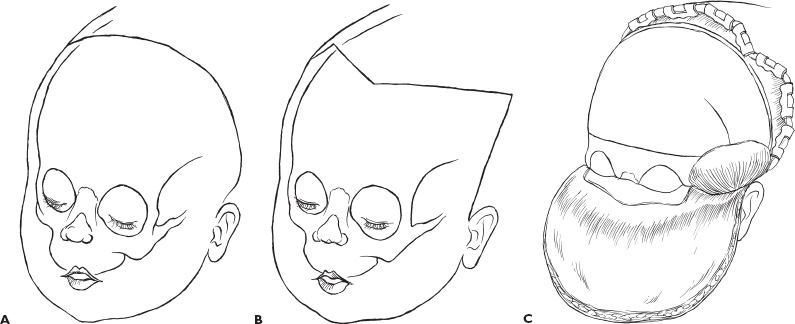
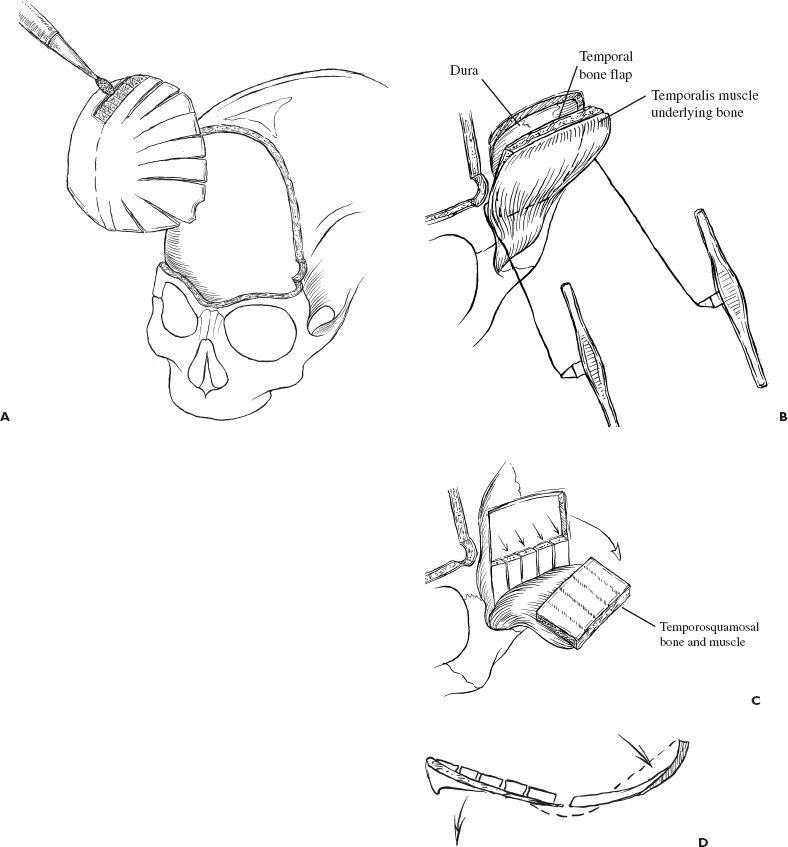
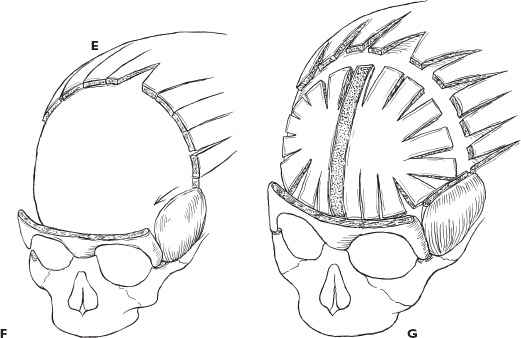
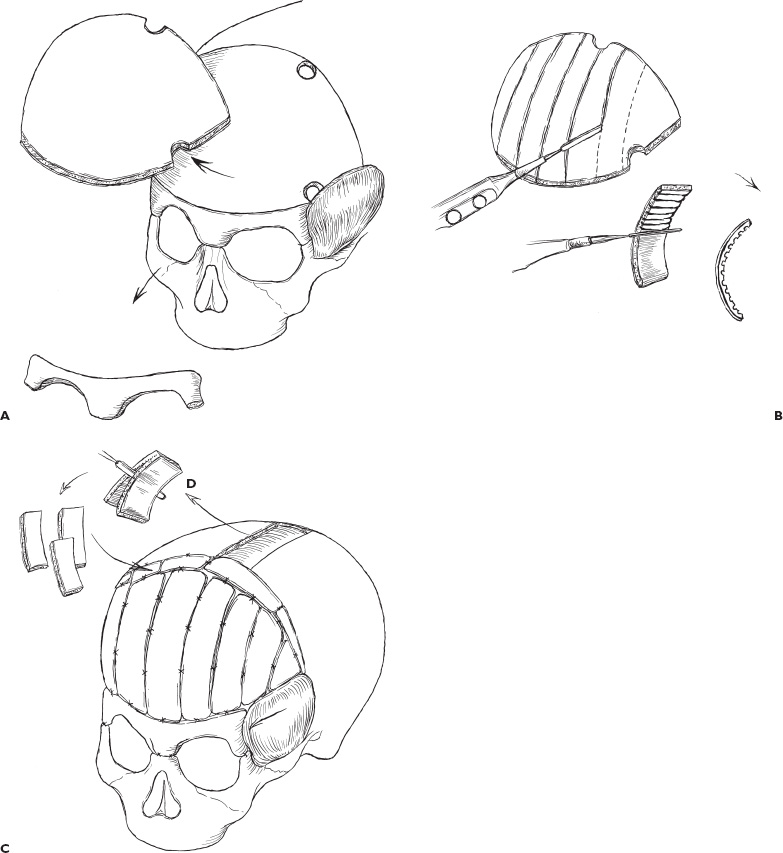
The treatment of craniosynostosis has evolved dramatically over the last 50 years. Linear-strip craniectomies were the first treatment approaches used to release synostotic cranial sutures. This approach was effective in young children who had not yet developed prominent compensatory cranial vault and base abnormalities. In children who had developed these abnormalities, however, incomplete correction of the skull deformities was seen regularly. Various techniques using foreign interposing material or application of caustic agents to the dura were used to prevent refusion of the suture, the mechanism thought to account for the variable success of the strip craniectomy procedures. Further modifications were developed in reshaping hypoplastic areas of the skull, such as the orbits, to improve the overall appearance. These techniques improved results, but it became clear that the existence of compensatory bulging skull deformities continued to constitute significant residual deformities. To achieve a normal skull form, bilateral and eventually holistic craniofacial approaches have been developed to correct all significant abnormal dimensions. Currently, surgical approaches focus on releasing the synostosis, reshaping the bone, and achieving as normal a correction as possible with direct reconstruction of compensatory deformities. The diagnosis of primary nonsyndromic craniosynostosis is based on the characteristic skull shape: Metopic synostosis causes trigonocephaly, unilateral coronal synostosis causes an anterior plagiocephaly, bilateral coronal synostosis causes brachycephaly (turribrachycephaly), sagittal synostosis causes scaphocephaly, and lambdoid synostosis causes a posterior plagiocephaly. Combinations of these pathologies may be evident if the individual forms occur in combination with another. The deformity is usually present at birth and becomes more exaggerated over time. Skull-shape abnormalities also can result from deformational forces such as compression or positional molding, which are much more common than true craniosynostosis. The overwhelming majority of posterior plagiocephaly is from molding. The skull shapes in these situations differ distinctively from the characteristic shapes of craniosynostosis. Positional (posterior) plagiocephaly is characterized by a parallelogram-shaped head when viewed from above and typically improves as the child develops motor skills to mobilize the head. Radiographic evaluations assist in the diagnosis. The characteristic skull shapes of craniosynostosis are easily recognized on computed tomography (CT) and bony bridging across a suture can be seen. Three-dimensional (3-D) CT reconstruction provides particular clarity in defining the full extent of the deformity. The recommendation for surgery in craniosynostosis is based on aesthetic and functional considerations. Prominent craniofacial deformities from craniosynostosis can affect a child’s psychosocial development significantly. For many parents and surgeons alike, the psychosocial benefits of early corrective surgery outweigh the low risk of modern craniofacial surgery. In addition, there is also evidence that single-suture synostosis can have an effect on intracranial dynamics, and children with uncorrected simple craniosynostosis must be monitored actively for signs and symptoms of elevated intracranial pressure. A multidisciplinary evaluation is performed preoperatively in patients with craniosynostosis. Genetic counseling and testing assist the family in understanding the full spectrum of potentially associated problems. Neuropsy-chologists assess and follow the child’s developmental status when there is clinical suspicion of developmental delay (or, in older children, psychological stress). Visual acuity, and the presence of papilledema, diplopia, or strabismus are tested by an ophthalmologist. A social worker or psychological therapist may be instrumental in assessing the family’s expectations. Radiographic evaluation centers on the head CT with 3-D bony reconstruction, which delineates the full extent of the deformity for presurgical planning. Attention is also given to the cerebrospinal fluid (CSF) spaces and ventricular size to rule out coexisting hydrocephalus. When a modified prone position is planned to gain simultaneous access to the anterior and posterior portions of the skull, cervical spine films are taken to exclude the presence of craniocervical abnormalities that might lead to brainstem or spinal cord injury during extension of the neck. In patients with syndromic synostosis or multiple suture involvement, magnetic resonance (MR) imaging is also appropriate to rule out an associated Chiari malformation. If a craniocervical abnormality is discovered, the patient would not be placed in the modified prone position but would be operated on serially on the same day with a two-stage operation, initially with the patient in a supine position and then in a prone position to correct both posterior and anterior abnormalities of the skull. Standardized photographs are taken preoperatively and serve as a baseline for outcome assessments. Longitudinal follow-up for at least 5 years is recommended. Early assessments of surgical efficacy are not complete until the facial skeleton has undergone additional development, particularly in patients who have asymmetric skull deformities such as unilateral coronal synostosis. With these developments in the facial skeleton, either amelioration of any postoperative deformity or recreation of the preoperative deformity may be seen. The major intraoperative concern in craniosynostosis surgery is the potential for blood loss and air embolism, which must be anticipated preoperatively by securing adequate amounts of blood for the patient and arranging appropriate monitors for surgery. All patients undergoing surgery receive a central intravenous line, large-bore peripheral venous lines, arterial line, Foley catheter, pre-cordial Doppler, and end-tidal CO2 monitor. The patient is also volume expanded with a 10 to 15 cc/kg crystalloid intravenous bolus prior to skin incision to decrease the risk of air emboli and cardiovascular collapse. Detection of possible air emboli by the Doppler or end-tidal CO2 is immediately followed by copious irrigation of the field, Trendelenburg positioning, and waxing of all bone edges. Rarely is the blood loss acute and rapid, although it may occur from tears of the sagittal or transverse sinuses. Extreme care must be taken when dissecting the sinus under a nonfused suture because it is regularly adherent. A more common observation is that there is a continuous low-grade, small amount of blood loss that occurs throughout the operative procedure. Because the circulating blood volume of the infant is relatively meager, even small amounts of blood loss assume greater importance. The surgeon can minimize blood loss by injecting local anesthetic with epinephrine in the anticipated incision line to achieve meticulous homeostasis on opening, dissecting in the supraperiosteal plane to minimize blood loss from the bone, and waxing all edges of bone when cut. Prompt replacement of fluid losses is also critical to maintaining hemodynamic stability. Controlled hypotension also can be employed intraoperatively to minimize blood loss. Nevertheless, blood replacement is routine. Intraoperatively, the coagulation status and platelet count are monitored. A continuing dialogue between the surgeon and anesthesiologist is helpful for optimal intraoperative management. Surgical technique is tailored to the type and severity of craniosynostosis as well as to the age of the patient. Various techniques have been described for each type of craniosynostosis. The occasional patient younger than 6 weeks of age with a mild deformity may be treated adequately by a limited suture resection, particularly those with sagittal synostosis. In most cases, however, suture resection alone will not yield a satisfactory result. The compensatory skull shape and associated fronto-orbital abnormalities produced by the fused suture have become the predominant deformities. Therefore, actively reshaping the deformities with a more extensive reconstruction frequently provides the best results. This includes supraorbital rim advancement in conjunction with bifrontal craniotomy in cases of metopic and coronal synostosis, for which the deformity involves the fronto-orbital region. No hair is shaved in any patient. The prepared area includes the orbital region in patients with coronal or metopic craniosynostosis where the deformity extends to the orbits. Care is taken to protect the cornea with shields or lubricants. In this way, the reconstruction can be evaluated by pulling the scalp back over the skull and orbits intraoperatively and examining the overall fronto-orbital soft-tissue profile. A coronal incision line is used for all patients (Fig. 5–1A). We extend the inferior portion obliquely posterior to the ear and then angle it anteriorly to the vertex of the skull (Fig. 5–1B). This incision allows simultaneous access to the anterior and posterior aspects of the skull, regardless of the skull deformity, and conceals the incisional alopecia. The incision should be beveled in the direction of the hair follicles to avoid amputating hair shafts and creating a wide scar. Dissection is done in the supraperiosteal plane to minimize blood loss, because stripping of the periosteum leads to significantly more bleeding from the bone. Leaving the periosteum attached to the underlying bone also assists in holding the bone together if it fractures during later remodeling. In metopic and coronal synostosis, exposure of the supraorbital region is needed for the supraorbital rim osteotomy. In these cases, an incision is made in the periosteum paralleling the rim. Dissection proceeds directly on the bone 1 cm above the supraorbital rim (Fig. 5–1C), thus allowing the supraorbital groove and its nerve to be visualized and separated. Subperiosteal dissection is carried to the level of the nasofrontal suture medially and the frontozygomatic suture laterally, exposing the entire supraorbital rim in preparation for the orbital rim osteotomy. Care is taken not to detach the medial canthus. The temporalis muscle is exposed in a suprafascial fashion and not detached from the underlying bone. FIGURE 5–1. Scalp incisions. A: Bicoronal skin incision. B: Stealth incision. C: Subperiosteal dissection in the supraorbital region beginning at 1 cm superior to the orbit. The orbital osteotomy is performed after a bifrontal craniotomy, which extends approximately 5 mm above the supraorbital rim (Fig. 5–2A). The dura is separated from the anterior frontal fossa to the level of the cribriform plate dural attachments and also dissected off the lateral greater sphenoid wing in the anterior temporal fossa in preparation for the osteotomies. A side microreciprocating saw or osteotome then is used to perform an orbital roof osteotomy approximately 5 to 10 mm posterior to the orbital rim. Malleable retractors are used to protect the brain and orbital contents. The osteotomy extends medially just anterior to the cribriform plate and laterally through the lateral wall of the orbit to the frontozygomatic suture. An osteotome is used to complete the fractures at the level of the frontozygomatic suture and the frontonasal suture. Both supraorbital rims are removed as a single unit for later contouring. FIGURE 5–2. Correction of early metopic synostosis. A: Bifrontal craniotomy and bilateral supraorbital rim osteotomy. The frontal bone then is remodeled to eliminate the frontal keel and triangular shape. B: Composite flap of temporal squamosal bone and temporalis muscle is developed using the Gigli saw and craniotome. C: Composite flap is created and reflected laterally. Barrel stave osteotomies are created in the more inferiorly located temporal bone and out-fractured. D: Remodeling of supraorbital rim. E: Parallel osteotomies in the parietal region for lateral expansion. F: The supraorbital rim is advanced and fixed to the glabella. The composite flap is then brought forward to the advanced orbital rims. G: Reshaped frontal bone is attached to the underlying dura and supraorbital rim. Postoperative temporal hollowing has been a cosmetic problem after detachment of the temporalis muscle and orbital advancement in the treatment of coronal and metopic craniosynostosis. Consequently, a composite temporalis advancement was devised. Instead of dissecting the temporalis muscle off the bone, a composite of the temporal squamous bone and muscle is elevated in an osteoplastic fashion. After a bifrontal craniotomy above the temporalis, two 2.0- to 2.5-cm vertical incisions are made into the temporalis muscle and squamous temporal bone: anteriorly at the greater wing of the sphenoid and posteriorly at the level the external auditory canal. The sphenoid wing usually needs to be partially resected with a rongeur. After the dura is freed of the inner table of the cut bone, a Gigli saw is slid down the two vertical grooves and used to undercut the base of the squamous temporal bone while preserving the overlying temporalis muscle (Fig. 5–2B). This composite myoosseus unit then is subsequently attached to the advanced orbital rim to prevent postoperative temporal hollowing. The techniques for reconstruction of the skull differ for different age groups. For patients younger than 1 year of age, the bone is thinner and more malleable. An abnormally convex surface may be made flat by performing radial osteotomies into the center of the bone. In an area that is abnormally flat and needs to be made more convex, radial wedge resections along the radial osteotomies are made. The bone then can be remodeled appropriately by gentle bending with a Tessier rib bender. Cranial defects are consistently regenerated during this time. The development of absorbable plates and screws now permits the use of rigid fixation in this age group. Permanent metallic rigid fixation is not preferred because endosteal displacement of hardware and the possibility of limiting brain growth are to be avoided. In patients older than 1 year of age, the bone of the skull is thicker, much more brittle, and more difficult to remodel. The best reconstructive strategy may be switching different osteotomy segments, substituting, for instance, in metopic synostosis, an appropriately contoured parietal skull for the triangle-shaped forehead. The more triangle-shaped forehead then may be weakened by creating channels or kerfs in the undersurface of the skull and with gentle “green stick” fracturing of the bone to a more flat configuration to serve as the posterior frontal skull. In some cases, an appropriate contour can be found by dividing an osteotomy segment and rotating the two pieces. If, however, there is no suitable substitute for the forehead bone, remodeling of the original frontal bone may be done by cutting it into smaller slats and remodeling these using kerfs or selectively placed weakening points (channels) on the endocranial surface of the bone. The thicker bone cannot be remodeled satisfactorily as one piece with radial cuts or wedge resections. Sizable cranial defects should be filled with bone grafts because they will persist. The surgical objectives in patients with metopic synostosis are to reduce the prominence of the midline forehead bone, to release the synostosis at the metopic suture, to reduce to normal the trigonocephaly over the forehead region, to advance the supraorbital rims laterally to a normal projection, and to advance the temporal myoosseous units forward to prevent temporal depression. In children younger than 1 year, the patient is placed supine, and the coronal incision is made to expose the frontal and orbital regions. A bifrontal craniotomy from just anterior to the coronal suture to 1 cm above the supraorbital rim is performed. The anterior fontanel is usually patent; therefore, craniotomy is based on the anterior fontanel as an entry point, followed by a bilateral supraorbital rim osteotomy with an oblique cut at the frontozygomatic suture (Fig. 5–2A). The supraorbital rim is remodeled to a more convex shape with restored lateral frontal projections, and the frontal bone is remodeled to eliminate the frontal keel and to achieve more lateral frontal prominence (Figs. 5–2A and D). In the temporal region, the composite resection is performed. The remaining basal squamosal temporal bone is split into vertical “barrel staves” and out fractured, thereby increasing the temporal flare (Fig. 5–2C). The remodeled supraorbital rim is advanced and fixed to the glabella, taking care to achieve the desired frontal nasal angle of approximately 20 to 30 degrees. The advancement is anchored by placing the lateral frontal bone of the supraorbital rim in front of the lateral zygomatic process (Fig. 5–2F). The composite temporal bone and muscle flap are brought forward and attached to the advanced orbital rims with absorbable plates. The advancement achieved is usually between 12 and 17 mm. At the coronal suture, adjacent bone is removed, and the parietal region is expanded by parallel osteotomies (Fig. 5–2E). The reshaped frontal bone is attached to the supraorbital rim (Fig. 5–2G). Occasionally, a prominent frontal keel exists without significant orbital retrusion or temporal narrowing. These cases can be treated simply by burring down the keel without an extensive reconstruction. In children older than 1 year, who have more mature bone, the frontal graft can be remodeled by splitting it into vertical slats with kerfs cut on the undersurface (Fig. 5–3). Alternatively, a second bone graft can be harvested with a biparietal craniotomy to substitute for the malformed frontal bone. The biparietal bone provides a smooth, round forehead without the need for extensive reshaping. With this biparietal bone segment, the proper amount of flare and flattening of the forehead usually is achieved. This segment should be cut to equal the height of the forehead which is usually 4.5 to 5.5 cm. Split calvarium may be needed to fill in bone gaps. No effort is made to correct the hypotelorism during early surgery. It is usually mild and partially self-correcting. If hypotelorism is pronounced in an older child, however, correction may be warranted. The supraorbital rim can be widened by splitting it at the midline and fixating an intervening free bone graft. By age 9 to 12 months, the lateral intercanthal distance should be 85 to 100 mm. Additionally a 3-cm inferior nasofrontal osteotomy with a wedged bone graft can be performed to increase the medial intercanthal distance. Of the various types of craniosynostosis, metopic synostosis has the most consistently favorable results after surgery. Reoperation is less common than after early supraorbital advancement and frontal reshaping. Treatment goals for patients with unilateral coronal synostosis are to remove the stenosis of the coronal suture, to provide symmetry to the forehead, to advance the supraorbital rim on the side of the fused suture, to normalize the shape of the orbits, to reduce the compensatory bulging on the contralateral frontal bone, and to advance the temporalis myoosseous unit ipsilateral to the fused suture to prevent hollowing of the temporal region following orbital rim advancement. The associated nasal deviation is not corrected because it usually improves with further development. In children younger than 1 year, the patient is placed in a supine position, and a bicoronal incision is made. A bifrontal craniotomy is performed, taking care not to detach the temporalis muscle (Fig. 5–4A). A bilateral orbital roof osteotomy with lateral cuts at the frontal zygomatic sutures follows. The orbital rims not only are recessed in unilateral coronal synostosis, but they are asymmetric. A drill is used to contour the orbits to symmetry and the orbital bar is outfractured with weakening kerfs to restore the normal projection (Figs. 5–4B and C). The ipsilateral pterion is resected to the frontosphenoid suture, and a composite temporalis flap is elevated ipsilateral to the fused suture. The reshaped symmetric supraorbital rim is advanced, secured at the midline and sutured laterally in front of the frontal process of the zygoma (Fig. 5–4D). The advancement should aim for overcorrection. A composite temporalis flap is created on the ipsilateral advancement side and is attached to the advanced supraorbital rim. The bifrontal bone graft is contoured to increase the projection on the flattened side and to reduce the projection of the bulging side. The remodeled frontal bone is attached to the advanced supraorbital rims.
SURGICAL INDICATIONS
PREOPERATIVE MANAGEMENT
PREOPERATIVE PLANNING
INTRAOPERATIVE TECHNIQUES
Initial Exposure
Orbit Osteotomy
Temporal Region
Bone Remodeling Techniques
TREATMENT FOR INDIVIDUAL FORMS OF CRANIOSYNOSTOSIS
Metopic Synostosis
Unilateral Coronal Synostosis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


