Chapter 158 Circumferential Cervical Spinal Fusion
The Rationale for Circumferential Surgery
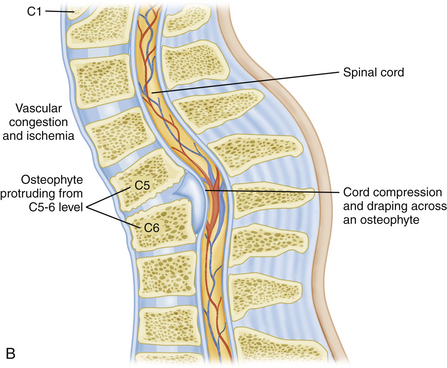
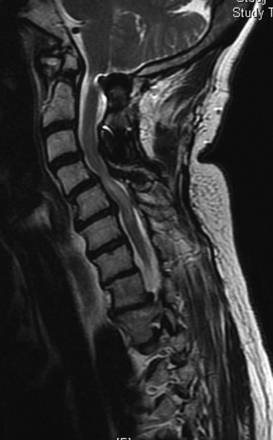
Certainly one of the most obvious reasons for choosing bidirectional surgery of the cervical spine would be that the patient presents with obvious compression of both the ventral and dorsal surfaces of the spinal cord (Fig. 158-1). If the patient is not overly frail, then one can make a rationale for this approach. There is some degree of inherent common sense to directly remove the compressive structure of the spinal cord. One variation might be surgery to treat ossification of the posterior longitudinal ligament (OPLL).1–4 Patients with dramatic anterior compression are commonly treated by posterior decompression in order to avoid the significant pitfalls of anterior surgery.
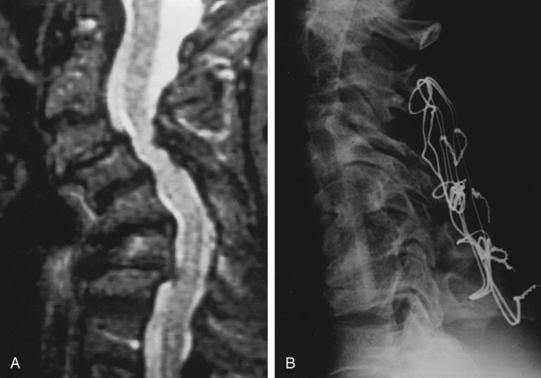
Restoration of spinal alignment has received an increasing degree of attention recently as a potential crucial factor in the outcome of patients with cervical spondylitic myelopathy (CSM).5–8 Most would agree that circumferential surgery is indicated for patients that present in frank kyphosis (Fig. 158-2). This may result from numerous factors including posterior migration of the cord, vascular perfusion, and longitudinal stresses on the cord. If a patient is left in a kyphotic position, then draping and potential anterior compression of the spinal cord are certainly possible. The classic example of this would be postlaminectomy kyphosis. Nottmeier et al. recently published results of cervical kyphotic deformity correction using a anterior-posterior reconstruction. Their patient population had a mean preoperative kyphosis of 18 degrees. They were able to achieve a mean correction of sagittal angle of 22 degrees. This resulted in a mean postoperative sagittal angle of 4 degrees. There was no reported loss of deformity correction during the follow-up period and they reported a fusion rate of 97.5%.8
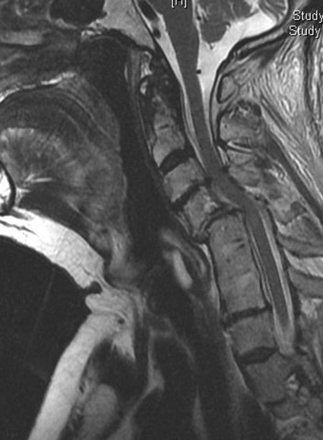
FIGURE 158-2 T2-weighted MRI in a patient with a previous fusion of C5–C7 with a pronounced anterolisthesis and kyphosis of C4–C5.
Several studies have looked at the potential importance of postoperative posterior spinal cord migration. There is a concern that residual kyphosis may allow the spinal cord to be draped across the vertebral column, which may contribute to compromise of the spinal cord via vascular compromise or longitudinal stress. Lee et al. attempted to quantitatively assess preoperative factors that would predict this postoperative movement of the cord. Besides the commonly stated importance of preoperative sagittal balance, they also found significance in the relative degree of stenosis directly above the “laminectomized” level to be particularly important.9 However, the clinical importance of cord shift remains uncertain. Hatta et al. found no clinical correlation in myelopathy outcomes to cord migration.10
There has also been some attention given to the potential effects of “longitudinal stress” to the spinal cord by Uchida et al. It is interesting to consider the potential similarities of this to the physiologic derangement that has been documented to occur with tethering of the spinal cord.11,12
History
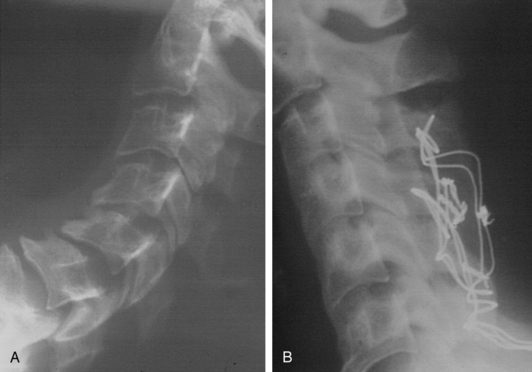
Bidirectional surgery for the cervical spine was originally reserved for cases of clear violation of stability of both the anterior and posterior elements of the cervical spine. Most cases dealt with either trauma or neoplastic disease. Instrumentation of the spine was limited to wiring techniques (Figs. 158-3, 158-4, and 158-5). Cases frequently required staging, and patients commonly required prolonged immobilization.
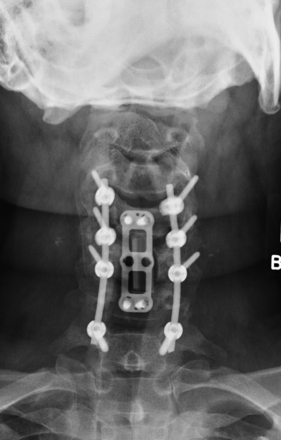
The evolution of surgical hardware has taken us from stainless steel wiring techniques to lateral mass plates and to polyaxially screw and rod fixation (Figs. 158-6 and 158-7). This has made single-stage anterior-posterior reconstructive procedures more feasible and reasonable in a larger number of patients.13

FIGURE 158-6 A case demonstrating the use of a lateral mass plate system, which became the first widely used screw system.
The surgical training for treatment of complex spinal disorders has also rapidly expanded. As a result, anterior decompression involving segmental reconstructions and corpectomies has become increasingly routine for spinal surgeons.
Technique
Imaging
Patients should be evaluated with preoperative plain x-rays in addition to the expected magnetic resonance imaging (MRI) and or computed tomography (CT) myelogram. Abnormal signal on MRI images may also offer some prognostic information regarding potential patient recovery. Mastronardi et al. studied patients with spondylotic myelopathy and found that T2 signal changes are potentially reversible with decompression. T1-weighted signal changes were associated with the worst prognosis and were thought to represent irreversible damage to the cord (Figs. 158-3 and 158-8). Patients with myelopathy that had no signal abnormalities on their preoperative MRI were found to have the best prognosis.14 This is an interesting concept to include in the debate of whether patients with cervical cord compression should be considered for early treatment or for a conservative approach during follow-up.
Anesthesia
Preoperatively the patient should be assessed regarding potential instability, range of motion, and exacerbation of neurologic symptoms associated with neck movement. The findings will determine whether the patient can be put to sleep with standard techniques or may require an awake fiber-optic intubation. This concern cannot be overemphasized in the ankylosing spondylitis patient. This pathology can produce alarming instability with devastating neurologic morbidity. All patients with ankylosing spondylitis should be considered for intubation with awake fiber-optic techniques. The authors believe that it is crucial to discuss the issues with the anesthesia team, so that no miscommunication occurs.
Neuromonitoring
Somatosensory potentials can be used with muscular paralytics and are not quite as sensitive to inhalational anesthetics. The posterior columns are monitored. One potential drawback to SSEPs is that a significant amount of time can elapse before the surgeon is alerted to dysfunction of the tissue.15
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree