14 Basic Electromyography
Analysis of Spontaneous Activity
Analysis of Spontaneous Activity
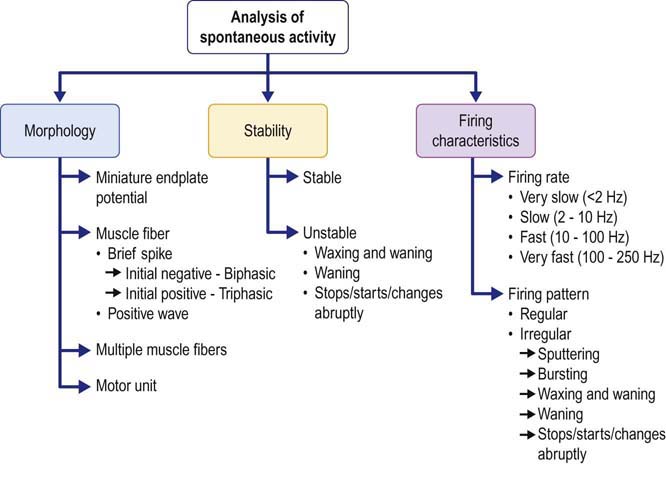
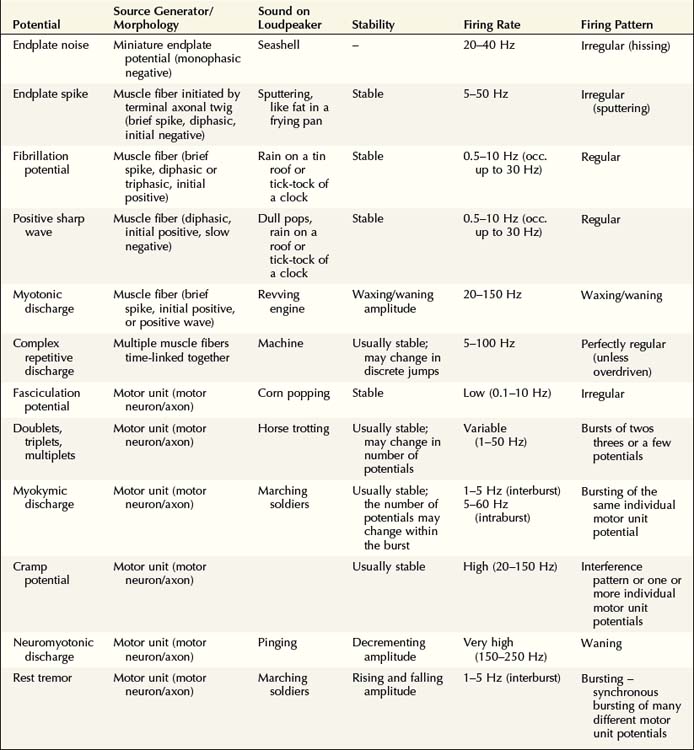
The identification of any spontaneous activity can be achieved by either pattern recognition or analysis of the waveform. With experience, the characteristic sound and appearance of each waveform become easily recognizable. However, when first learning needle EMG or when encountering an unusual waveform, one must be able to systematically analyze the waveform according to the following attributes: (1) morphology, (2) stability, and (3) firing characteristics (Figure 14–1). Using this information, nearly every spontaneous waveform can be identified correctly.
Morphology
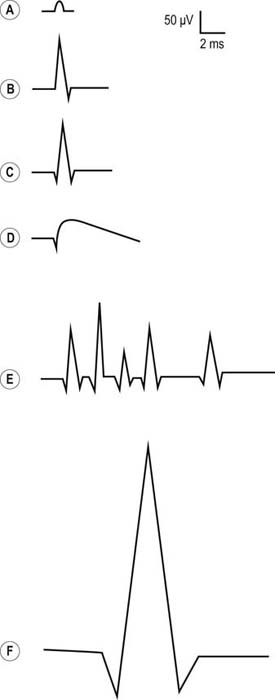
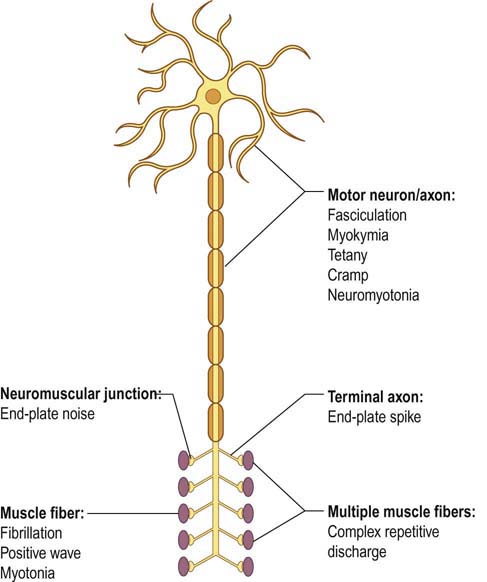
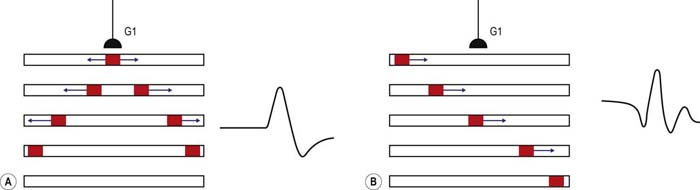
The source of a spontaneous discharge often can be identified by its distinctive morphology, including the size and shape of the potential (amplitude, duration, number of phases) and its initial deflection (Figure 14–2). By defining its source generator, the type of discharge usually can be identified. The source generators that must be differentiated include (1) the neuromuscular junction (NMJ), (2) a single muscle fiber, (3) the terminal axon twig, (4) a motor neuron/axon, and (5) multiple muscle fibers linked together (Figure 14–3, Table 14–1).
At the NMJ (i.e., endplate zone), miniature endplate potentials (MEPPs) occur spontaneously. They result from the normal spontaneous exocytosis of individual quanta of acetylcholine traveling across the NMJ, leading to a non-propagated, subthreshold endplate potential. If the EMG needle is near the endplate zone, MEPPs can often be recorded. They have a distinctive small amplitude and monophasic negative morphology (Figure 14–2A). These potentials are normal spontaneous discharges and are referred to as endplate noise.
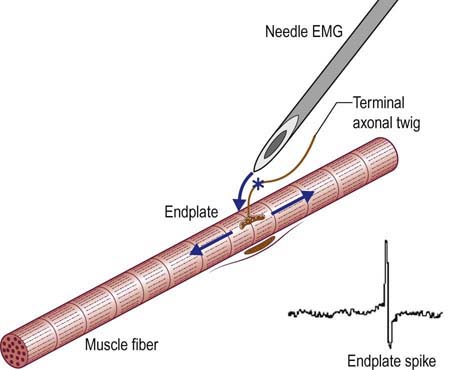
When a muscle fiber depolarizes to threshold, a muscle fiber action potential (MFAP) is created. The MFAP can assume one of two basic morphologies, either a brief spike or a positive wave. The brief spike typically is 1 to 5 ms in duration, biphasic or triphasic, with a low amplitude (typically 10–100 µV). This brief spike morphology is seen most often when a muscle fiber depolarizes spontaneously, for example, in denervation, but it can also occur as the result of an individual terminal axon twig depolarizing and then propagating across the NMJ to create an MFAP. Attention to the initial deflection and to whether the brief spike is biphasic or triphasic often can help distinguish between the two (Figure 14–4). If the depolarization begins under the recording needle electrode, a biphasic potential is seen, wherein an initial negative peak is followed by a short positive phase (Figure 14–2B). This signifies that the needle is at the endplate zone, where the depolarization begins, and usually is the result of the EMG needle irritating the terminal nerve twigs near the endplate zone. A nerve twig action potential then leads to an MFAP, known as an endplate spike, which is a normal finding (see section on Endplate Spikes). The reason for the initial negativity is similar to that of the compound muscle action potential (CMAP) in motor nerve conduction studies, wherein the initial deflection is negative when the active recording electrode is properly placed over the motor endplate zone. Otherwise, brief spikes that occur from the spontaneous depolarization of a muscle fiber are associated with an initial positive, usually triphasic morphology. When the depolarization begins at a distance from the needle, there is an initial positive deflection as it moves toward the needle, followed by a negative phase as it moves beneath the needle, and then a final positive deflection as it moves away from the needle (Figure 14–2C).
In addition to the brief spike, an MFAP can assume a positive wave morphology, with an initial brief positive phase followed by a long negative phase (Figure 14–2D). Both positive waves and initial positive, triphasic brief spikes are seen most often as denervating potentials, known as positive sharp waves and fibrillation potentials, respectively. However, it should not be surprising that myotonic discharges, which also originate in muscle fibers, have the same basic morphology as denervating potentials, either positive waves or brief spikes. This point exemplifies the important concept that morphology alone cannot be used to identify a potential. Although the morphology of a potential usually can be used to correctly identify its source generator, additional information regarding its stability and firing characteristics is needed to fully characterize and identify any potential (see later).
The next major category of spontaneous discharges is that which arises from motor neurons or their axons. Any discharge that occurs as a result of the spontaneous depolarization of a motor neuron or its axon (prior to its terminal branches) leads to a potential with the morphology of a motor unit (Figure 14–2F) known as a motor unit action potential (MUAP). Spontaneous discharges generated by the motor neuron or its axon include fasciculation potentials, doublets, triplets, and multiplets, myokymic discharges, neuromyotonic discharges, and cramp potentials, all of which lie along the spectrum of abnormal spontaneous MUAPs. They can be differentiated from each other, however, by their stability and firing characteristics (described in the following subsections). If the motor unit is normal, the MUAP morphology will be normal: typically two to four phases, 5 to 15 ms in duration, and variable amplitude depending on the needle position. If the motor unit is pathologic, the number of phases, duration, and amplitude of the MUAP may be abnormal. Differentiating a MUAP from a single MFAP usually is straightforward and typically can be done quite simply by analyzing its duration and amplitude.
The last distinctive waveform that must be recognized is that of time-linked individual muscle fibers, such as occurs in complex repetitive discharges. One might ask how this waveform differs from an MUAP, which also represents many muscle fibers linked together. The difference is that the muscle fibers in a motor unit fire more or less synchronously and, in almost every situation, summate to create a larger potential 5 to 15 ms in duration. In contrast, the multiple muscle fibers in a complex repetitive discharge fire consecutively and usually are discernible as individual spikes that are time linked together (Figure 14–2E).
Insertional Activity
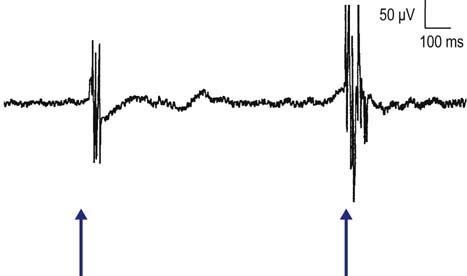
The needle EMG examination of each muscle begins with the assessment of insertional activity. When a needle is quickly moved through muscle, muscle fibers depolarize in a brief burst for several hundred milliseconds, known as insertional activity, which is a normal finding (Figure 14–5). The presence of insertional activity is important to the electromyographer to confirm that the needle is in muscle rather than fat or subcutaneous tissue. At least four to six brief needle movements are made in four quadrants of each muscle to assess insertional activity. Needle movement resulting in any waveform other than endplate potentials (see following section) that lasts longer than 300 ms indicates increased insertional activity. Increased insertional activity may be seen in both neuropathic and myopathic conditions. In rare conditions, where muscle has been replaced by fat and fibrous connective tissue, insertional activity may actually be decreased.
Spontaneous Activity: Normal
Endplate Noise
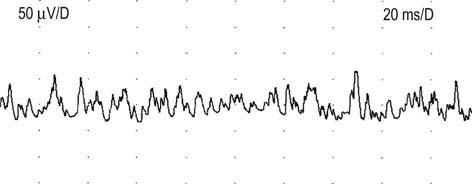
These are low-amplitude, monophasic negative potentials that fire irregularly at 20 to 40 Hz and have a characteristic “seashell” sound on EMG (Figure 14–6). Physiologically, they represent MEPPs. They are recognized by their characteristic shape and sound and by their frequent association with endplate spikes (described in the next subsection).
Endplate Spikes (“Nerve Potentials”)
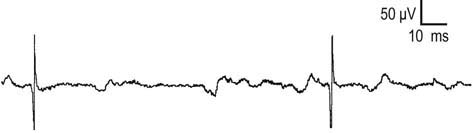
Endplate spikes are MFAPs that fire irregularly up to a frequency of 50 Hz (Figure 14–7) and usually are seen along with endplate noise. They are biphasic, with an initial negative deflection, reflecting that the needle is at the site where the action potential is generated. They have a cracking, buzzing, or sputtering sound on EMG. The key features that differentiate endplate spikes from fibrillation potentials, which are also brief spikes, are their initial negative deflection and their highly irregular firing rate.
Endplate spikes are thought to occur as a result of needle-induced irritation of a terminal nerve twig and the subsequent activation of a nerve action potential leading to an MFAP (Figure 14–8). Thus, the needle is necessary to create these potentials. This is in contrast to endplate noise (MEPPs), which occurs spontaneously, without the presence of an irritating source. In summary, endplate spikes only occur when a needle is in the muscle and close to the endplate zone, close enough to mechanically irritate nearby terminal nerve twigs.
Spontaneous Activity: Abnormal Muscle Fiber Potentials
Fibrillation Potentials
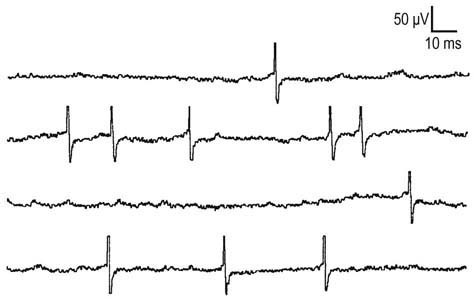
A fibrillation potential is derived from the extracellular recording of a single muscle fiber (Figures 14–9 and 14–10). These spontaneous depolarizations of muscle fibers are the electrophysiologic markers of active denervation. Although they typically are associated with neuropathic disorders (i.e., neuropathies, radiculopathies, motor neuron disease), they also may be seen in some muscle disorders (especially the inflammatory myopathies and dystrophies) and rarely in severe diseases of the NMJ (especially botulism). As they are generated in muscle fiber, fibrillation potentials are recognized by their single MFAP morphology: a brief spike with an initial positive deflection, 1 to 5 ms in duration, and low in amplitude (typically 10–100 µV). The firing pattern is very regular, with a rate usually 0.5 to 10 Hz, occasionally up to 30 Hz. In very chronic conditions (lasting >6–12 months), fibrillation potentials may become very tiny (<10 µV in amplitude) (Figure 14–11). On EMG, single fibrillation potentials sound like “rain on the roof.” Although fibrillation potentials fire at a regular rate, they may slow down very gradually over several seconds before stopping.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree