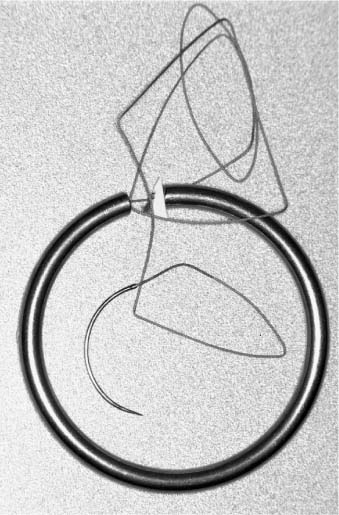
11 In the United States, the annual prevalence of newly diagnosed bone metastasis totals at least 100,000 cases.1,2 Substantially more cases go unreported. The incidence of spinal cord compression by metastatic disease, which has devastating consequences, has been estimated at 20,000 cases annually.3 The spinal cord and cauda equina can be compressed by metastatic epidural or locally invasive paraspinal tumors. Pain, numbness, weakness, and loss of bowel and bladder function are common manifestations that progress to paralysis in the absence of timely recognition and treatment. Several studies have documented a higher rate of functional recovery when treatment is initiated before severe neurologic deficits develop and while patients still remain ambulatory.4–7 A randomized trial recently compared direct surgical therapy plus radiotherapy to radiotherapy alone for metastatic spinal cord compression.8 The patients treated with radical direct decompressive surgery followed by radiotherapy retained their ability to walk longer and regained their ability to walk more often than those treated with radiotherapy alone. The surgical patients also required fewer steroids and narcotics than the radiotherapy patients. Although the role of surgical intervention always must be tailored to the individual patient, its role is becoming more prominent in the treatment of malignant spinal tumors. In addition to the established role of pre- and postoperative external beam radiotherapy (EBRT), brachytherapy is another adjunct in the therapeutic armamentarium that should be considered in the treatment of these diseases.9–13 In this context, brachytherapy refers to the implantation of radioactive agents at the time of spinal decompression and reconstruction. Sodium iodide I–125 is the agent most commonly used. Iridium–192 has also been used. Locally implanted radioactive seeds can boost the exposure of previously irradiated areas or serve as an adjunct to areas not yet treated with EBRT. Several authors have have reported the use reported the use of I-125 implants for local control of malignant spinal tumors.9,14–17 In the largest series treated at a single institution, 30 patients underwent spinal brachytherapy procedures for malignant tumors associated with spinal cord compression.15 The technique was associated with durable local control of the metastatic disease and prolonged preservation of ambulatory function. Brachytherapy for the treatment of malignant tumors associated with spinal cord compression must be considered before surgery begins. Consultation with a radiation oncologist, even immediately before surgical intervention, is critical for pre- and intraoperative planning of these procedures. In some cases, therapeutic radioactive agents must be ordered before a planned surgical procedure can be performed. Surgical interventions include simple decompression via a laminectomy with transpedicular extension to more radical posterior approaches such as costotransversectomies or en bloc vertebrectomies. Anterolateral approaches may be used for ventral decompression. These approaches are usually followed by immediate reconstruction of the spinal column. Preoperative imaging studies must be analyzed thoroughly to identify regions of the tumor that may be difficult to access and therefore be at a high risk for a local recurrence. Such regions, as well as areas adjacent to neural elements, should be targeted for brachytherapy. During an apparent gross total resection, attention should be focused on the operative bed adjacent to the spinal cord and nerve roots. Dosimetry considerations are also important in patients who have undergone EBRT before surgical intervention. This information is crucial in calculating brachytherapy doses to avoid radiation-induced myelopathy and related complications. The radioactive implant must be selected preoperatively. Ir–192 and I–125 implants have both been used in the local treatment of malignant spinal tumors.9–13 Ir 192 had been used as a temporary dose of radiation. Conversely, I–125 implants are permanent.9 The reported experience with I–125 implants is much greater than that with Ir 192, and the safety and efficacy of the former are well profiled.9,14,15 Underlying the more widespread use of I 125 is that the relatively low energy of I–125 (28 KeV) minimizes the risks of radiation hazard and allows a very small area (4 to 5 mm) to be radiated. The half-life of I 125 is ~60 days, so most of the radiation decays within 1 year. I–125 seeds absorbed onto a silver rod and coated with polyglactin 910 absorbable suture are commercially available and dispensed within a welded titanium capsule (OncoSeed RAPID Strand™, Med-Physics, Arlington Heights, IL). A needle at one end allows the strand to be sutured into place if desired (Fig. 11-1). The seeds are spaced 1 mm apart (Fig. 11-2). They are positioned to maintain the 1-cm spacing throughout the planar and volume implants. Dosimetry is performed using orthogonal plain radiographs and computed tomographic scans (Fig. 11-3). Several techniques for calculating radiation doses have been advocated.13,15 Given the large experience with I–125 permanent radioactive seeds, the following technique focuses on their placement. After a tumor has been resected and adequate hemostasis has been attained, attention is turned to the resection cavity. A thorough review of the preoperative imaging studies allows regions of the tumor that may have been resected suboptimally to be anticipated. Frozen-section pathologic analysis of the margins of the resection bed can also confirm the presence of residual tumor. Visual inspection, preoperative imaging, and assessment of margins can be used to determine the optimal placement for the radioactive implants. Metallic clips or specialized screw implants can be used to out-line the borders of the target, and later to aid in radiographic localization additional Gelfoam. This strategy creates an amalgam that holds the I–125 seeds in their intended geometric distribution. When a tumor involves the dura, the seeds are placed after the tumor is resected and before spinal reconstruction begins. Care is exerted to avoid disturbing the distribution of the seeds. If the dura is not involved, the seeds can be placed after the reconstruction procedure is completed.15 Given the propensity of Gelfoam to absorb water and swell, the implants must be embedded carefully. Several case reports have outlined the danger of using this material near neural structures where postoperative swelling can lead to compression.12,18 Tumor resection that creates a cavity decreases this concern, but great care is always necessary.
Brachytherapy for Malignant Spinal Tumors
 Preoperative Considerations
Preoperative Considerations
 Operative Treatment
Operative Treatment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




