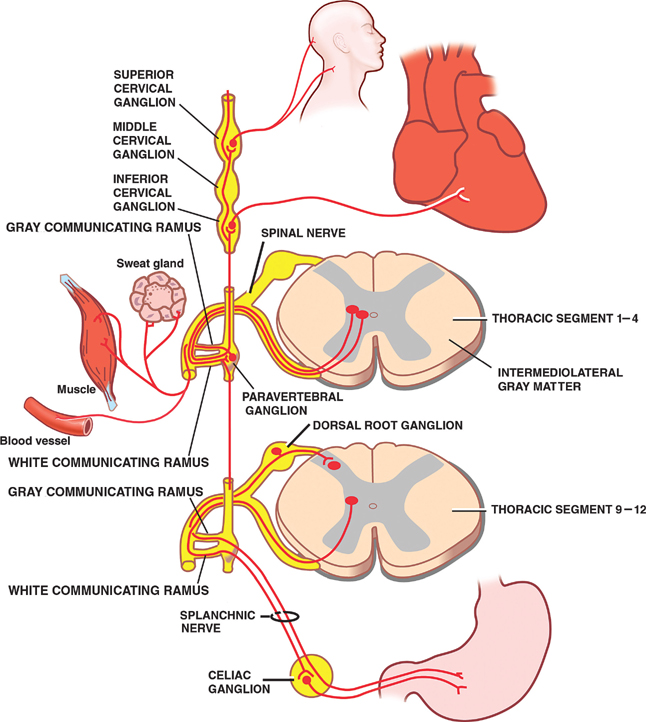
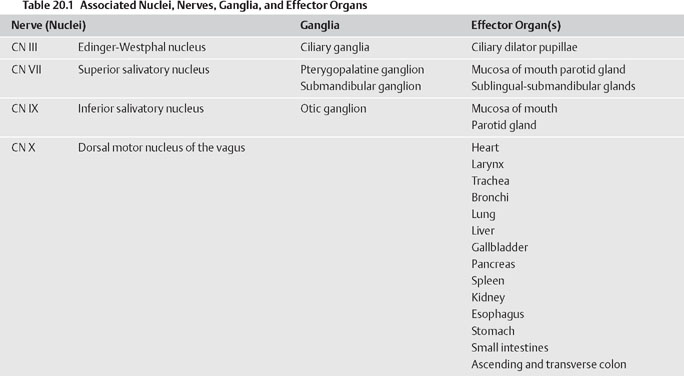
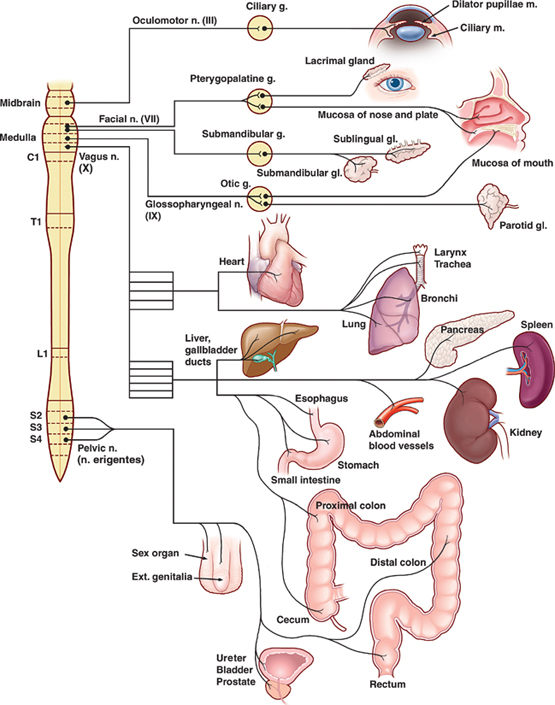
20 Autonomic Nervous System The autonomic nervous system comprises the central and peripheral components of the nervous system that regulate involuntary functions, such as those that are performed by smooth muscle, cardiac muscle, and glands. Functionally, the two divisions of the autonomic nervous system (sympathetic and parasympathetic) are distinguished on the basis of their tendency to expand (sympathetic) and conserve (parasympathetic) energy. Thus, the activation of the sympathetic system stimulates an increase in heart rate and arterial blood pressure, dilatation of the pupils and bronchioles, and inhibition of the intestine and bladder wall, whereas the parasympathetic activation system exerts an opposing effect. In other words, the sympathetic system is the “fght or fight” system, whereas the parasympathetic system maintains vegetative functions (e.g., digestion, urination, etc.). It is the delicate balance between the sympathetic and para-sympathetic outfow tracts that maintains the dynamic equilibrium of the internal environment. In maintaining homeostasis, autonomic function is associated with several other responses. Thus, autonomic and endocrine activities are closely integrated in higher centers, as are psychological and emotional inputs. Together with the autonomic system, they contribute to the so-called limbic system. For example, smelling or remembering a disagreeable food may cause one to become nauseous, with pallor, sweating, and lightheadedness. Anatomically, efferent pathways of the autonomic nervous system constitute a two-neuron limb that consists of fibers whose site of contact (i.e., synapse) lies outside the central nervous system (CNS) in the autonomic ganglia. Preganglionic efferent neurons are typically small, myelinated group B fibers, whereas postganglionic ef-ferents tend to comprise smaller, unmyelinated group C fibers. The preganglionic parasympathetic fibers are characteristically long, synapsing in or near their target organs. That is, their ganglia are often in the organ itself, for example, the myenteric plexus of the intestinal tract. The preganglionic sympathetic fibers have a very short course and terminate proximally, in a collection of ganglia that together form the sympathetic trunk (para-vertebral ganglia). The paravertebral ganglia (or sympathetic chain) run along the lateral margin of the vertebral bodies. The postganglionic sympathetic fibers follow a long course that ends in their target organs. Occasionally preganglionic sympathetic fibers pass through the sympathetic chain and terminate in a more distal plexus, for example, the hypogastric plexus. These preganglionic fibers are known as splanchnic nerves. Pharmacologically, acetylcholine is the neurotrans-mitter at all autonomic ganglia. The postganglionic para-sympathetic fibers release acetylcholine as well. However, most postganglionic sympathetic fibers release norepinephrine. Select postganglionic sympathetic neurons, such as those that innervate sweat glands, release acetylcholine rather than norepinephrine. The acetylcholine receptors on sympathetic postgan-glionic cell membranes are nicotinic, whereas the receptors on the parasympathetic postganglionic cells are muscarinic. The presence of dopaminergic interneurons in autonomic ganglia suggests that these ganglia are involved in the integration, rather than the simple relay, of information. See Fig. 20.1. The cell bodies of preganglionic sympathetic neurons are located in the intermediolateral cell column in the lateral horn of the spinal cord between levels T1 and L2-L3. The axons of these preganglionic neurons exit the spinal cord via the ventral roots, pass through the white communicating rami (remember these preganglionic fibers are myelinated), and synapse on postganglionic neurons in the paravertebral ganglia of the sympathetic trunk at their level of entry, or they may ascend or descend the sympathetic chain to fnally synapse. Alternatively, certain preganglionic fibers, which together form the splanchnic nerve, pass through the paravertebral ganglion without synapsing. Instead, they synapse in one of the prevertebral ganglia, which are distal to the spine, such as the celiac ganglion or the superior or inferior mesenteric ganglia. The neurotransmitter released by all preganglionic sympathetic neurons is acetylcholine. Upon leaving the paravertebral or prevertebral ganglia, many postganglionic fibers accompany arteries as they pass peripherally to innervate various internal organs. Other postganglionic fibers leave the paravertebral ganglia to return to the spinal nerves via the gray communicating rami, so called because most of these postganglionic fibers are unmyelinated. These fibers innervate blood vessels, sweat glands, and erector pili muscles, structures that receive no parasympathetic innervation. Because preganglionic neurons characteristically synapse on several postganglionic neurons, there is considerable divergence “built into the system.” Functionally, this is evident in the widespread effect produced by sympathetic stimulation. Further contributing to this widespread effect are a group of preganglionic fibers that accompany the splanchnic nerves and establish synaptic contacts with the secretory cells of the adrenal medulla. This neural crest structure represents a collection of specialized postganglionic sympathetic neurons that release epinephrine and, to a lesser extent, norepinephrine directly into the bloodstream. Except for the cells of the adrenal medulla, which use epinephrine, and the fibers that innervate sweat glands, which use acetylcholine, the neurotransmitter released by all postganglionic sympathetic neurons is norepinephrine. Fig. 20.1 Sympathetic outflow. See Fig. 20.2. In contrast to the thoracolumbar distribution of the sympathetic division, the parasympathetic division is distributed both rostrally and caudally. The rostral component of the parasympathetic division contains preganglionic neurons that originate in the nuclei of cranial nerves III, VII, IX, and X. These preganglionic neurons project fibers that accompany their associated cranial nerves to terminate in ganglia comprising cell bodies of postganglionic neurons that innervate the eye, the salivary glands, and the viscera of the abdomen and thorax. Associated nuclei, nerves, ganglia, and effector organs are presented in Table 20.1. The caudal component of the parasympathetic division comprises preganglionic fibers that originate in spinal segments S2 through S4, specifically in the in-termediolateral cell columns. These fibers exit the spinal cord via the ventral roots to form long pelvic nerves that terminate in or near the pelvic viscera, where they synapse on short postganglionic fibers that innervate the proximal and distal colon, the rectum, the bladder, and the genitalia. Compared with the sympathetic system, the parasym-pathetic system is capable of mounting a more discrete and localized response because there is less divergence in the contact between pre- and postganglionic neurons and between the postganglionic neurons and their target cells, and because acetylcholine is rapidly inactivated by acetylcholinesterase. Both the pre- and postganglionic neurons of the parasympathetic division use the neuro-transmitter acetylcholine.
Efferent Pathways
Sympathetic Division
Parasympathetic Division
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








