Fig. 37.1
(a) Facetectomy and pedicle screw cannulation. (b) Morselized bone graft prior to screw placement
Once the screws are placed at all levels, an appropriate length rod contoured to the appropriate sagittal profile is introduced. The rod is passed from distal to proximal below the soft tissues and under the skin bridges utilizing the elongated slots designed on the VIPER II cylinders (Depuy, J&J) (Fig. 37.2). The cylinders are made collinear prior to placement of the rod allowing for the majority of the deformity correction. The rod is reduced to the pedicle screws using the reduction instruments and secured using setscrews. Further correction is obtained with rod derotation into the appropriate sagittal plane. Prior to placement of the second rod en bloc, direct vertebral apical derotation is performed using the VIPER II cylinders. The second convex rod is then under-contoured in the sagittal plane and also placed from distal to proximal. Under-contouring of this rod allows for further deformity correction in the axial plane (Fig. 37.3). All rods are cobalt chrome and 5.5 mm in diameter. Uniaxial screws are primarily used (Fig. 37.4a, b).

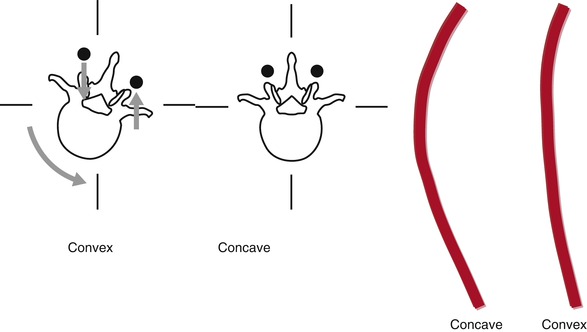
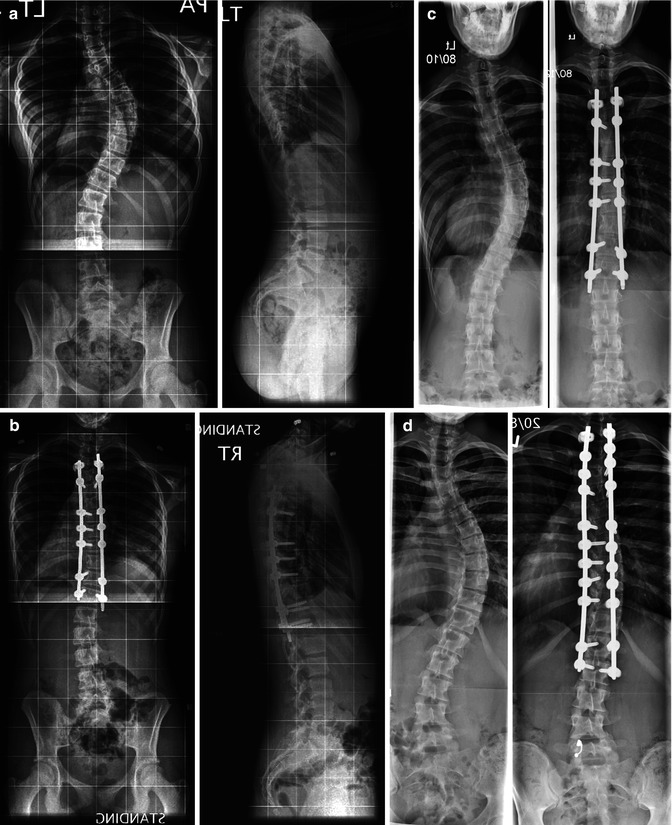


Fig. 37.2
Rod passage distal to proximal
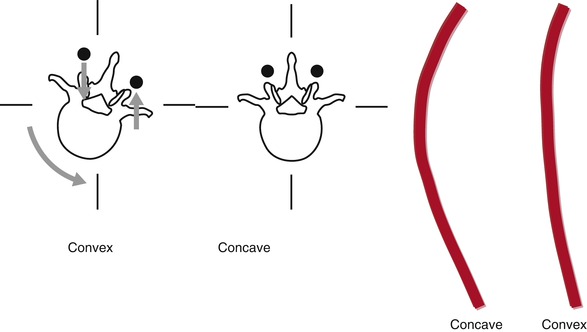
Fig. 37.3
Differential rod contouring (Courtesy Peter O. Newton)
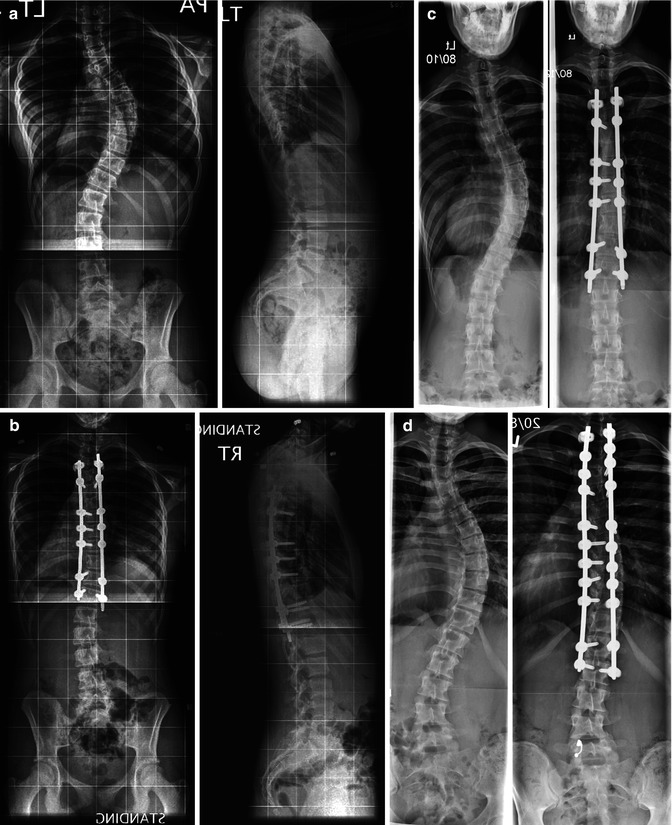
Fig. 37.4
(a–d) Pre and postoperative case examples of MIS in AIS

Fig. 37.5
Pre and 18 months post-operative clinical images. (a) Pre-operative clinical deformity, (b) Post-operative clinical result, (c) Pre-operative rib hump deformity, (d) Post-operative rib hump correction
Currently data focusing on outcomes of MIS techniques in AIS is limited. Anand and colleagues [25] reported on a series of 12 adult patients with degenerative scoliosis who had on average 3.64 segments fused. They reported a feasibility study in which patients underwent a lateral retroperitoneal approach followed by percutaneous pedicle screw placements. Functional or long-term data was not available in this series. Similarly Hsieh and colleagues [26] have described MIS procedures on a heterogeneous group of patients with complex spine disorders, but only one patient was treated for deformity. Samdani et al. [27] retrospectively reviewed their experience with MIS in 15 patients and had on average a preoperative major Cobb angle of 54° correcting to 18°, noting a 67 % correction. The average blood loss in their series was 254 cc and OR time was on average 470 min.
Our recent prospective comparison of MIS to open standard posterior techniques in the setting of AIS aimed at comparing curve correction and perioperative variables between the two groups [28]. The study found near-equivalent curve correction between the two groups (63 % open group; 68 % MIS group) (Fig. 37.5). The advantages of MIS over open posterior procedures were a significantly lower blood loss on average and decreased length of hospital stay. However, the operative time was significantly longer in patients treated with MIS. This may be the effect of a learning curve when applying new techniques but should be emphasized as a potential limitation of MIS in the setting of deformity.
37.3 Limitations and Future Trends
Curve correction, fusion, rod passage, and length of operative time have been raised as theoretical concerns of MIS. Although a number of deformity correction techniques exist for open procedures, not all are available to apply in the setting of MIS. There is greater emphasis on rod rotation, deferential rod contouring, distraction, compression, and intraoperative traction with MIS cases.
The fusion model in pediatric patients is different than adults and appears to be more favorable [29, 30]. However, fusion rates and/or time to fusion has not been reported for AIS treated with MIS techniques and should be the focus of much-needed prospective longer-term follow-up studies to assess these principal goals of AIS treatment and demonstrate the true clinical benefits of MIS in the setting of adolescent deformity.
The evolution of MIS as an effort to decrease the rate of approach-related morbidity associated with conventional open procedures certainly has shown potential for AIS at least in the short term, giving both surgeons and patients additional options to consider when planning surgical treatment for AIS.
References
1.
2.
3.
Newton PO, Perry A, Bastrom TP, et al. Predictors of change in postoperative pulmonary function in adolescent idiopathic scoliosis: a prospective study of 254 patients. Spine. 2007;32(17):1875–82.PubMedCrossRef
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








