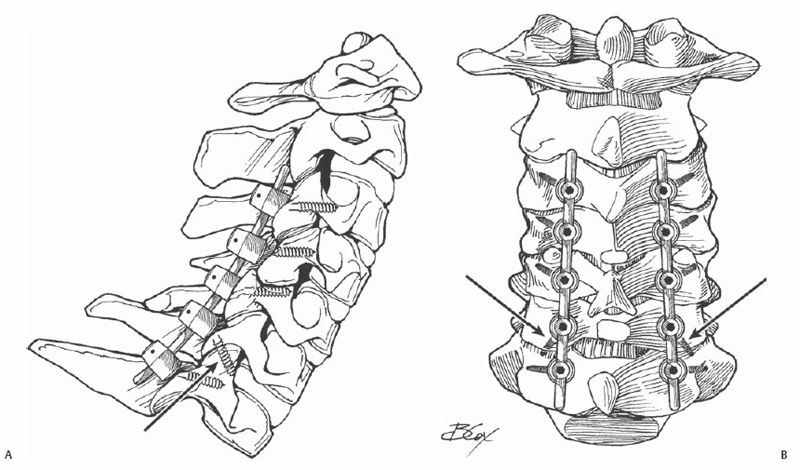
12 Jeffrey M. Spivak This fixation technique is not commonly used, as there are no clinical series of posterior cervical fusions reported using this method alone. However, this technique can be quite useful for isolated facet joint fusions, and has been described as a salvage technique in cases of failed lateral mass fixation. A full understanding of the anatomic orientation of the cervical subaxial facet joints is imperative for the proper use and execution of this fixation technique. The cervical facet joints are flat and angled cephalad at approximately 60 degrees in the coronal plane. Standard techniques for lateral mass screw insertion involve directing the screw path laterally and cepha-lad, avoiding any penetration of the facet joint. Subaxial facet screw fixation requires a caudal direction of the screw, perpendicular to and therefore across the facet joint surface. Transfacet screw fixation can be used as an isolated fixation technique or, more commonly, as a supplementary method of fixation in combination with anterior plate fixation following anterior diskectomy or cor-pectomy. The technique is technically demanding, with little room for error, but it can be used to salvage inadequate lateral mass fixation. Biomechanical data have shown that transfacet screw placement provides stronger resistance to pullout than bicortical lateral mass screws, with the most pronounced difference noted at the C7-T1 level. Comparison testing of fixated motion segments to resistance to physiologic motion (flexion-extension, lateral bending, axial rotation) has not been done for the two fixation techniques, and the strength of direct transfacet fixation alone to resist these forces is unknown. Use of subaxial facet screw fixation is indicated as an adjunct to cervical spine fusion. The technique can be used to support an anterior decompression and fusion procedure or as an isolated posterior fusion. It can be used in conjunction with other posterior fixation techniques including spinous process wiring and sublaminar wiring when these posterior elements are available. The technique can also be used as part of a multilevel posterolateral fixation construct in combination with lateral mass or pedicle fixation using rod or plate longitudinal members. It is very useful as a salvage technique for failed lateral mass fixation (Fig. 12.1). Fig. 12.1 Lateral view (A) and PA view (B) of transfacet fixation at C6-C7 as a salvage for failed right C6 lateral mass fixation. The caudal screw fixation (arrows) can be seen well in both views. Use of subaxial facet screw fixation is contraindicated in cases where one or both of the lateral masses is comminuted, incompetent, or disconnected from the remainder of the vertebra secondary to either a traumatic or neoplastic process. In cases requiring decompression of the neural foramen posteriorly via partial facetectomy and foraminotomy, this technique is not likely to be suitable due to the smaller amount of remaining facet joint surface following the decompression. For cases requiring fusion due to trauma or neoplasm, preoperative evaluation with computed tomography (CT) scanning including sagittal reconstructions is necessary to assess the bony integrity of the lateral masses and facet joint to be sure that posterolateral fixation of any type is a viable option for providing stability. Prone positioning with rigid hold of the head using skull pin fixation is recommended. Adequate cervical alignment should be achieved before the skin incision if possible. If not, intraoperative reduction and realignment must be achieved before screw placement. Subaxial cervical facet screws are used only for fixation, not for segmental realignment. Fluoroscopic guidance for screw placement is extremely useful to be sure that the joint is crossed near its midportion and to ensure adequate surrounding bone stock to avoid iatrogenic facet fracture. Fluoroscopy is also helpful to ensure that the next caudal facet joint is not disrupted at its anterior aspect due to too caudal screw angulation. Fluoroscopic visualization by level without parallax is important to ensure proper screw insertion. The left and right facet joints at each level should be visualized as one structure without incongruent overlap. Deformities of the motion segment can be compensated for by adjusting the position of the operative table or the fluoroscopy unit to visualize the facet joints properly. The alignment of the facets should be visualized and evaluated preoperatively once the patient is positioned and before prepping and draping and beginning the procedure. Use of a transfacet screw as part of a multilevel lateral mass fixation construct will place the screw-head offset from the regular lateral mass screw head positioning within the plate. This may require some compromise of optimal screw insertion point and angulation to keep it within the plate construct. Multiaxial screw and rod systems, with increased flexibility for screw head position and screw angulation, are preferred for this type of mixed fixation construct. The main difficulty with this type of screw placement is achieving adequate fixation across the facet joint. Use of intraoperative lateral fluoroscopy is extremely helpful to ensure proper trajectory and screw length. As with cervical lateral mass screws, exposure of the posterior neck should allow for full definition of the lateral border of the lateral mass and the posterior aspect of the facet joint to be bridged. This joint capsule should be removed and the posterior facet decorticated, but the capsules of the joints above and below must be meticulously maintained if they are not to be fused. The proper screw insertion point for a cervical transfacet screw is described as 1 mm medial and 1 to 2 mm caudal to the midportion of the lateral mass. The screw path is directed as perpendicular as possible to the facet joint, approximately 40 degrees caudally from the posterior lateral mass surface, and 20 degrees laterally to avoid the exiting nerve root and transverse foramen; 3.5-mm-diameter cortical bone screws are utilized, which is a standard size in most manufacturers’ cervical screw-rod and screw-plate sets. Screw length should allow for fixation across the anterior cortex of the caudal lateral mass. This technique is most commonly used itself as a bailout for failed segmental lateral mass fixation. When it is used as such and fails, as by fracture of the inferior articular process, the only potential monosegmental bailout would be with the use of pedicle screw fixation. Connection of pedicle screws to lateral mass or transfacet screws requires the use of offset connectors and rod-based systems, and cannot be done as part of segmental plate fixation. Additional lateral mass fixation used above or below a transfacet screw often provides adequate additional fixation along with onlay bone grafting. Failure of this technique when using a primary procedure for monosegmental fixation may be salvageable with the use of lateral mass fixation if adequate bone stock is available, or by pedicle screw fixation if the surgeon has adequate experience with this technique in the midcervical spine. Fixation and fusion of additional levels above or below is also a potential salvage technique. Fixation of the contralateral side, with or without midline (spinous process) fixation, may also be sufficient and obviate the need for inclusion of any additional levels.
Cervical Subaxial Transfacet Screw Placement
Description
Key Principles
Expectations
Indications
Contraindications
Special Considerations
Special Instructions, Position, and Anesthesia
Tips, Pearls, and Lessons Learned
Difficulties Encountered
Key Procedural Steps
Bailout, Rescue, Salvage Procedures
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








