Fig. 35.1
Intraoperative fluoroscopic image of K-wire insertion into the pedicle and vertebral body with overlying dilator

Fig. 35.2
Fluoroscopic image of screw placement after facet fusion

Fig. 35.3
Intraoperative photograph of the dilator over the facet joint

Fig. 35.4
View of the decorticated facet joint through the dilator tube

Fig. 35.5
Fluoroscopic image of the burr inserted through the dilator to the level of the facet joint
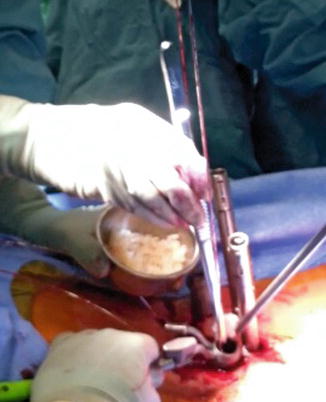
Fig. 35.6
Intraoperative photograph showing placement of bone graft through the dilator tube
35.4 Clinical Data
Most of the clinical data regarding facet-mediated fusions are based on open techniques [1, 3, 5–7]. King [1] described a fusion rate of 91 % in his original series of 55 patients, with only one patient experiencing nerve root irritation secondary to screw placement. Other surgeons [5], however, reported pseudarthrosis rates of up to 55 % with transfacet screw fixation using the King’s technique. Boucher [3], with his modified technique, reported a 100 % fusion rate in patients undergoing single-level fusion for degenerative disc disease and a 92 % fusion rate in patients undergoing fusion for spondylolisthesis. In more recent years, El Masry et al. [6] reported a 100 % fusion rate, with 89 % of patients in this cohort having excellent or good results and no neurological complications. Margulies and Seimon [7] similarly reported that 91 % of their patients had excellent clinical results after single-level fusion with the open Boucher technique.
Magerl’s variation of open transfacet fixation using a translaminar facet screw has also been shown to be a successful technique with few complications and favorable clinical outcomes [4, 8–11]. Jacobs et al. [8] reported a 91 % fusion rate with favorable clinical results in 93 % of their cohort undergoing lumbosacral fusion. Humke et al. [9] obtained a 94 % fusion rate using translaminar facet screw fixation for posterior fusion, achieving good or excellent clinical results in 97 % of their patients. One of 173 patients in this series had temporary quadriceps weakness that resolved within 6 months after fusion and decompression at L2−L3. Three of 173 had symptomatic nerve root irritation that resolved at minimum final follow-up of 52 months. Other studies [10, 11] using open translaminar facet fixation have reported fusion rates exceeding 94 % with good or excellent results achieved in a high percentage of patients.
Best and Sasso [12] also presented a cohort of patients who underwent circumferential lumbar fusion. The authors compared the reoperation rate of translaminar facet screw fixation with that of pedicle screw fixation. In this series, two of 43 patients (4.7 %) with translaminar facet fusion and none of 24 patients (37.5 %) with pedicle screw instrumentation required a second operation at the index level. Operative re-exploration revealed that the pseudarthrosis rate was 2.3 % in the translaminar facet screw population, compared with 4.2 % in the pedicle screw population. Interestingly, the single patient in the translaminar facet screw group with pseudarthrosis had additionally undergone an intertransverse process fusion, using pedicle screws, without removal of the facet screws. All patients in the pedicle screw group who underwent reoperation required removal of the screws and rods.
To date, no study of open or minimally invasive surgery has analyzed the results of performing thoracolumbar fusion with just a facet or mediated fusions with pedicle screws. Whether historical data regarding transfacet screw fixation with facet fusion is generalizable to minimally invasive facet fusions with pedicle screws is unknown. Thus, data to champion this technique as a viable option is based on anecdotal experiences.
35.5 Conclusion
With advances in minimally invasive spine surgery, percutaneous facet fusion is becoming an attractive alternative for posterior lumbar fusion. The percutaneous procedures offer numerous advantages compared with open techniques, including less blood loss [13–15], less soft-tissue disruption [16–18], less postoperative pain [16, 19, 20], and less risk of infection [14, 21, 22]. Radiation exposure is a concern; however, it can be minimized with virtual fluoroscopy and CT-guided techniques [23, 24].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








