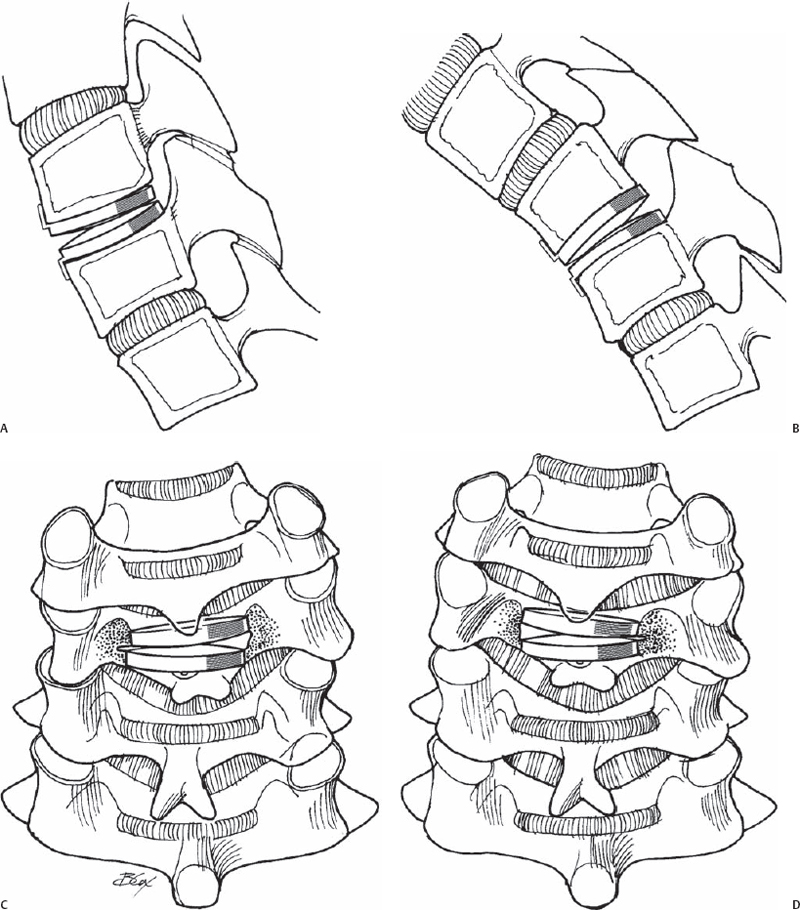
77 Rick C. Sasso and Ben J. Garrido Anterior cervical diskectomy and fusion has historically been the gold standard treatment for patients experiencing cervical radiculopathy or myelopathy refractory to nonoperative measures. The safety and effectiveness of this procedure have been established and demonstrated in the literature; however, limitations have evolved, and subsequently alternatives such as disk replacement are being investigated. Such innovative technology has addressed kinematic and biomechanical factors in cervical spine motion. Intervertebral disk replacement is designed to preserve motion, both at the affected and adjacent levels, and avoid limitations of fusion. Hilibrand et al have described adjacent level degeneration in patients having undergone cervical fusion at a rate of 2.9% of patients per annum. Such new-onset degenerative changes and possible recurring neurologic symptoms may be deferred or eliminated with cervical disk replacement. In addition, potential complications related to fusion such as pseudarthrosis, anterior plate problems, and morbidity associated with bone graft harvest may be avoided. Cervical disk arthroplasty is designed to provide physiologic motion and eliminate abnormal loading stresses at adjacent levels that lead to accelerated degeneration. Disk arthroplasty results may be highly subject to procedural technique. Preoperative planning with magnetic resonance imaging (MRI) or computed tomography (CT) myelogram is essential to determine neural compressive lesions. Appropriate disk sizing and assessment of excessive osteophytes is performed with preoperative CT scans. Disk height should be relatively normal without profound collapse, facet joints must not be extremely degenerated, and reasonably normal motion must be present. Intraoperative patient positioning is supine, with the spine stabilized in neutral position without hyperextension. It is important to perform adequate decompression of both the spinal canal and the bilateral neuroforamen. With motion-sparing techniques, it is extremely important to adequately decompress the asymptomatic side as well as the target site. Appropriate end-plate preparation is critical to allow for bony ingrowth into the prosthetic shell while maintaining the strong subchondral end plate. Undersizing the base-plate area may result in end-plate damage and implant subsidence. Prosthetic disk placement is confirmed under fluoroscopy. Postoperative immobilization is not required. Intervertebral disk replacement is indicated for cervical radiculopathy due to a herniated disk or osteophyte complex at a single level between C3 and C7. These patients must have failed aggressive nonoperative treatment modalities and be skeletally mature with relatively normal segmental motion. Cervical disk replacement surgery should not be performed in patients with sagittal plane abnormalities, spondylolisthesis, retrolisthesis, spondylolysis, or any evidence of segmental instability. Poor surgical candidates and those with active systemic or operative site infection should be excluded. Those patients who have a history of previous cervical surgery, metabolic bone disease, progressive neuromuscular disease, or significant osteoporosis, or are on corticosteroid therapy, should not be considered for this procedure. In addition, radiographically confirmed ankylosis, ossification of the posterior longitudinal ligament (OPLL), fixed kyphosis, and incompetent end-plate or severe facet joint arthritic changes should also be excluded. Cervical myelopathy secondary to factors other than a soft disk herniation at the level to be treated via an anterior diskectomy decompression should be avoided. There are several disk arthroplasty systems for which early data has been reported but long-term outcomes are still pending. Wigfield et al recently reported favorable results after 2 years with the Prestige I disk design (Medtronic Sofamor Danek, Memphis, TN). They concluded that motion was successfully preserved without sacrificing device stability. No devices dislocated, and procedural complications were limited to two cases of transient hoarseness, which resolved demonstrating procedural safety. Goffin et al also reported early excellent results for the Bryan disk (Medtronic Sofamor Danek) placed at a single level in 60 patients. Sasso et al compared the initial functional outcome results on the Bryan disk replacement with anterior cervical fusion. This study used multiple outcome measures, also demonstrating favorable results for disk replacement compared with anterior cervical arthrodesis. Significant more motion at 3, 6, and 12 months was retained in the disk replacement group (Fig. 77.1). The clinical benefits of maintaining motion and providing symptom relief are postulated to delay or avoid adjacent level degeneration. These promising results suggest that artificial cervical disk replacement is comparable, if not superior, to fusion at least in the short term. Although not the current standard, wide acceptance will depend on long-term outcome studies. Current success with artificial cervical disk replacement has demonstrated that the intended effects are being achieved, sparing cervical motion and decreasing future fusion associated morbidity.
Cervical Disk Replacement
Description
Expectations
Indications
Contraindications
Special Considerations
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








