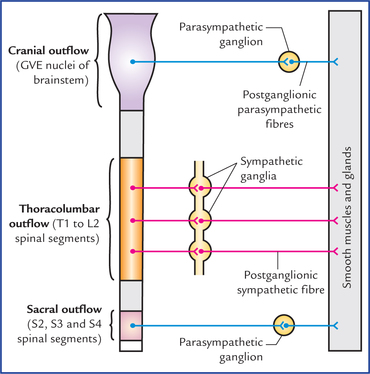
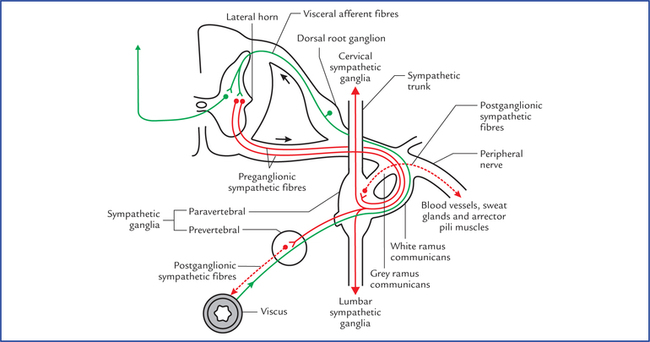
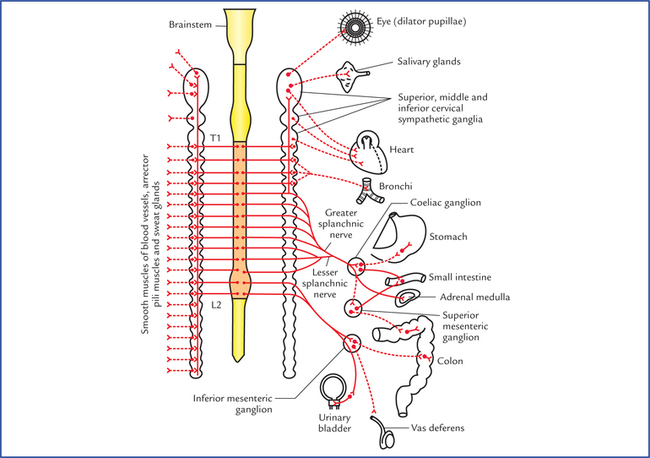
20 1. Sympathetic nervous system: The preganglionic sympathetic fibres arise from lateral horn cells of the thoracic and upper two lumbar segments (T1 to L2) of the spinal cord, hence sympathetic nervous system constitutes the thoracolumbar outflow (Fig. 20.1). The axons of preganglionic neurons project to the autonomic ganglia (the sympathetic ganglia). The ganglia are connected to each other and form a beaded chain. Fig. 20.1 Schematic diagram to show the craniosacral outflow (parasympathetic) and thoracolumbar outflow (sympathetic). Note that postganglionic parasympathetic fibres are shorter in length as compared to postganglionic sympathetic fibres. 2. Parasympathetic nervous system: The preganglionic parasympathetic fibres arise from general visceral efferent (GVE) nuclei of brainstem and lateral horn cells of the second, third and fourth sacral segments of the spinal cord, hence parasympathetic nervous system constitutes the craniosacral outflow (Fig. 20.1). The axons of preganglionic fibres project to the autonomic ganglia (the parasympathetic ganglia) which are located near or embedded in the wall of viscera/glands. The sympathetic ganglia are located near the CNS along the sympathetic chain in the paravertebral region or in front of vertebral column, hence the postganglionic sympathetic fibres are longer in length, on the other hand the parasympathetic ganglia are located near effector organ, hence the postganglionic fibres are shorter in length (Fig. 20.1). 3. Enteric nervous system: It is a network of neurons in the wall of gastrointestinal tract. The activities (functions) of the sympathetic nervous system are such that as if it prepares the body to deal with the emergency (exciting and stressful) situations. The heart rate is increased, arterioles of the skin and intestine are constricted, those of skeletal muscle are dilated, and the blood pressure is raised. There is redistribution of the blood so that it leaves the skin and GIT and pass to the brain, heart and skeletal muscles. In addition there is dilatation of pupils, inhibition of the smooth muscle of the bronchi, intestine, and urinary bladder, and closure of sphincters. It is generally said that the sympathetic stimulation mobilizes the body energy for flight or fight. • Widening of the palpebral fissure • Motor for arrector pili muscles • Vasoconstriction of blood vessels all over the body, except those in skeletal muscles • Bronchodilatation and inhibition of secretion from bronchial glands • Inhibition of gastrointestinal motility and secretions • Sensory for pain from most of the viscera • Contraction of sphincters of the bladder and bowel Once preganglionic fibres reach the paravertebral ganglia (ganglia in the sympathetic chain) they are distributed as follows (Figs 20.2, 20.3): Fig. 20.2 Sympathetic efferent and afferent fibres. The preganglionic sympathetic fibres are shown by solid red lines and postganglionic sympathetic fibres by interrupted red lines. The sympathetic afferent fibres are shown by green lines. Note the fate of preganglionic sympathetic fibres. These may (a) relay in their corresponding ganglion and pass to their corresponding spinal nerve for distribution, (b) ascend or descend in the sympathetic chain and relay in higher or lower ganglia, or (c) pass without synapse to a peripheral (prevertebral) ganglion for relay. Fig. 20.3 Sympathetic nervous system (thoracolumbar outflow). The postganglionic sympathetic fibres are shown by interrupted lines. • Synapse with the cells in the ganglion. The postganglionic fibres (non-myelinated axons) arising from ganglion cells rejoin the spinal nerves (grey rami communicantes) and distributed through its branches to the blood vessels, sweat glands and arrector pili muscles. • Ascend in the sympathetic trunk to synapse in the cervical sympathetic ganglia. • Descend in the sympathetic trunk to synapse in lumbar sympathetic ganglia. • Leave the ganglia without synapsing as splanchnic nerves and relay in the prevertebral ganglia. Some of these fibres pass to the suprarenal gland where they synapse with the cells within the medulla. These medullary cells which may be regarded as modified postganglionic sympathetic neurons, secrete epinephrine and norepinephrine. • The superior cervical ganglion is largest and formed by the fusion of upper 4 cervical ganglia. It is spindle-shaped and lies in front of transverse processes of C2 and C3 vertebra. – Grey rami communicantes to ventral rami of upper four cervical spinal nerves. – Arterial branches to, both external and internal carotid arteries. These branches form plexuses around these arteries and are distributed along their branches. The fibres carried by external carotid artery are vasomotor, sudomotor, and pilomotor and supply areas of skin mainly supplied by trigeminal nerve. – Cardiac branch (superior cervical cardiac branch) to the heart. It is motor (visceral) to cardiac muscle. • The middle cervical ganglion is small and formed by the fusion of 5th and 6th cervical ganglia. It lies in close relationship to inferior thyroid artery at the level of cricoid cartilage (C6). – Grey rami communicantes to 5th and 6th cervical spinal nerves. – Arterial branch to inferior thyroid artery for distribution to pharynx, larynx, and upper parts of the trachea and oesophagus, thyroid and parathyroid. – Cardiac branch (middle cervical cardiac branch) to the heart. • The inferior cervical ganglion is formed by the fusion of 7th and 8th cervical ganglia. It fuses with the first thoracic ganglion to form the cervicothoracic ganglion (also called stellate ganglion because its numerous branches give it a star-shaped appearance). – Grey rami communicantes to C7 and C8 (in most cases T1 also) spinal nerves. – Arterial branches to both subclavian and vertebral arteries. • They are connected by grey and white rami communicantes to the thoracic spinal nerves. • The first five thoracic ganglia (T1-T5) give postganglionic fibres to the heart, lung and oesophagus (through cardiac, pulmonary and oesophageal plexuses). • The lower eight ganglia give preganglionic fibres, which are grouped to form the three splanchnic nerves: • Greater splanchnic nerve arises from 5th to 9th thoracic ganglia. • Lesser splanchnic nerve arises from 10th and 11th thoracic ganglia. • Least splanchnic nerve arises from 12th (or last thoracic) ganglion. The abdominal part of sympathetic trunk consists of four ganglia: • Only upper two ganglia receive white rami communicantes from first and second lumbar spinal nerves. • All ganglia give grey rami communicantes to corresponding lumbar spinal nerves. • Visceral branches and lumbar splanchnic nerves from ganglia pass downwards, to form a plexus in front of the 5th lumbar and upper sacral vertebrae, called superior hypogastric plexus. It lies between the common iliac vessels. It divides into two inferior hypogastric plexuses, one on each side of the rectum. • Increase in lens curvature (antero-posterior) for accommodation. • Secretion of respiratory and digestive glands. • Inhibition of cardiac excitation, conduction and contraction. • Bronchoconstriction and increased secretion from bronchial glands. • Increased gastrointestinal motility and inhibition of pyloric and anal sphincters. • Sensory differentiation of faeces and flatus. • Contraction of muscular wall of urinary bladder (detrusor muscle) and inhibition of the internal urethral sphincter (sphincter vesicae). • Motor for initiation and maintenance of erection of penis. The functions of sympathetic and parasympathetic nervous system are compared in Table 20.1. Table 20.1 Comparison of sympathetic and parasympathetic functions
Autonomic Nervous System
Divisions of the Autonomic Nervous System
Sympathetic Nervous System
Functions of the sympathetic nervous system
Efferent nerve fibres (thoracolumbar outflow)
Sympathetic trunks
Cervical sympathetic ganglia
Thoracic ganglia
Lumbar ganglia
Parasympathetic Nervous System
Functions of the parasympathetic nervous system
Structure
Sympathetic function
Parasympathetic function
Eye
Dilatation of pupil
Constriction of pupil
Lacrimal gland and Salivary glands
Viscous secretion
Watery secretion
Bronchial smooth muscle
Relaxation
Contraction
Heart
Increases heart rate
Decreases heart rate
GIT
Decreases peristalsis and constricts the sphincters
Increases peristalsis and relaxes sphincters
Genitourinary tract
• Bladder wall and sphincter
Relaxes bladder wall and constricts the sphincter
Contracts the bladder wall and relaxes the sphincter
• Penis
Ejaculation
Erection
Skin
• Sweat glands
Produce sweating
No effect
• Arrector pili
Contraction of arrector pili leading erection of hair
No effect
Blood vessels
• Skin, splanchnic vessels
Contraction
No effect
• Skeletal muscles
Relaxation
No effect ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Autonomic nervous system






