44 Costotransversectomy
I. Key Points
– Conservative management of thoracic disc herniation with radiculopathy is the preferred primary management.
– The presence or progression of myelopathy due to thoracic disc pathology is accepted as an indication for surgery.
– Costotransversectomy is best suited for ipsilateral noncalcified central pathology and is contraindicated for contralateral decompression and large central calcified disease.
– Costotransversectomy provides a well-tolerated surgical corridor to address ventral and ventrolateral pathology via a posterior approach, but care must be taken in working around the neural structures.
– Excellent choice for patients who cannot tolerate anterior approaches via thoracotomy
II. Indications
– Drainage of spinal abscess/infections (originally described for tubercular abscess by Ménard)
– Spinal decompression of ventral and ventrolateral space-occupying lesions2–4
– Resection of paraspinal nerve sheath tumors2,3
– Correction of kyphotic deformity2
III. Technique (Fig. 44.1)
– Position patient prone or partial lateral. Incision can be paramedian, T-shaped, straight, or curvilinear with convexity toward the midline to allow for greater access.
– The incision is carried through skin, trapezius, and/or latissimus dorsi (for lower approaches) and erector spinae with medial retraction to expose the ribs and transverse process of the caudal vertebrae of the level of interest.
– Subperiosteal dissection of the perichondrium around the rib is performed, protecting the pleura and neurovascular bundle (use a semisharp subperiosteal dissector such as a Doyen rib raspatory).
– After sharp division of the costotransverse ligament, the transverse process is removed at the junction with the lamina using rongeurs or a high-speed drill.
– Transection of the rib about 3 to 5 cm (depending on the exposure needed) from the costotransverse junction and disarticulation of the rib from the costovertebral joint is then performed.
– Partial laminectomy and facetectomy are carried out to identify the lateral margin of the dura using a high-speed drill and/or small Kerrison rongeurs.
– The pleura may be protected ventrally with a malleable retractor, and a rib spreader may be used to increase exposure depending on number of levels indicated.
– Careful dissection along the superolateral border of the pedicle can be performed to safely expose the vertebral body or identify the disc space, depending on the goals.
– Discectomy should be performed laterally first, followed by the creation of a cavity centrally that can be used to push mediodorsal pathology inward to facilitate safe removal without manipulation of the spinal cord. This cavity may be enlarged to include partial vertebral resection as needed.
– If vertebral column resection is to be performed, then a midline approach with or without T-shaped extension is best to allow for safe instrumentation.
– If the spine is to be destabilized due to vertebral column resection, posterior instrumentation with gradual reduction of kyphosis using temporary rods should be done first.
– During closure, the field should be flooded with irrigation and a Valsalva maneuver performed to identify any pleural compromise. If pleura is violated, primary repair should be attempted with or without placement of a chest tube.
– The wound should be closed in layers and drains placed as needed.
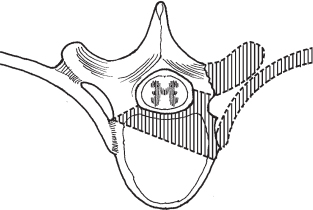
Fig. 44.1 Cross-section of the costotransversectomy approach. The shaded area depicts bone that may be removed using this approach to expose the spinal canal. (From Vaccaro AR, Albert TJ, Spine Surgery: Tricks of the Trade 2nd ed, Thieme; pg. 86, Fig. 24.3.)
IV. Complications
– Highly dependent on pathology and procedure performed
– Neurologic decline (5.5%), neurovascular bundle compromise, hemothorax
– Pneumothorax (as high as 25%), injury to pleura, lung contusion, atelectasis2–4
– Dural tear, symptomatic or asymptomatic pseudomeningocele
– Infection
– Injury to great vessels lying anterior to vertebral body
– Injury to radiculomedullary arterial branches, leading to spinal cord infarct
V. Postoperative Care
– Chest x-ray should take place in recovery room to evaluate for pneumothorax.
– Patient should be placed in a monitored unit with continuous pulse oxymetry performed.
– Incentive spirometry and pulmonary toilet are key in the postoperative period.
– Pain should be adequately controlled to prevent guarding and shallow breathing.
– Early mobilization with standard spinal postoperative care (e.g., deep vein thrombosis [DVT] prophylaxis)
VI. Outcomes
– Improvement in weakness ranging from 30 to 58%
– Improvement in radiculopathy or local pain ranging from 42 to 91%
– Spasticity and myelopathy improvement has been reported as high as 95%.
– Comparing costotransversectomy with anterior or combined approaches for treatment of oncologic disease, the perioperative complication profile is similar, but a posterior approach may be better tolerated in patients with multiple medical comorbidities.
VII. Surgical Pearls
– The spinal cord should never be manipulated to gain exposure.
– If the goal of surgery is anterior column resection, then posterior instrumentation should be placed with a temporary rod prior to destabilization of the vertebral column
– Following the neurovascular bundle back will lead to the neural foramen, and the removal of the rib head leads to the disc space of interest.
– If more exposure is needed one should remove more rib, allowing a greater lateral corridor, rather than trying to work via a more posterior approach.
Common Clinical Questions
1. With central thoracic disc herniations, what side is preferred for performing a costotransversectomy approach if indicated?
2. What is the origin of the major arterial supply to the spinal cord from T8 to the conus, and where is it located?
3. During positioning, what is a useful anatomic landmark for the T7 vertebral level?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







