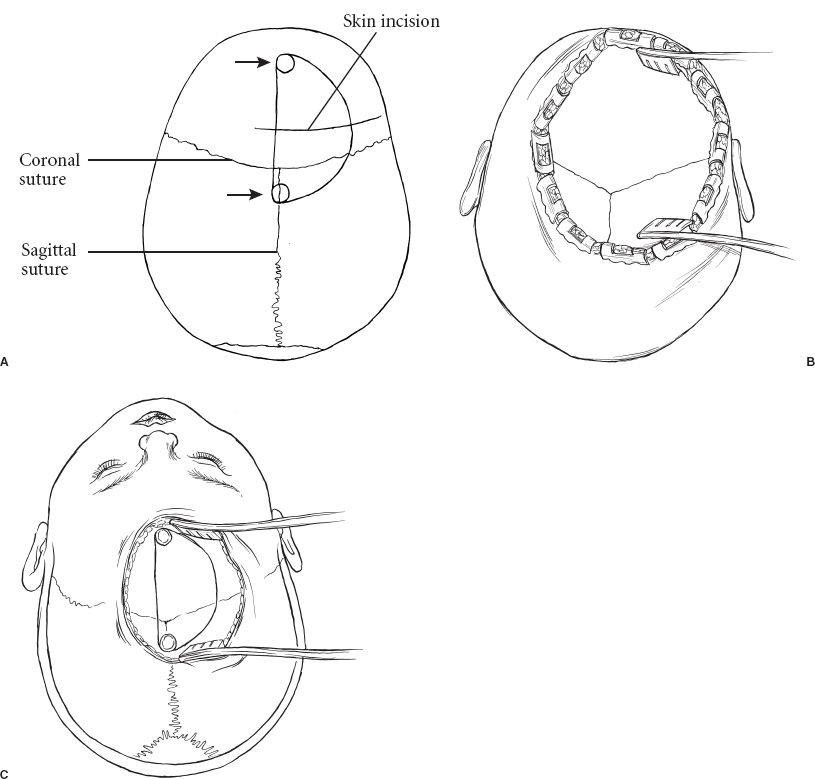
Corpus callosotomy originally was designed for medically intractable epilepsy patients with secondary generalization of focal seizures, in whom cortical resection of the seizure focus is not feasible. In addition, beneficial effects can be seen in children with generalized seizures in whom electroencephalography (EEG) demonstrates simultaneous bilateral sites of onset. Unlike other surgical therapies for epilepsy in which the epileptic focus is identified and removed, callosotomy interrupts the propagation of epileptic discharges, resulting in a truly functional procedure with the target being a physiological process rather than a pathological lesion. Conceptionally, severing the major connection between the hemispheres might logically reduce the generalization of a unilateral seizure focus. The benefit for patients with bilateral onset of epileptigenic activity is more difficult to explain, but it may result from global diminution of synaptic connectivity within the cerebrum. This “synaptoreduction” also may help to explain the observation that postoperative EEGs rarely demonstrate well-lateralized foci of seizure activity, which might be expected if corpus callosotomy simply prevents propagation of epileptic activity between the hemispheres. The surgical technique is relatively straightforward and is associated with minimal morbidity and mortality. A few patients develop an acute disconnection syndrome characterized by mutism, nondominant left-arm and left-leg apraxia, inattention, bilateral Babinski signs, and urinary incontinence, although fortunately these symptoms typically resolve quickly. Postoperative hydrocephalus can largely be avoided by careful attention not to violate the ventricular system. Long-term seizure control in postcallosotomy patients is difficult to ascertain because without generalization, many postoperative seizures may be sub-clinical. Few studies report sophisticated outcome analysis and quality-of-life measures, which are likely superior to seizure frequency in assessing the efficacy of callosotomy. Recent series have been encouraging, however, with 56 to 100% of patients experiencing significant improvement in the frequency of generalized seizures. Although predicting which patients will benefit from a callosotomy remains difficult, it is clear that patients with “drop” attacks derive the most benefit from the procedure. The goal of this operation is not to make the patient seizure free but to improve quality of life and function. The clinical indications for callosotomy continue to evolve with the development of newer investigational and therapeutic techniques. In particular, many centers are inserting vagal nerve stimulators (VNS) in most patients with seizures previously treated with callosotomy. The long-term outcome with this treatment strategy remains unknown, although many of these patients may undergo callosotomy secondarily if generalized seizures persist. Most centers consider callosotomy a safe and effective treatment for selected patients with intractable, debilitating, generalized seizures. In particular, atonic–tonic seizures, or “drop” attacks, are accepted as the most responsive seizure type. The role of callosotomy in partial epilepsy is controversial, with dramatically varying results in different centers. At Children’s Hospital in Boston, patients unresponsive to adequate trials of multiple antiepileptic medications with an absence of a resectable seizure focus are considered for callosotomy if there exist: (1) the presence of incapacitating generalized seizures causing drop attacks or interfering significantly with quality of life; (2) recurrent episodes of convulsive or nonconvulsive status epilepticus; or (3) a desire to lateralize a frontal lobe focus where long-term EEG monitoring is inconclusive. The first two groups of patients are also good candidates for VNS, which we presently prefer as an initial procedure. Because roughly 50% of patients with VNS continue with intractable seizures, many patients may benefit secondarily from a callosotomy. Contraindications include an inadequate trial of antiepileptic agents, nondebilitating seizure pattern, or surgically accessible seizure focus. In addition, if there is a focal lesion that could lead to a new neuropsychologic deficit if combined with division of the corpus callosum, or if significant language function resides in both hemispheres, a callosotomy usually is not performed. The presumed developmental potential of the child is our primary criterion for selecting a patient for a single-stage complete callosotomy rather than an initial anterior callosotomy. A partial callosotomy can be followed by a second procedure to complete the division of the corpus callosum if significant seizures persist. Whereas severely impaired children clearly have less morbidity with a single-stage procedure, the risks of a postcallosotomy disconnection syndrome often outweigh the advantage of a single-step procedure in patients who are expected to be able to read and live independently. There are no data to suggest that a complete callosotomy performed in two stages is more or less effective in dealing with seizures than a single-stage procedure. The preoperative evaluation includes EEG monitoring to demonstrate sites of seizure origin as well as high-quality magnetic resonance imaging (MRI) to identify structural lesions that may be associated with epileptic activity. The MRI is also valuable for operative planning in defining the anatomy of the corpus callosum and its surrounding vasculature. A Wada test, consisting of intracarotid sodium amytal injection, is performed when there is a possibility of significant language function residing in the nondominant hemisphere for handedness, as seen with mixed or crossed language dominance. Ictal and interictal studies of metabolism or blood flow are used by some centers as confirmatory data to localize areas of seizure activity. Formal neuropsychologic evaluation should be obtained when possible. As with all major surgery, the patient must be evaluated carefully for previous medical problems or physical findings that might complicate the intraoperative or postoperative course. A complete history and physical examination including appropriate blood work is vital to ensure the highest level of safety for the patient. Certain antiepileptic medications are known to interfere with coagulation, and some centers stop administering agents such as valproic acid several weeks prior to surgery. Careful discussion of the procedure, alternatives, possible complications, and likely results must be held with the parents and patients of sufficient age to participate in the decision. Anterior callosotomy and single-stage complete callosotomy are performed with the patient under general anesthesia with the usual monitoring required for such a procedure, including adequate venous access, blood pressure monitoring, Foley catheter, and cardiac Doppler to detect air embolism. These children are often sensitive to narcotics and other central nervous system depressants even before the callosotomy is performed. As a result, we minimize the intraoperative and postoperative use of these medications. Intraoperative corticosteroids are not routinely used, although osmotic diuresis with mannitol or mild hyperventilation can minimize the degree of brain retraction required. Patients continue taking preoperative anticonvulsant medication except when that medication might interfere with coagulation. Prophylactic antibiotics are administered prior to the incision and every 6 hours during the procedure. The patient is positioned supine with the head elevated and slightly flexed (Fig. 23–1). We use a 10-cm linear incision parallel, and 2.5 cm anterior to the coronal suture, centered 2 cm to the right of midline (Fig. 23–2). Two burr holes are placed on the midline, one located at or just posterior to bregma, the confluence of the coronal and sagittal sutures, and the other 5 cm anterior to bregma (Fig. 23–2). A trapezoidal or D-shaped craniotomy is made with a high-speed drill. To achieve true midline visualization of the corpus callosum, it is vital that the bone flap comes to or slightly past the midline of the sagittal sinus. If the sinus is firmly adherent to the bone, the edge of the craniotomy should be placed slightly to the left of the sinus to avoid inadvertent injury. FIGURE 23–1. The patient is positioned supine with slight flexion of the neck. If the patient is older than 1 year, the head is placed in pin fixation.
SURGICAL INDICATIONS
PREOPERATIVE MANAGEMENT
INTRAOPERATIVE TECHNIQUE

![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


