CHAPTER 314 Atlantoaxial Rotatory Subluxation, Transverse Ligament Injury
The atlantoaxial joint is one of the most active joints in the body, and increased mobility of this joint causes some interesting problems with stability. Atlantoaxial rotatory subluxation (AARS) refers to a number of pathologic processes in which increased rotational instability of the C1-2 joint causes disarticulation of the facets and translational subluxation. AARS is relatively rare in adults but somewhat more common in children, albeit by a largely different mechanism of action. In pediatrics, the term atlantoaxial fixation refers to subluxation in which the facets become locked, thus making the deformity largely irreducible.1,2 In adults, the condition is almost exclusively due to trauma, whereas in children it may be the result of inflammatory diseases or congenital laxity of the transverse ligament. The lethality of atlantoaxial injuries is often discussed, but the true incidence is unknown. It is possible that the relative paucity of literature regarding atlantoaxial subluxation in adult trauma reflects this lethality. The close proximity of the medulla and vertebral arteries makes potentially fatal injuries seem relatively likely. The presence and duration of neurological symptoms vary greatly. Treatment of AARS is largely dependent on the age of the patient, etiology of the instability, radiographic classification, and the presence or absence of neurological symptoms.
Anatomy and Biomechanics of The Atlantoaxial Joint
The atlantoaxial joint is one of the most mobile joints in the human body and is estimated to move an average of 600 times per hour.3 Unfortunately, with the gain of a greater range and frequency of motion, a joint must sacrifice some inherent stability, and this predisposes the atlantoaxial joint to injury. The normal rotational motion of the cervical spine is approximately 90 degrees to either side, and nearly 60% of this rotation occurs at the atlantoaxial joint.4,5 The facet joints at C1-2 are almost horizontal, which allows excellent axial rotation with the sacrifice of bony translational stability. The joint is largely stabilized by two sets of ligamentous structures, the transverse ligament and the alar ligaments. The transverse ligament is a rather large web-like structure that courses immediately posterior to the dens. When intact, this prevents excessive translation of the atlas on the axis. The paired alar ligaments run from the lateral surface of the tip of the odontoid process to the occipital condyles and serve to limit rotation of the atlas on the axis. The alar ligaments act as secondary translational stabilizers in addition to the transverse ligament. When the transverse ligament is cut in cadaver studies, anterior translation of around 4 mm occurs.6 When the alar ligaments are additionally damaged, further translation of the atlas on the axis also occurs and rotatory stability is lost. The widest portion of the spinal canal in the cervical spine occurs at C1-2, but this part of the canal narrows as the head is turned to the side. The facets can be dislocated at roughly 63 degrees of rotation, and spinal cord compression occurs with this degree of rotation as well.7 It is important to keep in mind that the vertebral arteries run in the transverse foramina and, as the head is turned, the ipsilateral vertebral artery becomes kinked whereas the contralateral artery is stretched.8 Therefore, vertebral artery injury or insufficiency may be associated with AARS.
Diagnosis and Classification
The clinical manifestation of AARS includes what has been termed the “cock-robin” position of the neck. The patient is seen with the head tilted to one side and rotated to the contralateral side with slight flexion of the neck.6,9,10 The patient cannot usually correct the deformity beyond the neutral position, and attempts to reduce the deformity by the examiner cause cervical pain. Occipital pain may occur as a result of compression of the greater occipital nerve or the C2 nerve root. Posterior fossa symptoms (vertigo, nausea, tinnitus, visual disturbance) may result from stretching or kinking of the vertebral arteries.11 Neurological compromise is relatively rare in children unless associated with trauma but is more common in adults.9,10,12 The presence of neurological signs and symptoms in adults is thought to be more common; however, there is a paucity of literature on the subject. Of seven case reports on traumatic adult AARS,13–19 two patients had partial neurological deficits.17,19 Differentiation of atlantoaxial subluxation from benign torticollis is based on the side of sternocleidomastoid spasm. In torticollis, it occurs on the contralateral side of the head rotation because contraction of the muscle leads to the neck deformity. In rotatory subluxation, the muscle contracts in an attempt to reduce the deformity.20,21
Radiographic diagnosis can be difficult but has been made much easier with the advent of newer imaging modalities. Plain radiographs are very difficult to obtain in these patients and can be complex to interpret. An open-mouth, “odontoid” view shows asymmetric lateral masses with respect to the midline.6,10,12,20,22 A lateral mass that has rotated forward appears widened and shifted toward the midline. A lateral radiograph may show one lateral mass of the atlas projecting anterior to the odontoid process and giving a “wink” sign.22,23 In adults fracture may be seen, and the fragments of bone may further confuse the issue. Dynamic films have been suggested as a better tool to determine whether the deformity is fixed,6,12,20,22 but one must be careful in this case to be sure there are no fractures or gross instability.
Computed tomography (CT) is essential in diagnosing these injuries. Cervical spine CT is almost always included in modern trauma evaluation. Axial CT scans can reveal the rotated position of the atlas on the axis, and the classification of AARS (see later) is based on the amount of forward or backward displacement seen on CT. Fractures not easily visualized on plain radiographs also become apparent on CT scans. The occiput-C1 joint should also be examined to be sure that concomitant atlanto-occipital rotatory fixation is not present.24 CT scans can be reformatted in the coronal and sagittal planes and also now in three-dimensional space, which can be very useful in making the diagnosis. The use of contrast material can help determine the position and degree of torsion of the vertebral arteries and will be useful when transarticular screws are considered. Magnetic resonance imaging is the only study that can actually image the transverse ligament.10 It can also reveal the degree of cord compromise, if any. It is not as useful as CT in imaging the bony structure of the cervical spine.
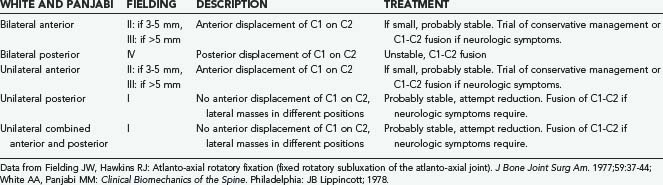
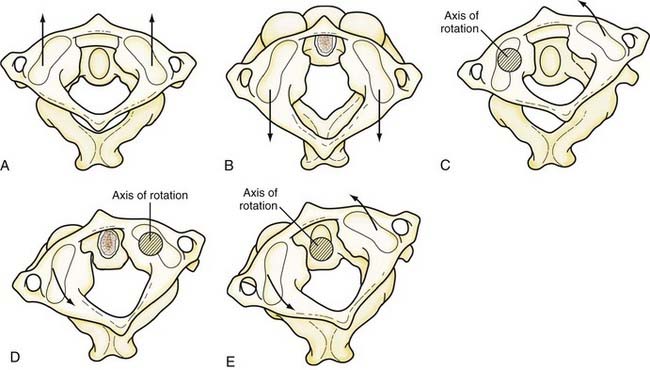
Two classification systems have been proposed for rotatory subluxation, and both are based on the direction and degree of subluxation on imaging. The Fielding system,9 proposed in 1977, divides the entity into four separate classes. In type 1, the odontoid is intact and continues to act as the pivot point for the atlas. In this class, the transverse ligament is often intact with disruption of the alar ligaments bilaterally. Types 2 and 3 encompass injuries with anterior translation of the atlas on the axis, and one lateral mass may act as the pivot point. The transverse ligament is usually disrupted or unusually lax in these cases. In type 4, there is posterior displacement of the atlas and the odontoid is compromised. In 1989, Levine and Edwards proposed the addition of type 5 to the Fielding classification, which consists of bilateral rotatory facet dislocation.25 These injuries occur almost exclusively in trauma; the transverse ligament is generally intact but the facet capsules are disrupted bilaterally. The White and Panjabi system classifies the entity into five classes based on the direction and laterality of the dislocation26 (Table 314-1 and Fig. 314-1).
Grisel’s Syndrome
Nontraumatic atlantoaxial subluxation, or Grisel’s syndrome, is a rare but dangerous complication after infectious processes or head and neck procedures. The underlying mechanism is unknown but is thought to be related to hematogenous spread of infection to the cervical spine with resulting edema and relaxation of the ligamentous structures.27 The most common cause is infection, which accounted for 48% of all cases according to one meta-analysis, followed by postsurgical cases, which accounted for 31%.28 These children often have clinical findings similar to those with painful torticollis. A high index of suspicion should be maintained in any child with a recent infection or procedure, and there should be a low threshold for imaging. A study by Rinaldo and colleagues concluded that permanent neurological sequelae may develop in 15% of patients with nontraumatic atlantoaxial subluxation.29 Children with disorders that already predispose them to ligamentous laxity, such as Down’s and Klippel-Feil syndromes, seem to be at increased risk for the development of Grisel’s syndrome. Broad-spectrum antibiotics can be a preventive measure in these high-risk groups. The majority of patients do quite well with conservative management, including reduction via cervical traction and muscle relaxants, but a small subset with higher grade subluxation may require surgical fusion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree