Figure 10-1 A, A transverse T1 MRI scan showing bilateral, left greater than right sciatic nerve enlargement (arrow). B, An intraoperative photograph of the sciatic nerve showing enlargement taken at the time of fascicular biopsy.
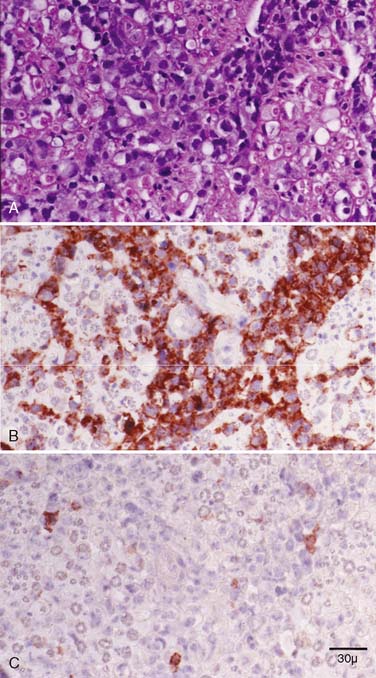
Figure 10-2 Serial paraffin cross sections of a fascicular sciatic nerve biopsy diagnostic of a large B-cell lymphoma. A, H&E shows many immature and large lymphocytes. B, CD-20 shows that the immature lymphocytes react to a B-cell marker but not (C) CD-3 to a T-cell marker.
(Reprinted with permission from Ghobrial IM, Buadi F, Spinner RJ, et al. High-dose intravenous methotrexate followed by autologous stem cell transplantation as a potentially effective therapy for neurolymphomatosis. Cancer 2004;100:2403-7.)
Initial therapy with dexamethasone, high-dose ARA-C, and cisplatin chemotherapy for two cycles failed to improve his symptoms. Repeat EMG demonstrated worsening of the severe axonal lumbosacral plexus neuropathies bilaterally. He subsequently received high-dose intravenous methotrexate (8 g/m2) every 2 weeks for a total of five cycles with significant improvement of his symptoms after the first dose. The patient then received high-dose therapy and autologous hematopoietic stem cell transplant (AHSCT) for recurrent diffuse large B-cell lymphoma and conditioning. On day 100 after the AHSCT, the patient had significant improvement in his strength with near-resolution of the severe neuropathic pain. His NIS had improved from 37 to 26 points. He had resumed his regular daily activities, including training in the martial arts. The patient remained in complete disease remission 6 months after AHSCT therapy.
CONCLUSION
PNL, a rare neurologic manifestation of systemic lymphoma, is characterized by lymphomatous infiltration of the peripheral nervous system.1 A review of 52 available case reports of PNL showed an equal male-to-female ratio. Seventy five percent of the patients were older than 50 years of age.1,2 All of the cases, except a single patient with Hodgkin’s disease,3 had non-Hodgkin’s lymphoma. Approximately one third of the patients had a history of lymphoma before the diagnosis of PNL. Approximately one half of the cases had widespread systemic lymphoma found at the time of autopsy, and 5% had central nervous system involvement.1,4
Most cases of PNL presented with a subacute progressive sensorimotor polyneuropathy. Less common presentations included cranial neuropathy, multiple mononeuropathy, and an isolated median or sciatic nerve palsy.4 Clinical findings that suggest PNL as opposed to paraneoplastic or inflammatory processes included severe pain, asymmetric distribution, and rapid evolution.5 An MRI of suspected involved segments of the neuroaxis is essential for diagnosis because it is able to indicate sites of the lesions and extent of involvement. Furthermore, MRI scans may show thickening, enlargement, and increased T2 signal of nerves involved and may help to identify potential sites for biopsy.6 MRI findings are not diagnostic, and targeted fascicular nerve biopsies are required to obtain diagnosis of these patients. Electrodiagnostic findings are diverse but typically there are some demyelinating features. However, axonal neuropathy is the most common finding on EMG.2 A premortem diagnosis can be confirmed by nerve biopsy. Approximately 83% of nerve biopsies in PNL are reported to demonstrate lymphomatous infiltration, whereas the rest may demonstrate only nonspecific findings.7 Suspicion of PNL warrants a multidisciplinary approach with a biopsy performed on a clinically or radiologically suspected nerve.
This case demonstrates that the peripheral nerve acts as a haven for lymphoma cells because most forms of chemotherapy do not cross the blood-nerve barrier, allowing tumor cells to survive. Consequently, it is fundamentally important to diagnose PNL since it has a different treatment. It is not sufficient to know that the patient has lymphoma; what is needed is to know that the patient has lymphoma in the peripheral nerve. As in this case, diagnosis usually requires a targeted fascicular nerve biopsy. Once the diagnosis is made, high-dose methotrexate (which crosses the blood-nerve barrier) and AHSCT may be the treatments of choice.2,8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








