27 Chiari I Decompression
I. Key Points
– Consistent feature of Chiari I: disruption of normal cerebrospinal fluid (CSF) flow through the foramen magnum. Most symptomatic cases have descent of cerebellar tonsils ≥5 mm below the margins of the foramen magnum, which is best seen on magnetic resonance imaging (MRI).
– Surgical treatment for symptomatic patients consists of enlarging the foramen magnum (suboccipital decompression), usually with C1 laminectomy.
– Syringomyelia, if present, will usually respond to suboccipital decompression alone.
II. Indications
– Symptoms include
• Pain (the most common symptom; mostly suboccipital headache that is exacerbated by neck extension), neck pain, arm pain, weakness/numbness in one or more limbs, loss of temperature sensation (dissociated sensory loss),1 balance difficulties. Fifteen to 30% of patients meeting radiographic diagnostic criteria are asymptomatic.2
– Signs3 include
• Hyperactive lower-extremity (LE) reflexes, downbeat nystagmus, gait disturbance, hand muscle atrophy, cerebellar signs, Babinski sign
III. Technique
– Position: Patient is prone on chest rolls with the neck flexed and the head in a Mayfield head holder (Schaerer Mayfield, Randolph, MA) or on a horseshoe head rest.
– Skin incision: midline incision from the inion down to the C2 spinous process
– The fascia is opened in a Y or T, leaving a cuff of tissue attached to the occiput for use during closure.
– The occipital bone is exposed down to the foramen magnum (FM). The posterior C1 arch is exposed (taking caution regarding the vertebral arteries).
– At a minimum, the surgery consists of enlargement of the FM (suboccipital decompression) often combined with C1 laminectomy. The area of removal of occipital bone should be as wide as the FM, but should be no more than 2.5 to 3 cm above the FM (to avoid cerebellar herniation). Techniques include thinning the bone with a high-speed drill and removing the residual bone with a Kerrison rongeur (Fig. 27.1). Options to suboccipital decompression include
• C2 laminectomy: reserved for cases with severe tonsillar descent below the superior margin of C2 (Table 27.1)
• Duraplasty: A Y-shaped incision is made in the dura (some surgeons preserve the arachnoid4) and a patch graft is sewn in watertight closure with 4-0 Nurolon (Ethicon, Johnson & Johnson, Piscataway, NJ). Options for sources of graft: pericranium, fascia lata, and dural substitutes. Pericranium can be harvested through the same incision by subcutaneous dissection.5
• Instead of opening the dura in all cases, some surgeons simply lyse extradural constricting bands. Then intraoperative ultrasound may be used to determine if there is adequate room for CSF circulation. If not, a duraplasty is performed.
• An alternative to duraplasty (primarily in pediatrics): partial thickness scoring of the dura with several parallel passes of a scalpel
– Closure: A multilayered water-tight closure is performed. Skin approximation with sutures is preferred over staples. A wound drain is not used. A lumbar drain is occasionally used for 2 to 3 days.
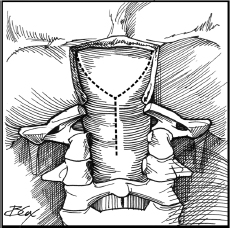
Fig. 27.1 Posterior exposure of the dura after bony removal, showing an outline of the Y-shaped dural incision. (From Vaccaro AR and Albert TJ, Spine Surgery: Tricks of the Trade, Thieme; 2009. Reprinted with permission.)
IV. Complications
– The major complication from surgery is CSF leak. This may be external (and can be initially treated by oversewing the site of leak and temporary lumbar drainage) or subcutaneous (pseudomeningocele).
– Overaggressive removal of occipital bone can lead to cerebellar ptosis (sagging of the tonsils).
– Injury to brainstem or posterior inferior cerebellar arteries (PI-CAs). Avoid aggressive treatment of tonsillar adhesions. Use an operating microscope if needed.
– Post-op apnea or respiratory depression: tends to occur within the first few days post-op. Monitor for apnea and increasing arterial pCO2.
V. Outcomes
Pre-op symptoms of headache or pain respond in 82% with a 4 year follow-up.1 Weakness is less responsive to surgery, especially if atrophy has occurred. Symptoms of greater than 2 years’ duration have a worse prognosis.
Postoperative Care
– Intensive care unit (ICU) observation overnight with head computed tomography (CT) the next morning to rule out epidural hematoma.
– Mobilize and discharge typically in 24 to 48 hours postoperatively.
– Early follow-up in clinic recommended to assess wound, d/c sutures/staples, and ensure no pseudomeningocele has developed.
VI. Surgical Pearls
– Treating the Chiari malformation via suboccipital decompression corrects syringomyelia in the majority of cases without the need for any other procedure.
– Fifteen to 30% of patients with radiographic criteria of Chiari I malformation are asymptomatic.2
Table 27.1 Variation with Age of the Location of the Inferior Tonsillar Pole Relative to the Foramen Magnum6
| Age (years) | Two standard deviations below the FM (mm) | |
| 0–9 | 6 | |
| 10–29 | 5 | |
| 30–79 | 4 | |
| 80–89 | 3 |
Abbreviation: FM, foramen magnum.
Common Clinical Questions
1. Three weeks following a suboccipital decompression with duraplasty for a symptomatic Chiari I malformation, a patient develops a tense, very painful fluid collection under the incision and an MRI shows it has the appearance of CSF without any other significant abnormalities. The best management options are:
A. Percutaneous tapping of the fluid after careful skin prep, and then tightly wrapping the head with bandages to prevent reaccumulation
B. Placement of a lumbar drain and having the patient lie flat in bed for 3 days
C. Surgical exploration of the wound in the OR with repair of dural defect, and placement of lumbar drain for 3 days with the head of bed greater than 30 degrees
D. Placement of an external ventricular drain to divert the CSF from the wound, and conversion to a ventriculoperitoneal (VP) shunt if the patient is drain dependent after 5 days
2. A 48-year-old female elementary school teacher presents with a 20-year history of headaches that occur almost every day at the same time. They vary from the left to right side and are often associated with neck pain. No medication or change in position has provided any relief. Her primary care physician ordered a brain MRI, on which the only abnormality identified is that the inferior pole of the cerebellar tonsils is 4 mm below the foramen magnum. She is neurologically intact. You should:
A. Order a cine flow MRI
B. Have her see a neurologist to rule out other causes of chronic headache
C. Order a cervical MRI
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







