34
Open Lumbar Microscopic Diskectomy
David A. Wong
Description
The open posterior lumbar microscopic diskectomy provides a minimally invasive, often outpatient decompression of a nerve root compromised by a herniated nucleus pulposus. The operating microscope enhances illumination and visualization within the surgeon’s visual field. This allows more precise identification of the pathology and other critical anatomic structures such as nerve roots and epidural veins. Superior orientation and careful handling of tissues minimizes the risks of intraoperative complications and postoperative problems such as scarring and instability. Integrating the fundamentals of anatomy, technology, and surgical technique in the open lumbar microscopic diskectomy establishes several critical skills. Mastery of these techniques opens the door to more advanced procedures such as the far lateral/ intertransverse diskectomy and the lumbar laminaplasty (bilateral decompression of the spinal canal via a unilateral surgical approach).
Expectations
Most patients obtain significant relief of their radicular symptoms. If compression of neural structures is the dominant symptom generator, improvement may be seen in a matter of hours or days. However, inflammation in the nerve may take weeks to months to resolve, even once compression is removed. Axonal damage to the nerve already present at the time of surgery (usually correlating with a significant neural deficit on physical exam) may repair/regenerate over a year or more.
Diskectomy does not cure the patient’s underlying degenerative changes. If mechanical back pain is part of the presenting symptom complex, the patient needs to be aware that this might persist and require long-term participation in a postoperative strengthening and stabilization program to optimize the surgical result. Rarely, mechanical factors of back pain or instability are sufficient so that fusion is a consideration.
Overall, a 50 to 75% reduction in symptoms, a 5 to 8% rate of recurrent disk herniation, and a 5% likelihood of future fusion are reasonable expectations for the patient and surgeon.
Indications
Persistent radicular symptoms or signs despite 1 to 3 months of nonsurgical care are good clinical indications for surgery. Radicular findings should correlate to the pathology visualized on confirmatory imaging studies. More urgent surgical intervention may be considered in situations of severe, incapacitating symptoms, progressive neurologic deficit, or cauda equina syndrome. Back pain from a large central disk herniation is an indication for microdiskectomy.
Contraindications
Conflicting symptoms and signs versus imaging studies is a situation for restraint. Significant nonorganic (Waddell’s) findings, particularly in a scenario of minor radicular changes and minimal pathology on imaging, is a relative contraindication. Primary mechanical back pain is not likely to be significantly improved by diskectomy.
Special Considerations
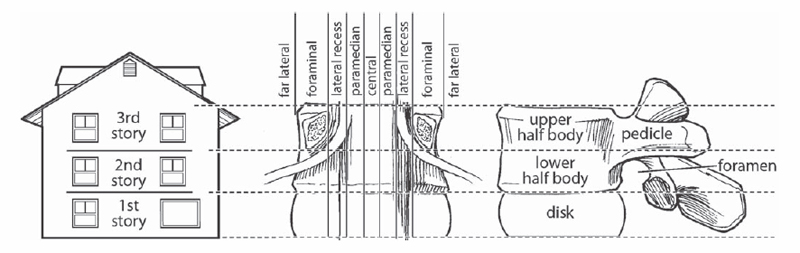
A key principle of successful microsurgery is the precise awareness of spinal anatomy. This bears on the preoperative analysis and localization of the patient’s pathology as well as the intraoperative orientation of the surgeon. Pathology can be accurately localized by mentally mapping a grid to overlie the spinal canal (Fig. 34.1). The horizontal lines of the grid corresponding to the inferior/superior direction are defined by McCulloch’s first-, second-, and third-story house analogy. The first story is opposite the disk. The second story encompasses the lower half of the vertebral body with the foramen at its posterior aspect. The third story corresponds to the upper half of the vertebral body anteriorly with the solid, bony pedicle located posterior. Correlate the presence of disk fragments opposite the disk space versus foramen versus pedicle on the axial images to precisely locate pathology in a vertical orientation. The medial/lateral lines of the grid are laid out according to Macnab’s system of central versus paramedial versus lateral recess versus foraminal versus far lateral location of disk herniation/root compression. The grid location L4-L5/R1P would thus describe a disk herniation at the L4-L5 segment, on the right side, first story vertically (opposite the disk space), and in the most common paramedial location. Pathology may encompass more than one grid area.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







