Figure 8-1 The family history indicates autosomal dominant inheritance. Note multiple family members with high arches, tremor, or both.
(Reprinted with permission from Chahin N, Zeldenrust SR, Amrami KK, Engelstad JK, Dyck PJB. Two causes of demyelinating neuropathy in one patient: CMT1A and POEMS syndrome. Can J Neurol Sci 2007;34:380-5.)
On examination, he had +2 pes cavus, +2 pitting edema in his feet and ankle areas and hypertrichosis. No organomegaly or skin pigmentation was found. Mental status and cranial nerve examinations were normal. He had diffuse weakness in upper and lower extremities, moderate weakness in proximal muscles, and severe weakness in distal muscles. He was areflexic and had a panmodality sensory loss with pseudoathetosis of the fingers.
Extensive laboratory evaluation revealed a normal complete blood count, erythrocyte sedimentation rate, B12, folic acid, vitamin E, HbA1C, aspartate aminotransferase, angiotensin-converting enzyme, free thyroxin, prolactin, luteinizing hormone, follicle-stimulating hormone, antinuclear antibodies, extractable nuclear antigen (ENA), antineutrophilic cytoplasmic antibodies, rheumatoid factor, paraneoplastic antibodies, Lyme disease by enzyme-linked immunosorbent assay, hepatitis profile, human immunodeficiency virus serology, copper, zinc, heavy metal screen, and urine protein monoclonal study. There was mild elevation of his fasting blood sugar 119 mg/dL (70–100), thyroid-stimulating hormone 6.4 mIU/L (0.30–5), total testosterone 67 mg/dL (240–950) and a small monoclonal immunoglobulin A (IgA) Lambda on his serum protein monoclonal study. CSF analysis showed raised opening pressure to 250 mm H2O, protein 146 mg/dL (14–45), normal glucose, cell count, immunoglobulin G (IgG) synthesis, Lyme disease antibody screen, Venereal Disease Research Laboratory (VDRL), and cytology.
Metastatic radiographs showed sclerotic lesions in the right transverse process of the first thoracic vertebrae and left neck and the body of the scapula. A computed tomography (CT) scan showed additional sclerotic lesions in the left occipital bone and enlarged left axillary lymph node (Fig. 8-2). A 3-tesla magnetic resonance imaging (MRI) scan of the pelvis with special attention to the lumbosacral plexus demonstrated increased size and hyperintensity involving all of the portions of the lumbosacral plexus with markedly enlarged L4 and L5 nerve roots. With contrast, there was mild to moderate enhancement. The MRI also showed a sclerotic lesion within the left ilium and multiple enlarged lymph nodes in the pelvis (see Fig. 8-2).
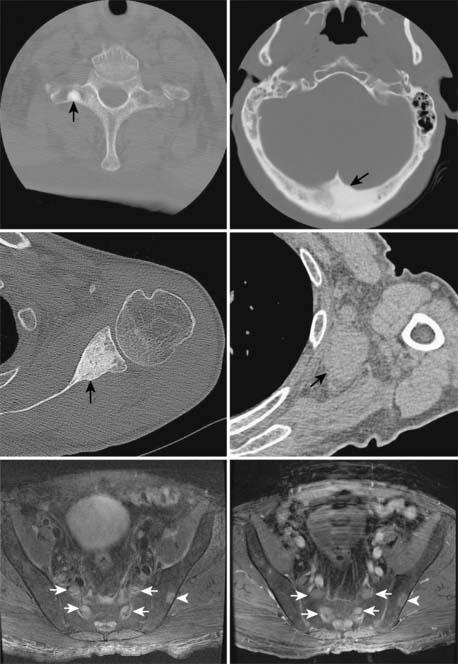
Figure 8-2 Computed tomography scan showing multiple osteosclerotic lesions in the right transverse process of T1 (upper left, arrow), left occipital bone (upper right), neck and adjacent body of the left scapula (middle left, arrow), and an enlarged left axillary lymph node (middle right). Magnetic resonance imaging scan of the pelvis (lower left and right) showing enlargement and increased T2 signal of the lumbar roots (arrows); it also shows an additional sclerotic lesion in the ilium (arrowhead).
(Reprinted with permission from Chahin N, Zeldenrust SR, Amrami KK, Engelstad JK, Dyck PJB. Two causes of demyelinating neuropathy in one patient: CMT1A and POEMS syndrome. Can J Neurol Sci 2007;34:380-5.)
A contrast-enhanced abdominal CT showed borderline periaortic lymphadenopathy and moderate diffuse edema of the subcutaneous and intra-abdominal fat, but no hepatomegaly or splenomegaly. Bone marrow biopsy was normal.
Electrophysiologic studies showed absent right tibial and peroneal motor responses and absent sural, ulnar, and median sensory responses. The right ulnar motor amplitude was reduced to 0.1 millivolts, with markedly slowed conduction velocity of 8 ms and prolonged distal latency of 16.9 ms. The musculocutaneous motor has amplitude of 0.3 mV with slowed conduction velocity of 7 m/s and markedly prolonged distal latency of 16.6 ms. The ipsilateral R1 and R2 responses of the right trigeminal were markedly prolonged at 37.7 ms (8–13) and 61.5 ms (29–41), respectively, with a prolonged contralateral R2 response of 59.2 ms (29–44). Needle EMG showed sparse fibrillation potentials and marked reduced recruitment of mildly to moderately long duration, high amplitude complex motor unit potentials diffusely including the lumbar and thoracic paraspinal muscles.
A left sural nerve biopsy showed severely decreased density of myelinated fibers in diffuse pattern, an altered size distribution with selective loss of large fibers, thinly myelinated fibers, dense generalized onion bulbs, and increased numbers of empty nerve strands. There were a few small collections of perivascular epineurial mononuclear cells and an increased number of endoneurial macrophages seen. Smooth muscle actin (SMACTIN) showed extensive neovascularization in the epineurium (Fig. 8-3).
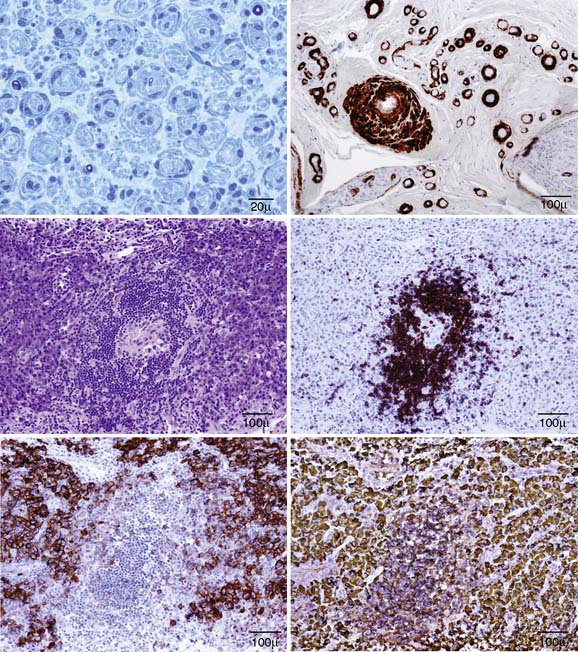
Figure 8-3 Left sural nerve biopsy (upper left and right). There is extensive generalized hypertrophic onion bulbs in semithin epoxy sections and severe decreased density of myelinated fibers and a few remaining small thinly myelinated fibers (upper left). Smooth muscle actin immunostaining (SMACTIN) of transverse paraffin sections (upper right) show extensive epineurial neovascularization. Serial sections through an axillary lymph node biopsy showing germinal follicle (middle left, H&E) composed of B cells (CD20) (middle right), surrounded by plasma cells (CD138) (lower left), which show Lambda light chain restriction pattern (lower right). The findings are consistent with Castleman’s disease.
(Modified and reprinted with permission from Chahin N, Zeldenrust SR, Amrami KK, Engelstad JK, Dyck PJB. Two causes of demyelinating neuropathy in one patient: CMT1A and POEMS syndrome. Can J Neurol Sci 2007;34:380-5.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








