Figure 69-1 Chest x-ray (posteroanterior view) showing elevation of the diaphragm, right greater than left.
Bilateral phrenic nerve conduction studies3 were similar at 2, 8, and 12 months. On the right, 13 milliseconds, 100 microvolts, left: 9 milliseconds, 100 microvolts (normal 6.5 +/− 0.8 milliseconds; 660 +/− 201 microvolts); latency, amplitude, respectively (Fig. 69-2). Needle EMG of the right diaphragm4 at 8 months showed insertional activity but no fibrillation potentials or positive sharp waves and no motor unit potentials. The prolonged latency, reduced amplitude of the diaphragm compound muscle action potential and the absence of both denervation potentials and motor unit potentials on needle electromyography suggested relatively pure demyelination of the phrenic nerves.
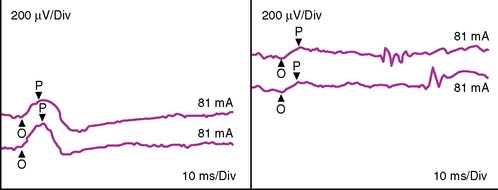
Figure 69-2 Left (left panel) and right (right panel) phrenic nerve conduction studies at 12 months performed with surface electrodes by stimulating twice either phrenic nerve in the neck and recording the diaphragm compound action potential at the ipsilateral costal margin. Latencies are prolonged and amplitude is reduced, especially on the right. div, division; mA, milliamp; ms, millisecond; O, onset; P, peak; uV, microvolt.
We believe that the radiofrequency induced lesion of the auricles and pulmonary veins had damaged the adjacent phrenic nerves distal to the point of electrical stimulation in the neck. The demyelination persisted for 12 months, which is an unusually long time for demyelination. In his report, the surgeon indicated mechanical damage to the phrenic nerves was unlikely because both nerves were identified and specifically avoided during surgery. He speculated thermal (heat) injury during the radiofrequency ablation.
CONCLUSION
Studies of cadavers indicate ablation procedures involving the superior venocaval vein and right pulmonary vein present a risk of phrenic nerve damage. The left phrenic nerve is more likely to be vulnerable during these procedures because of the adjacent great cardiac vein, left obtuse marginal vein and left atrial appendage.5
In comparison to catheter ablation, the incidence of phrenic nerve injury after coronary bypass surgery determined by phrenic nerve conductions was 7% to 26%.6,7 In a well-designed prospective study, phrenic nerve conduction and needle EMG studies of the diaphragm were performed before, and serially after, coronary bypass surgery in 94 patients.8 Fifteen patients (16%) had phrenic nerve injury, 12 unilateral, 3 bilateral. In 12 the lesion was demyelinating with recovery in 1 to 3 months and in 6 axonal with recovery in 6 to 18 months. The mechanism of injury is likely dependent on the technical variation, and is generally considered to be due to surgical manipulation, hypothermia or ischemia from harvesting of the internal thoracic artery.8
Thermal injury to nerves has been studied in both humans and animals. Thermal coagulation with radio frequency is used to treat trigeminal neuralgia, the heat being applied to the gasserian ganglia and posterior rootlets. Symptoms were improved in 90% of patients.9 Light touch was preserved, suggesting smaller diameter myelinated and unmyelinated fibers, which conduct pain signals, were predominantly affected.
Direct heating of the peripheral nerve in cats,10 dogs,11 and rats12 revealed conduction block and loss of both myelinated and unmyelinated fibers. In rats, there was conduction block and subsequent axonal degeneration.13 Blood flow studies indicated damage to the vasonervorum and subsequent nerve ischemia. Unmyelinated fibers seemed most susceptible.
In experiments, especially relevant to our patient, radiofrequency pulmonary vein ablation in dogs caused immediate transient phrenic nerve dysfunction without temperature change, suggesting a direct current affect. However, with increasing temperature, there was progression to long-lasting nerve damage due to heat.14
The severe bilateral damage to both phrenic nerves in our patient is an exceptionally rare complication of the radiofrequency catheter ablation procedure. Animal and human experiments suggest that early conduction block with subsequent axonal degeneration is secondary to heat-induced phrenic nerve ischemia. There was evidence in our patient, although not conclusive, of focal and unusually long lasting demyelination.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








