Fig. 2.1
36-in. antero-posterior X-ray illustrating scoliosis terms. CSVL Central Sacral vertical line
2.2 Adolescent Idiopathic Scoliosis Classification Systems
Based on etiology, scoliosis has been broadly subdivided into idiopathic, neuromuscular, syndromic, congenital, and degenerative types. The idiopathic type (which is most common) can be subclassified further according to the patient’s age at diagnosis into infantile, juvenile, adolescent, and adult groups [5]. The early efforts at classification of scoliosis were essentially focused on the adolescent idiopathic scoliosis (AIS) subtype.
Schulthess in 1905 classified scoliosis into cervicothoracic, thoracic, thoracolumbar, lumbar, and combined double primary [6]. This classification was based on curve type and its location. Subsequent publications by James in 1954 [7] and Moe in 1970 [8] excluded the cervicothoracic type due to its rarity. However, they retained the fundamental principles of curve location and type in classifying the disorder. These features were noted to be constant for a curve even during its growth [9]. The early classifications were inadequate for making treatment decisions. Advancements in the understanding of the clinical features of scoliosis, investigative modalities, and surgical techniques led to more refined classification schemes. These include the classification systems of King [10], Coonrad [11], Lenke [12], and the Peking Union Medical College [3].
2.2.1 The King System
The King classification was aimed at choosing the patients who are suitable for selective thoracic fusion in the presence of combined thoracic and lumbar scoliosis and to identify the segments to be fused. A retrospective review of 405 patients who had undergone posterior spine fusion with Harrington rod instrumentation for thoracic AIS was done. They excluded the patients who had single lumbar or thoracolumbar curves, developmental delay, neuromuscular disease, and spondylolisthesis and those who were older than 25 years at the time of surgery. The following set of x-ray films were analyzed for each patient: preoperative standing anteroposterior (AP) or posteroanterior (PA) and a set of preoperative supine side-bending AP films. The curve types were assessed based on the CSL and the stable vertebra was noted. The term “flexibility index” was introduced. This is determined by measuring the percentage of flexibility of the thoracic and lumbar curves on maximum lateral bending x-ray films. The percentage correction of the thoracic curve is deducted from that of the lumbar curve; this difference is the flexibility index [10].
Type I is an S-shaped curve in which both the thoracic curve and the lumbar curves cross the midline. The lumbar curve is larger than the thoracic curve on the standing radiograph. The flexibility index is a negative value (i.e., the thoracic curve was more flexible on side bending). Type II is an S-shaped curve in which both the thoracic and lumbar curves cross the midline. The thoracic curve is equal to, or greater than, the lumbar curve and the flexibility index is ≥0. Type III is a thoracic curve in which the lumbar curve does not cross the midline (so-called overhang). A type IV long thoracic curve is one in which L5 is centered over the sacrum but L4 tilts into the long thoracic curve. In type V, there is double thoracic curve in which the T1 is tilted into the convexity of the upper curve and the first rib is elevated on this convexity.
2.2.2 The Coonrad System
In 1998, Coonrad et al. noted the lack of a comprehensive, data-based, and user-friendly coronal pattern classification of idiopathic scoliosis [11]. They reviewed the records and radiographs of 2,000 consecutive patients with idiopathic scoliosis. These patients spanned a period of 30 years. Their aims were (1) to identify and categorize the spectrum of coronal curve patterns in a large sample of patients with idiopathic scoliosis according to the SRS definition of the apical vertebra and (2) to apply simple numerical nomenclature for classification. The classification was seen as a vital prelude to the consideration of the sagittal and three-dimensional variables of idiopathic scoliosis. The flexibility of the curves was determined by a supervised recumbent lateral bending coronal x-ray. Eleven types were described and these are summarized below.
Type 1A consists of thoracic and lumbar curves and both are structural. The lumbar curve is larger and/or less flexible, and its apex is at/or below the L1–L2 disc space. Type 1B consists of thoracic and thoracolumbar curves, both are structural. The thoracolumbar curve is larger and/or less flexible, and its apex is at T12, L1, or the disc space in between. Type 2A consists of thoracic and lumbar curves, both are structural. The thoracic curve is larger and/or less flexible and the apex of the lumbar curve is at or below the L1–L2 disc space. Type 2B consists of thoracic and thoracolumbar curves, both are structural. The thoracic curve is larger and/or less flexible. The apex of the lumbar curve is at T12, L1, or the disc space in between. Type 3 consists of a thoracic curve that is structural, and its apex is at T7–T9. Type 4 consists of a thoracic structural curve with the apex at either T10 or T11. The lower end vertebra is usually at L2 or L3 and the L4 is tilted into the curve. Type 5 consists of double thoracic curves and both are structural. The T1 or T2 vertebra is usually tilted into the upper curve. Both apices are located at the thoracic spine segment. Type 6 consists of a thoracolumbar curve, the apex of which is at T12, L1, or the disc space in between. Type 7 consists of a lumbar curve, and the apex is at the L1–L2 or L4–L5 disc spaces or between these. Type 8 consists of triple curves; the size of the largest of the three curves determines the laterality. Type 9 consists of multiple curves. The largest number in the Coonrad study was the quadruple.
This classification was based on the following characteristics of the curves: the location, number, relative Cobb angles, and flexibility of each curve when they are multiple. The sagittal and three-dimensional features of the deformity were not considered. It was however noted that these were necessary for the choice of treatment, fusion levels, and surgical approach. The identification and categorization of the spectrum of existing coronal pattern types is considered a mandatory prerequisite for any classification. This classification complemented the King’s system. Its interobserver and intraobserver reliability was initially reported to be 98.7 % and 100 %, respectively. However, the former was subsequently found to be only 46 % (κ = 0.38) [15]. The Lenke classification system was introduced 3 years later.
2.2.3 The Lenke System
Lenke et al. in conjunction with the Scoliosis Research Society (SRS) introduced another classification system in 2001 which is based on both coronal and sagittal aspects of the scoliotic deformity. This method was designed to determine the appropriate vertebral levels that should be included in a fusion. They studied four x-ray films for each of their 27 patients, including the coronal and lateral views of the standing long cassette x-rays and the coronal views of the right and left supine side bending. The curve locations were defined as proximal thoracic (PT), main thoracic (MT), or thoracolumbar/lumbar (TL/L). The apex of the PT curve lies at T3, T4 or T5. That of the MT curve lies between T6 and the T11/T12 disc. The SRS definitions were applied to distinguish between major and minor curves and also to define the apices of the thoracolumbar and lumbar curves. The flexibility of the minor curves was considered. They lacked normal flexibility if the Cobb angle is ≥25° on side-bending radiographs and/or kyphosis is at least +20°, and these were described as structural. The curve types were based on the identification of the major curve and the structural characteristics of the minor curves [12] as follows.
In type 1, the MT curve is the major curve; the PT and TL/L curves are minor and nonstructural. Type 2 consists of double thoracic curves; the MT curve is major, while the PT curve is minor and structural. The TL/L curve is minor and nonstructural. Type 3 consists of double major curves. The Cobb angle of the MT is ≥TL/L or it may be lesser, in which case the difference is not greater than 5°. Both curves are structural and the MT is regarded as the major curve, while the PT curve is nonstructural. Type 4 consists of triple major curves, the PT, MT, and TL/L. All are structural and either of the two latter curves may be the major curve. In type 5, the TL/L curve is structural and it is the major curve. The PT and MT curves are nonstructural. In type 6, the TL/L curve is the major curve, and it is at least 5° greater than the MT which is also structural. The PT curve is nonstructural. See Fig. 2.2.
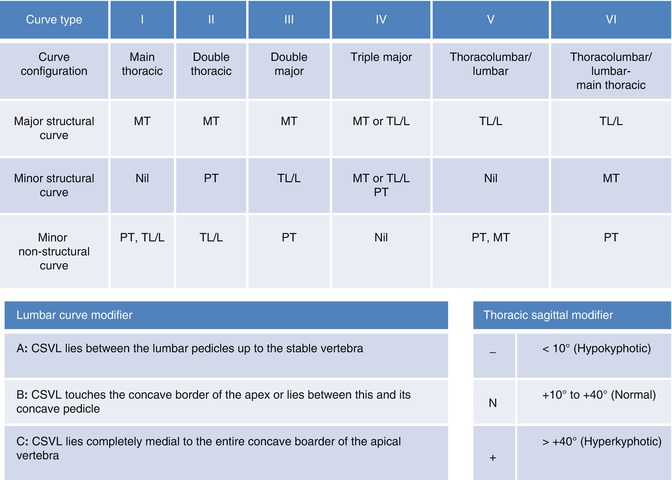
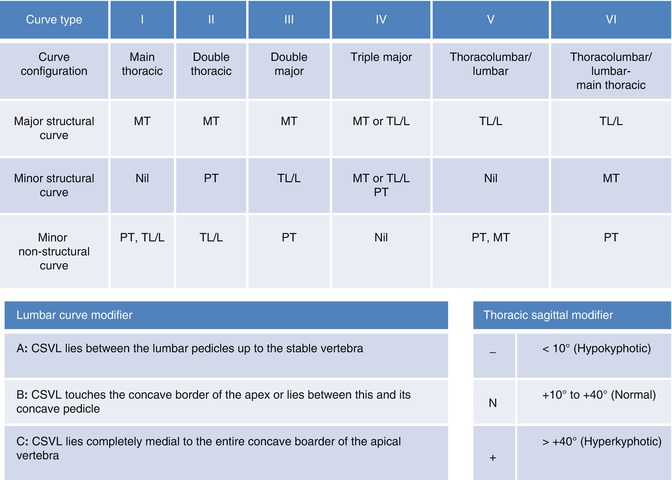
Fig. 2.2
The Lenke system. A structural curve has a Cobb angle of ≥25° on side-bending radiographs and/or kyphosis of at least +20°. The minor non-structural curves maybe present or not. PT Proximal Thoracic curve. MT Main Thoracic curve. TL/L Thoracolumbar/Lumbar curve. CSVL Central sacral vertical line (Adapted from, Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, Blanke K. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am 2001;83:1169–81, [12])
Lumbar spine modifiers A, B, or C were introduced because the lumbar deformity alters spinal balance and affects proximal curves. Modifier “A” is applied when the CSVL runs between the lumbar pedicles to the level of the stable vertebra. The curve apex must be in the thoracic spine, at or cephalad to the T11/T12 disc. Thus, modifier A can only be applied for a main thoracic curve (types 1–4). It is not applied for thoracolumbar/lumbar curves (types 5 and 6) or when the CSVL lies on the medial aspect of the lumbar apical pedicle. Modifier “B” is applied when the CSVL touches the concave margin of the lumbar curve apical vertebra body (or bodies if the apex is a disc) or when it lies between this border and the concave pedicle. The TL/L curves are excluded because the curves all have a thoracic apex. Modifier C is applied if the CSVL lies completely medial to the entire concave lateral aspect of the thoracolumbar or lumbar apical vertebral body or bodies (if the apex is a disc).
The kyphotic component of the thoracic spine deformity was described in this method of classification with another set of modifiers: −, N, or +. The mean normal sagittal thoracic alignment from the fifth to the twelfth thoracic vertebra is +30° with a range of +10° to +40° [16]. Patients who have adolescent idiopathic scoliosis tend to have decreased thoracic kyphosis or even thoracic lordosis in comparison with normal controls [16, 17]. The sagittal thoracic modifiers were determined by measurements from the superior end plate of the fifth thoracic vertebra to the inferior end plate of the twelfth thoracic vertebra on a standing lateral radiograph. Modifier “−” is applied if there is thoracic hypokyphosis, which is a curve <+10°. Modifier “N” is applied for normal thoracic kyphosis (+10° to +40°), while the “+” sign is applied for hyperkyphotic thoracic curves (>+40°). The recommendation for spinal arthrodesis is that it should include only the major curve and structural minor ones.
Lenke et al. noted inaccuracies in assessing axial plane deformity on biplanar radiographs; thus the axial components of the deformities were excluded from this system of classification. The authors stated that the mean interobserver reliability for determining curve type with this system was 93 % (range, 85–100 %), with a mean κ value of 0.92 (range, 0.83–1.00), while that of the King system was found to be 64 %, and the κ value was 0.49 [14]. Subsequently, other investigators reported moderate range interobserver reliability for the Lenke system [18, 19].
The Lenke system is more comprehensive than the earlier classifications; it also provides for objective curve assessments to aid surgical planning. The sagittal component of the deformity was included in the classification. However, the complexity must be noted. Forty-two curve patterns are derivable by the application of the modifiers to the six basic curve types. The rotational component of the deformity was also not addressed. The Lenke system is currently the most widely utilized classification scheme for AIS and it thus provides a basis for comparison of treatments and outcomes [20].
2.2.4 Peking Union Medical College System
Qiu et al. at the Peking Union Medical College (PUMC) proposed this system of classification in 2005. They reviewed the records of 427 idiopathic scoliosis patients who were managed operatively over 18 years. The curves were assessed with the preoperative supine side-bending radiograph and anteroposterior and lateral standing radiographs taken before and after surgery. The SRS definitions of scoliosis and curve apex locations were strictly applied. The flexibility of the curvature was calculated thus: (Cobb angle on standing – Cobb angle on convex bending)/Cobb angle on standing} × 100 % [3]. The rotation of the apical vertebra was recorded from 1° to 4° using the Nash-Moe method [21].
This method was designed to enable the selection of a surgical approach and of fusion levels. All the curves were classified into single, double, and triple curves according to the apex vertebra, and these were termed types I, II, and III, respectively. There were a total of 13 subtypes.
Type Ia is a thoracic curve, Ib is thoracolumbar, and Ic, a lumbar curve. Type II consists of thoracic (T) and thoracolumbar/lumbar (TL/L) curves. Subtype IIa consists of double thoracic curves. In subtype IIb, the T curve is at least 10° > TL/L curve. For IIc, the difference between the Cobb angles of T and TL/L curves is <10°, while in IId, the TL/L is 10° > T curve. Further subdivisions of these subtypes are based on the differences in flexibility of the curves, presence of TL/L kyphosis, and its degree of axial rotation. Subtype IIIa consists of triple curves; its thoracolumbar/lumbar component has a Cobb angle of ≤45°, rotation <2°, flexibility ≥70°, and no kyphosis. In subtype IIIb, distal lumbar curve is larger and more rigid.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








