverse ligament injury.6 The integrity of the transverse ligament is essential in making the decision to use anterior odontoid screw fixation. If the ligament is intact, one can proceed with odontoid screw fixation; otherwise, a C1-C2 fixation is necessary. The techniques for C1-C2 fusion and for anterior odontoid screw fixation are discussed below. Type III odontoid fractures extend into the cancellous portion of the C2 vertebral body. They are considered unstable fractures and are treated by reduction with skeletal traction as needed and immobilization with a collar or halo. Surgery is indicated if there is persistent disunion after 12 weeks of orthosis use.
Traumatic Spondylolisthesis of the Axis (Hangman’s Fracture)
Traumatic spondylolisthesis of the axis was first described in convicts who were hanged, hence its nickname, Hangman’s fracture. When the convict fell into the rope, the neck was distracted and hyperextended, resulting in rupture of the C2-C3 disc and fracture of C2. Hangman’s fractures account for approximately 7% of all cervical fractures. Today the most common cause of traumatic spondylolisthesis of the axis is a hyperextension-compression injury. This explains the fact that patients who sustain these fractures seldom have neurologic complications. Hangman’s fractures cross the pars interarticularis of C2 and are classified by Effendi et al7 into three types: Type I Hangman’s fractures account for 65% of all traumatic spondylolistheses and consist of a stable, nondislocated fracture with intact C2-C3 disc space, type II involves a ruptured C2-C3 disc with dislocation of the C2, and C2-C3 is unstable. It account for 28% of traumatic spondylolisthesis, and type III adds a unilateral C2-C3 dislocation to the type II definition.
Fractures of the Atlas
Atlas fractures account for approximately 2% to 13% of all cervical spinal injuries and are classified according to Gehweiler and colleagues8 as follows:
• Type I: isolated fracture of the anterior arch of C1
• Type II: isolated fracture of the posterior arch of C1
• Type III: combined anterior-posterior fracture (Jefferson fracture)
• Type IV: isolated lateral mass fracture
Type I fracture is a horizontal avulsion injury of the caudal portion of the anterior arch due to the contraction of the longus colli during hyperextension. Hence the circumferential integrity of the atlas is maintained, and treatment involves symptomatic relief and a collar. With concomitant dens dislocation, the fracture can become unstable, and the algorithm follows that of an odontoid fracture. In type II injuries, the fracture is located in the weakest part of the posterior arch, usually at the sulcus arteriae vertebralis, and it is bilateral. It is a hyperextension and axial loading injury that is usually not accompanied by neurologic deficit, since the osseous structures are pushed outward. A concomitant dens fracture needs to be excluded during the differential diagnosis and treatment is symptomatic. Type III injury, or Jefferson fracture, was first described by Jefferson in the 1920s.9,10 It involves both the anterior and the posterior arch of C1 and can include unilateral and/or bilateral fractures on either arch. Type III is an axial loading injury with lateral displacement of the fragments that can include a concurrent avulsion injury of the transverse ligament. The latter renders a Jefferson fracture unstable. It is therefore imperative to exclude injury of the transverse ligament on the basis of radiographic evidence of a Jefferson fracture. Spence’s rule assumes a rupture of the transverse ligament if the step-off of the lateral masses confirmed by a transoral open-mouth view or by coronal reconstructive CT is at least 7 mm. If the sum is less than 7 mm, a flexion-extension study can be obtained to rule out underlying instability. Types IV and V fractures are rare, stable fractures requiring symptomatic treatment. With transverse process fractures, there is a risk of thrombosis of the vertebral artery. Obtaining an arteriogram may become necessary if there are clinical signs of vertebral artery thrombosis. Patients with all of these injuries need to have follow-up flexion-extension examinations to rule out ligamentous laxity after the fractures have healed.
Isolated Transverse Ligament Injury
Traditionally, Spence’s rule is applied to identify a transverse ligament injury radiographically. More recently, some authors have indicated that MRI is a more sensitive indicator of transverse ligament injury than Spence’s rule.6,11,12 Dickman et al11 classified isolated transverse ligament injuries into two different types based on MRI: type I is an injury of the transverse ligament without concurrent atlantal fracture, and type II involves an avulsion fracture at the insertion of the ligament into the medial aspect of the arch. In their series of 39 patients with axial and atlantal fractures, they concluded that use of Spence’s rule would have missed 60% of transverse ligament injuries (as determined by MRI). They suggested that type I transverse ligament injuries need to be treated with early surgery and favor external halo immobilization for type II fractures.12
Ligamentous Injury
Flexion of the upper cervical spine can lead to ligamentous injuries and subsequent laxity without bony injury. A value greater or equal to 5 mm for the anterior atlantodental interval in adults (normal value, 2 to 4 mm in adults and 7 mm in adult patients with Down syndrome) indicates ligamentous laxity, and a value greater than 10 to 12 mm indicates complete ligamentous destruction.13 Axial rotation of the upper cervical spine is limited by the alar ligaments, and damage to these ligaments increases rotation on the contralateral side by 30%.14 Failure of any of the components of the atlantoaxial ligament complex requires dorsal surgical fusion.
Rheumatoid Arthritis
Rheumatoid arthritis (RA) is a systemic disease that can affect the atlantoaxial junction and subaxial vertebrae. Eighty-eight percent of RA patients have involvement of the C1-C2 junction.15 As many as half of patients with RA develop symptomatic atlantoaxial subluxation, 56% of whom have myelopathy.16 Postmortem examinations have indicated C1-C2 instability as the cause of death in as many as 10% of patients.17 Classic radiographic findings include the staircase phenomenon, which is due to multiple subluxations involving the atlantoaxial and subaxial joints. In general, the following are indications for surgical intervention: spinal cord compression, severe neck symptoms, and marked subluxation. Any combination of two of the following factors also warrants surgery: cervical myelopathy, delayed central motor latency, spinal cord diameter less than 6 mm in a neutral or flexed position observed on an MRI study or less than 10 mm upon flexion, pannus more than 10 mm behind the dens, and anterior atlantodental distance more than 10 mm. Some authors advocate surgical intervention if the posterior atlantodental interval is less than or equal to 14 mm, even without neurologic symptoms.18
Congenital Abnormalities
Any congenital abnormality that prevents optimal development of the osseous (dens) and/or ligamentous structures (cruciate ligament) can lead to atlantoaxial instability. Os odontoideum is a failure of the dens to fuse with the body of the axis and, together with odontoid agenesis, can lead to ligamentous laxity or underdevelopment and hence instability, requiring surgical intervention.19,20
OS Odontoideum
Os odontoideum is an ossicle with smooth circumferential cortical margins that represent the dens without osseous continuity with the body of C2.21,22 The etiology of this entity remains disputed (acquired vs. congenital), but the etiology is of no importance in the treatment algorithms.20 Os odontoideum can be classified as orthotopic and dystrophic. The former defines an ossicle that moves with the anterior arch of C1 and can sublux anterior to the arch,23 and the latter describes an ossicle that is fused to the basion. The natural history of os odontoideum is variable, and no predictive factors for a clinical scenario have been identified. Surgical treatment of os odontoideum correlates with the presence or absence of C1-C2 instability. Patients without neurologic deficits and without C1-C2 instability on flexion-extension can be managed conservatively. Although some patients with instability have been treated nonoperatively, most surgeons advocate operative stabilization and C1-C2 fusion. The concern is that with this constellation there is a higher risk of future spinal cord injury, and several studies have indicated that surgery has merit.24–27 Furthermore, longitudinal radiographic and clinical surveillance is recommended for all conservatively treated patients.23 Screw fixation techniques have the advantage that no postoperative external fixation is required. The last category of etiologies that can lead to instability of the atlantoaxial junction includes infectious and neoplastic processes affecting the C1-C2 junction.
Dorsal Wiring Techniques
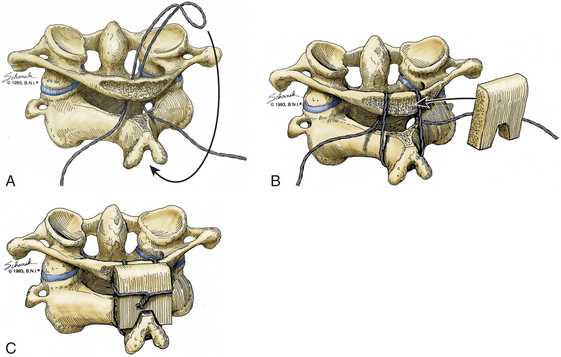
Gallie Fusion
Initially described in 1939, the Gallie dorsal wiring fusion technique is a simple surgical fixation method (Fig. 176-2).28 It consists of placement of a medial bone graft between the posterior arch of C1 and the spinous process of C2, with sublaminar wiring around the arch of C1 and looping around the C2 spinous process. For the sublaminar placement of the wire, a 1.2-mm wire is looped into a hook configuration and passed from the inferior aspect of posterior arch of C1 ventrally to the arch of C1 and over the posterior aspect of the arch of C1. Attention should be paid so that no injury to the spinal cord occurs during that process. The loop is then pulled caudally enough to hook it over the spinous process of C2. The arch of C1 and the lamina of C2 are decorticated, and a bone graft in an H configuration is placed over the decorticated area and fixated with the two lateral ends of the wire. The area around the bone graft can then be packed with more cancellous bone. This technique is the simplest and poorest form of biomechanical stabilization. It requires an intact C1 arch, and as such it cannot be used to treat Jefferson fractures or any entities with involvement of the posterior arch of C1, such as infections, tumors, and rheumatoid arthritis. It offers minimal rotational stability and requires postoperative external immobilization.29 Its disunion rate is rather high at 25%, and this technique is most often used to supplement other stabilization methods.30
Brooks-Jenkins Fusion
For the Brooks-Jenkins wiring technique,31 the laminae of C1 and C2 are dissected and two 20-gauge wires are passed under the lamina bilaterally (Fig. 176-3). Two bone grafts are then placed into the lateral interlaminar space on each side, held in place by the wires. As compared to the Gallie technique, this technique allows more rotational stability with higher fusion success rates of up to 93% with the use of a halo postoperatively. This technique has the same contraindication as the Gallie technique and requires an intact C1 posterior arch. In addition, the passage of two wires can result in wider curvature and a “clothesline” compression of the spinal cord.32
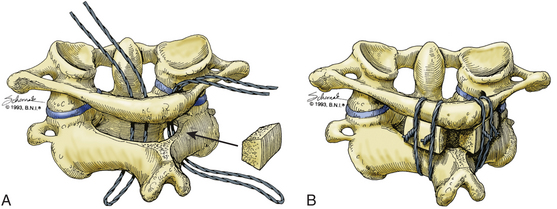
Sonntag’s Modified Gallie Fusion
Sonntag and colleagues33 introduced the modified Gallie dorsal wiring fusion technique to provide more stability than the classic Gallie technique. The intralaminar space between C1 and C2 is widened by using a high-speed drill, and a single bicortical graft is fitted into that space. The lamina and the spinous process of C2 are decorticated, and two 24-gauge sublaminar wires are passed around the posterior arch of C1, over the graft, and around the spinous process of the axis. Like the Gallie technique, the Sonntag technique requires an intact posterior arch. Another disadvantage of the Sonntag technique is the postoperative need for external fixation. The halo will be used for 3 months after surgery, and subsequently the patients need to be in a hard collar for 4 to 6 weeks.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree