31 Cervical Arthroplasty
I. Key Points
– Anterior cervical discectomy and fusion (ACDF) remains the gold standard in the surgical management of symptomatic cervical spondylosis and central disc herniation.
– The emerging option of cervical arthroplasty is aimed at preservation of segmental motion with maintenance of adequate stability.1
– Key elements to achieving a good result and avoiding complications with cervical arthroplasty:
• Appropriate patient selection (competent posterior elements, without spondylolisthesis)
• Correct neck positioning during surgery (neutral to slightly lordotic cervical curvature)
• Generous decompression with resection of the bilateral uncovertebral joints and posterior longitudinal ligament
• Precise end plate preparation (parallel or domed according to device, with preservation of cortical end plates)
• Accurate midline acquisition
• Proper implant sizing (footprint coverage of disc space and avoidance of overdistraction)
II. Indications
– The current indications for cervical arthroplasty in the United States include symptomatic one-level cervical radiculopathy or myelopathy in patients who have failed nonsurgical management.
– Relative contraindications include (1) cervical kyphosis, (2) cervical spondylosis with incompetent or significantly degenerated facets (>2 to 3 mm subluxation on flexion-extension x-rays), (3) cervical ankylosis, (4) osteoporosis, and (5) cervical trauma with ligamentous or facet injury.
III. Technique
– Prophylactic antibiotics should be given; perioperative dexamethasone and intraoperative neuromonitoring are optional.
– The patient is positioned supine with the neck in neutral or slight extension, with shoulder retraction to allow adequate fluoroscopic visualization of the target level.
– Create a transverse skin incision along preexisting skin crease near the index level.
– Perform dissection between the carotid sheath and strap muscles (anterior-medial to sternocleidomastoid muscle) to expose the retropharyngeal space.
– The trachea and esophagus are retracted and protected medially by self-retaining retractors placed under the elevated longus colli muscles for exposure of the anterior cervical spine.
– After confirmation of the index level by lateral fluoroscopic x-ray, anterior cervical discectomy is performed with curettes, rongeurs, or drill.
– Full bilateral nerve canal decompression must be achieved, including removal of the uncovertebral joints.
– End plate preparation is crucial in cervical arthroplasty and may differ between prostheses. Caution must be taken not to violate the cortical surface, which would increase the risk of implant subsidence or migration.
– Midline acquisition, implant sizing (including footprint size and disc height), and insertion trajectory should be controlled to allow physiological range of motion in the cervical spine after implantation of the prosthesis.
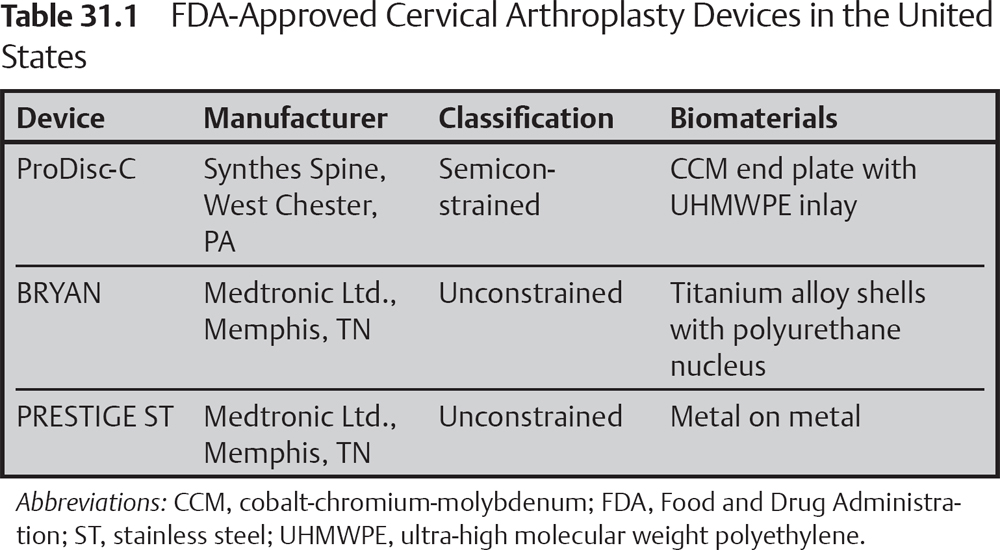
– There are several cervical artificial discs currently on the market, and each has its unique design and fixation system (Fig. 31.1). Therefore, there are differences in the technique of final implantation. But they all have the common feature of absolutely requiring adequate decompression of the index level. Some differences in material and biomechanics may provide advantages in certain scenarios. In choosing one, the surgeon must have a thorough understanding of the prosthesis’s biomechanical design and familiarity with its implantation (Table 31.1).
IV. Complications
Complications are similar to those for ACDF; however, there are four primary reasons to consider revision of cervical arthroplasty:
– Radiculopathy (or other new-onset neurologic deficit) after cervical arthroplasty
– Subsidence
– Implant migration
– Ankylosed joint (formation of significant heterotopic bone around the implant)
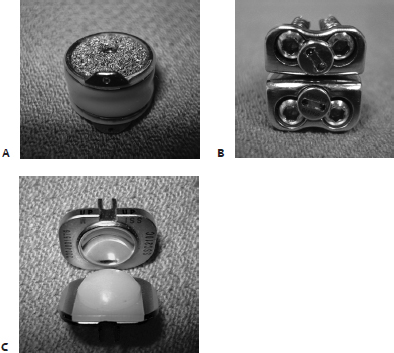
Fig. 31.1 (A–C) Photographs of the three arthroplasty devices currently approved by the U.S. Food and Drug Administration. (A) Bryan Device. (B) Prestige Device. (C) Pro-Disc C Device. (From Baaj et al, History of Cervical Arthroplasty. Neurosurgical Focus. September 2009, Figs. 2–4.)
V. Postoperative Care
Same as for ACDF, except for the following:
– Mummaneni et al suggested that perioperative oral nonsteroidal antiinflammatory drugs (NSAIDs) for 2 weeks2 might reduce the incidence of heterotopic bone formation.
– Avoid neck collar (encourage normal motion).
To date, there have been three prospective randomized multicenter U.S. studies comparing cervical artificial disc implantation with ACDF in patients treated for single-level cervical disc disease with radiculopathy or myelopathy.
– The largest of these studies compared the PRESTIGE ST Cervical Disc System (Medtronic, Memphis, TN) with ACDF in a total of 541 patients. At 24 months’ follow-up, the arthroplasty group demonstrated maintenance of physiologic segmental motion in association with improved neurologic success, improved clinical outcomes, and a reduced rate of secondary surgeries compared with conventional ACDF.2
– Heller et al compared the BRYAN Cervical Disc (Medtronic, Memphis, TN) with ACDF in 463 patients. At 24 months after surgery, the arthroplasty group showed a statistically greater improvement in the primary outcome variables: neck disability index score and overall success. No statistical difference was found between the arthroplasty and ACDF groups with regard to secondary surgical procedures or implant-related adverse events. The arthroplasty patients returned to work nearly 2 weeks earlier than the ACDF patients.3
– Murrey et al compared single-level ProDisc-C (Synthes Spine, L.P., West Chester, PA) arthroplasty with ACDF in 209 patients. At 24 months after surgery, visual analog scale (VAS), neck disability index (NDI), and neurologic success rate demonstrated no statistical difference between the arthroplasty and ACDF groups. Statistically fewer reoperations and less pain medication usage were noted in the ProDisc-C cohort.4
VII. Surgical Pearls
– Generous decompression of the neuroforamen bilaterally (including asymptomatic side)
– Proper end plate preparation
– Correct implant selection (footprint size, height)
Common Clinical Questions
1. How many degrees of neck range of motion loss could result from a single-level ACDF?
2. What is the incidence of development of symptomatic adjacentlevel disease after single-level ACDF?
3. Why should patients take oral NSAIDs and avoid neck collar use after cervical arthroplasty?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







