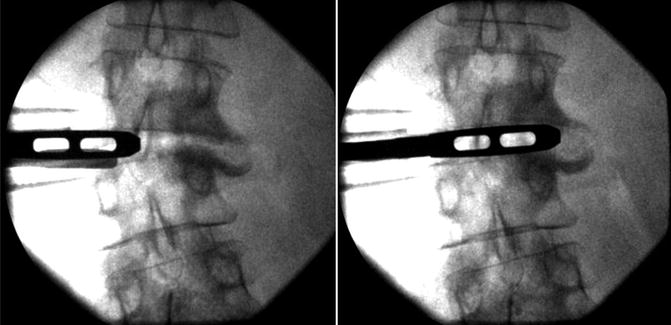
Fig. 27.1
Serial dilators and the retractor itself are each inserted utilizing EMG neuromonitoring to detect nerve proximity and location thus minimizing the risk of neural injury during psoas transgression
Although rare, the motor nerve injuries could happen during the minimally invasive lateral interbody fusion procedures. Cahill et al. reported a single-center experience of 118 consecutive patients who underwent lateral interbody fusions at 201 lumbar intervertebral disc levels. The authors noted 4.8 % injury risk of femoral nerve at the L4–L5 level and 0 % injury risk at other lumbar spine levels [2]. At the L4–L5 disc space, the lumbosacral plexus is more anterior compared to other disc levels. The femoral nerve can be located as far anteriorly as the midpoint of the disc space at L4–L5 [20], explaining the higher risk of femoral nerve injury at L4–L5 levels during minimally invasive lateral approaches.
In the same article, Cahill et al. also documented a 4.2 % incidence of postoperative abdominal flank bulge [2]. Similarly, Dakwar et al. reported a 1.8 % incidence of abdominal wall paresis after minimally invasive lateral transpsoas interbody fusion [5]. Most of the patients with abdominal wall paresis resolved at the 6-month follow-up visit. Fahim et al. performed a detailed anatomical analysis to study the etiology of abdominal flank bulge after anterolateral approaches to the thoracolumbar spine [7]. They found that T11 and T12 intercostal nerves are the major contributions to the anterolateral abdominal wall innervation. The occurrence of postoperative abdominal flank bulge is most likely due to muscle denervation caused by T11 and T12 intercostal nerves injury. The authors speculated that the nerves could be injured during the rib dissection to gain access to the upper level of the lumbar interbody space, from the crush or stretch injury when retractor is used to expand the intercostal space or during dissection of the three layers of the abdominal musculature, especially when Bovie electrocautery is used for the dissection through the muscle layers.
While the spine surgeon is acutely aware of the potential for neurologic injury during surgery, perhaps the most devastating complications of the lateral transpsoas interbody fusion procedure are injuries to the vascular and visceral contents of the retroperitoneum. Regardless of the side of approach, the colon and great vessels lie in close proximity to the ventral spinal column – the ascending colon and inferior vena cava (IVC) on the right and the descending colon and aorta on the left. Anterior mobilization of the peritoneal contents through the posterolateral incision is the first and most critical step upon entry into the retroperitoneum, and – particularly in very thin patients and in the setting of significant rotational deformity – these viscera are frequently seen and/or felt along the surgical corridor.
Bowel injury is most likely to occur as a result of sharp division of the transversalis fascia, excessively vigorous blunt dissection of the peritoneum, or pincer action of the retractor blades. Even when recognized intraoperatively, injury to the colon is a potentially disastrous complication, frequently necessitating the performance of a diverting colostomy and close observation for development of a retroperitoneal abscess. The consequences of occult bowel injury may be catastrophic [19] (Fig. 27.2). The kidneys are also at risk during exposure and transit of the retroperitoneal space and may be injured as a result of sharp entry into the retroperitoneum at the more rostral levels of the lumbar spine or excessive retractor opening [9]. Finally, the ureters travel on the ventral surface of the psoas muscle and, particularly in the setting of rotational deformity, may be encountered during retractor placement.
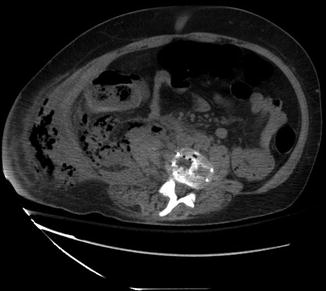
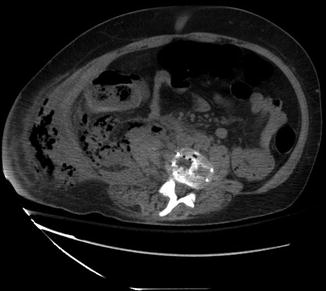
Fig. 27.2
An unappreciated descending colon injury with fecal extravasation into the retroperitoneal space led to catastrophic sepsis. An acute abdomen did not present due to the containment of the contents within the retroperitoneal cavity; thus, bowel injury can remain relatively silent for days following injury
Similarly, injury to the great vessels during the lateral approach has been reported and carries with it the potential for massive intraoperative blood loss, postoperative retroperitoneal hematoma with or without hemodynamic instability, and delayed pseudoaneurysm formation [17, 19]. The great vessels are at risk particularly in the setting of severe rotational deformity, in which the vessels are often displaced from their typical locations anterior to the spine. Injury may result from aggressive dissection along the ALL or from pincer action of the retractor against the spine. Also at risk – particularly with excessive opening of the rostral and caudal blades of the retractor – are the segmental spinal arteries. Although injury to the segmental arteries is much less likely to be hemodynamically significant, and rarely has any consequences for spinal cord perfusion (except perhaps at L1), it remains a potential source of intraoperative bleeding and, if not controlled, of postoperative retroperitoneal hematoma [11, 18].
At the thoracolumbar junction, the thoracic cavity replaces the retroperitoneum in the approach to the ventral spine. Violation of the parietal pleura is common during the dissection and typically does not require specific management. The visceral pleura is, however, occasionally breached and if the defect is significant should be treated with placement of a small chest tube. Even in the absence of a large recognized defect, a pleural effusion or hemopneumothorax may develop postoperatively and, when significant, requires placement of a draining catheter [9, 19].
Avoidance of approach-related complications begins prior to incision, ensuring that the patient is positioned so that a true lateral image and an anteroposterior image are projected with the fluoroscope at right angles to the floor. This decreases the likelihood of bringing the abdominal viscera further into the operative corridor. When planning the incision(s), it may be advantageous to consider the local pattern of Langer’s lines as the risk of transection of cutaneous nerves – and of the postoperative flank and anterior abdominal wall dysesthetic pain syndromes thought to result therefrom – may be less when the incision(s) are made parallel to these lines. Next, confirmation of proper entry into the retroperitoneum is critical, facilitated by careful preoperative review of magnetic resonance or computed tomography imaging. The authors utilize the posterolateral incision in most lateral approach cases (and in all cases involving rotational deformity) and emphasize the importance of blunt finger dissection at a 45° angle to the plane of the spine, so as not to lose one’s orientation and risk entrapment of peritoneum. Passage through the transversalis fascia and into the retroperitoneum is typically achievable without the need for sharp dissection, avoidance of which may limit the risk of injury to the retroperitoneal viscera. Thorough, gentle mobilization of the peritoneal viscera anteriorly, away from the operative corridor, is critical.
As an additional protection against the development of infectious complications in the event of a bowel injury, a preoperative bowel preparation may be considered. Given the extremely low incidence of bowel injury reported thus far [9, 15, 16, 19], this is probably only necessary for complex cases, such as in the setting of significant deformity.
After the flank incision is made, careful blunt dissection to connect the two corridors will permit safe descent of the dilators onto the psoas muscle. Some surgeons advocate direct inspection of the psoas in the depths of the corridor by temporary insertion of the retractor, prior to dilation of the psoas. This additional step may allow the surgeon to better plan his initial entry into the psoas muscle so as to avoid the genitofemoral nerve. During dilation of the psoas muscle, real-time, directional EMG monitoring should be used to safely position the retractor away from the nerve roots. An in-depth understanding of the position of the lumbar contributions to the lumbar plexus within the psoas muscle is critical if injury to the plexus is to be avoided during retractor placement. Elegant cadaveric and radiographic studies have demonstrated that these contributions become progressively more ventral as one proceeds caudally down the lumbar spine and have defined safe working zones at each level [1, 8, 20]. Even with avoidance of direct trauma to the neural elements, however, the roots and proximal portions of the lumbar plexus are at risk of stretch injury from excessive retractor opening. For this reason, it is advisable to open the retractor blades only enough to permit the discectomy and graft insertion, which also helps to avoid injury to the segmental arteries and psoas muscle (Fig. 27.3). Once the retractor is docked on the lateral annulus, proper orientation should again be confirmed with an anteroposterior fluoroscopic image. Any soft tissue remaining in the depths of the field should be carefully dissected away, using an EMG-equipped ball-tipped probe to ensure that no neural elements have crept into the field during retractor manipulation and placement.
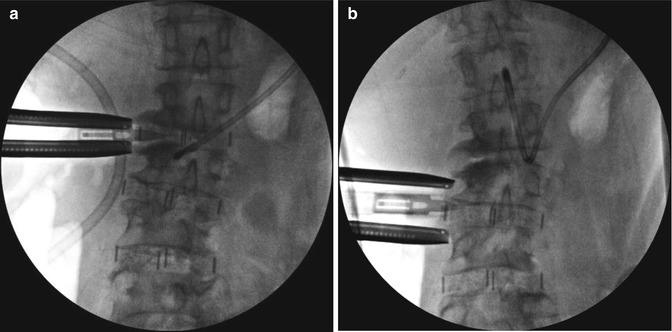
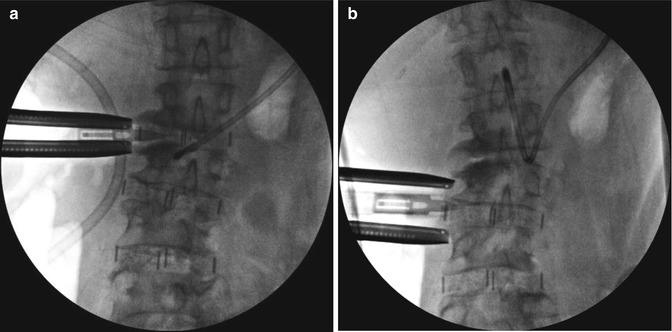
Fig. 27.3
It is important to (a) limit the rostral-caudal retractor blade opening to only what is necessary to successfully complete the discectomy and implant the cage; (b) excessive blade retraction can lead to injury to the psoas muscle, lumbar plexus, segmental arteries, and other vital structures that lie within and adjacent to the lateral spine
27.3 Complications Encountered During Discectomy and Graft Placement
The main concern during discectomy and graft insertion is for violation of the bony vertebral end plate(s) and disruption of the ALL with the attendant risks of graft malposition, subsidence, and migration. Also worthy of mention, however, is the potential for many of the injuries – previously discussed in the context of the exposure and retractor placement – to occur on the contralateral side as a result of maneuvers during the discectomy and graft insertion steps of the procedure. It is essential, using fluoroscopic imaging if necessary, to remain aware at all times of the depth of insertion of the instruments used during the discectomy. This is particularly true when using the Cobb elevator to open the contralateral portion of the annulus fibrosus and break any bridging anterolateral osteophytes (Fig. 27.4), which risks injury to the contralateral nerve root and psoas muscle and may lead to the development of a contralateral retroperitoneal hematoma [13]. All of the visceral structures discussed in the preceding section – including the ureter, kidney, pleura, lung parenchyma, and great vessels – might theoretically be injured on the side opposite the approach, particularly in the setting of rotational deformity.