2 Craniovertebral Junction
I. Key Points
– The craniovertebral junction (CVJ) includes the base of the occiput (O), the occipital condyles, and vertebrae C1 and C2.
– Principal motion at O-C1 is flexion-extension and at C1-C2 axial rotation.
– The CVJ ligamentous complex is key to the stability of this region (Fig. 2.1).
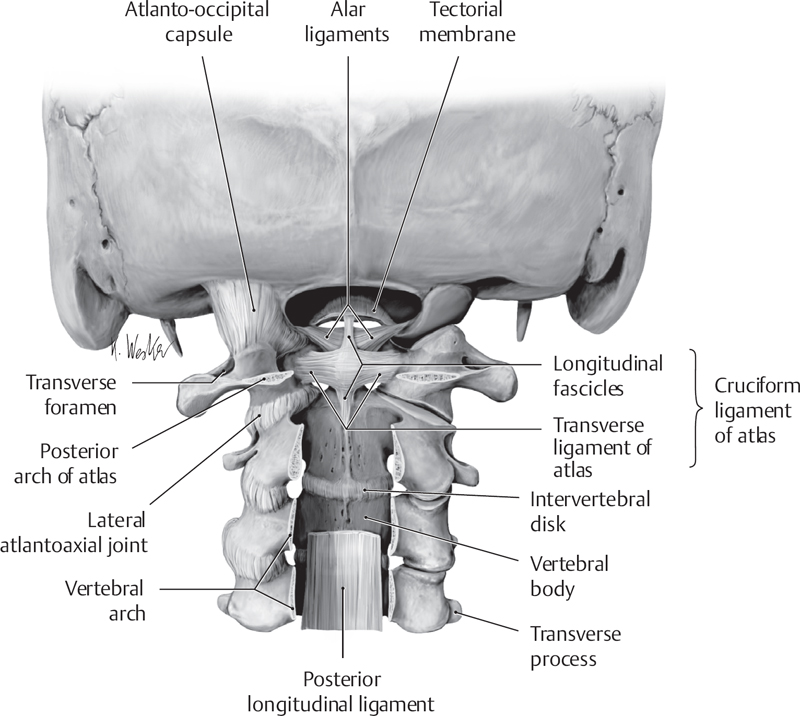
Fig. 2.1 CVJ ligamentous structures (from THIEME Atlas of Anatomy, General Anatomy and Musculoskeletal System, (c) Thieme 2005, Illustration by Karl Wesker).
II. Bony Anatomy
– CVJ refers to the base of the occiput, the atlas (C1), and the axis (C2).
– The boundaries of the foramen magnum are the basion anteriorly, the opisthion posteriorly, and the occipital condyles inferolaterally.
– C1 has no vertebral body or spinous process. It has a posterior arch and an anterior arch. It’s the widest cervical vertebra, and its superior concave articular surface accommodates convex occipital condyles (Fig. 2.2).
– The C1 anterior tubercle (C1 “button”) is the attachment site of the anterior longitudinal ligament (ALL) and the longus colli muscle.
– The vertebral artery and C1 nerve run along the superior lateral groove on C1 (sulcus arteriosus). In less than 15% of the population the groove is roofed, forming a foramen (arcuate foramen).
– C2 consists of the body, odontoid process, articulating surfaces, pedicles, pars interarticularis (note that pars and pedicles are distinct anatomical landmarks), lamina, and large, bifid spinous process (Fig. 2.3).1
– The C2 odontoid (Gr. “tooth”) process projects superiorly and has multiple (and overlapping) ligamentous attachments to C1 and the occiput.
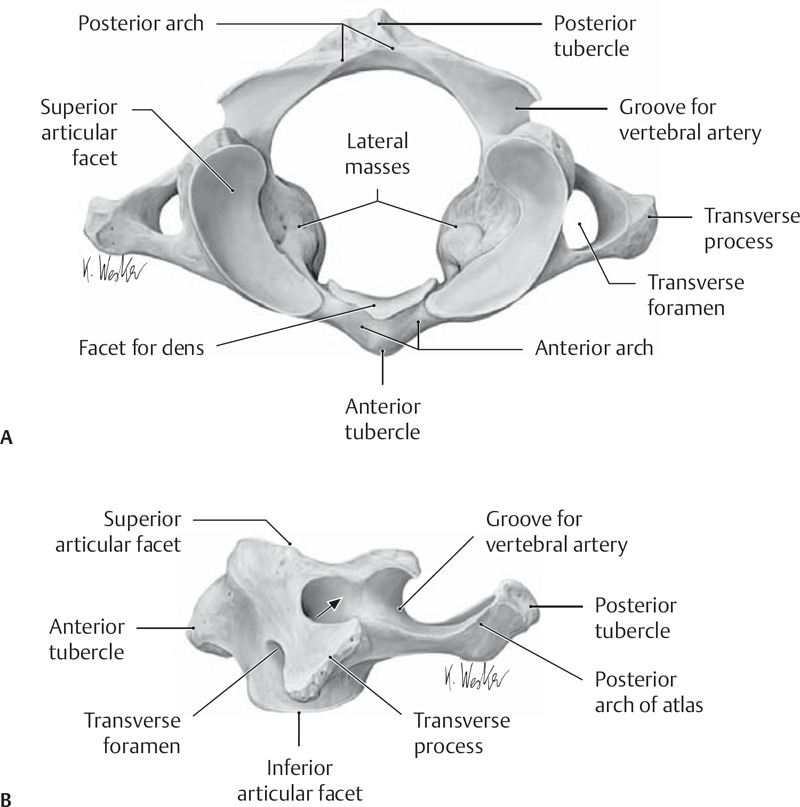
Fig. 2.2 (A) Superior and (B) lateral view of the atlas (from THIEME Atlas of Anatomy, General Anatomy and Musculoskeletal System, (c) Thieme 2005, Illustration by Karl Wesker).
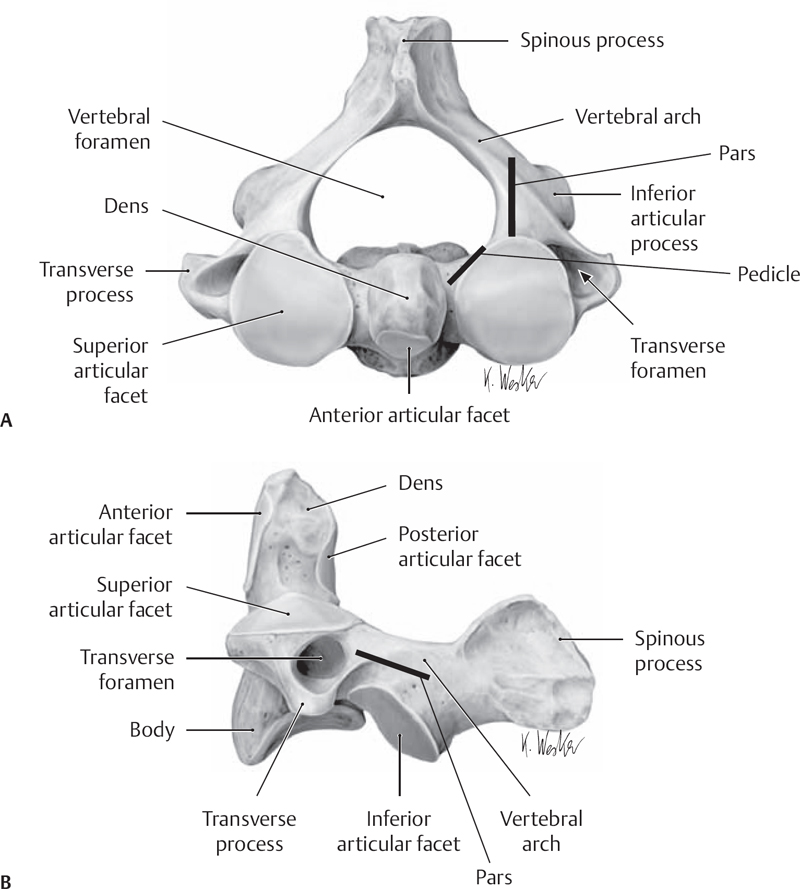
Fig. 2.3 Superior (A) and lateral (B) view of the axis (from THIEME Atlas of Anatomy, General Anatomy and Musculoskeletal System, (c) Thieme 2005, Illustration by Karl Wesker).
III. Neural Anatomy
– Cervical nerve roots exit above their corresponding level (i.e., C2 nerve root exits above C2 pedicle).
– C1 nerve root: the posterior division (suboccipital nerve) is more prominent than the anterior division. It innervates suboccipital muscles and occasionally branches to the lesser/greater occipital nerve.
– C2 nerve root: posterior, medial (greater occipital nerve), and lateral divisions innervate suboccipital muscles and scalp from occiput to vertex.
– The lesser occipital nerve is formed by dorsal divisions of C2 and C3.
IV. Vascular Anatomy
– The vertebral artery (VA) leaves the C2 transverse foramen (becoming V3), takes a 45 degree lateral projection, and ascends (vertical portion of V3) into the C1 transverse foramen.
– The VA then courses medially (horizontal portion of V3) along the C1 sulcus arteriosus and then anteriorly through the atlantooccipital membrane, where it becomes intradural (beginning of V4 segment).
– Blood is supplied to the CVJ primarily through branches of the vertebral and occipital arteries.
– The base of the dens of C2 receives blood supply from vertebral artery branches (posterior circulation); the top is supplied by apical branch of the hypoglossal artery (anterior circulation).
– Lymphatic drainage of the CVJ is through retropharyngeal and deep cervical nodes (Grisel’s syndrome: CVJ instability with concomitant retropharyngeal inflammation/infection).
V. Ligamentous and Muscular Anatomy (Table 2.1)
– Suboccipital muscles and the CVJ (Fig. 2.4)
• Superior oblique: C1 transverse process laterally to occiput medially
• Inferior oblique: C1 transverse process laterally to spinous process of C2 medially
• Rectus capitis posterior major: spinous process of C2 up to base of occiput
• Rectus capitis posterior minor: posterior tubercle of C1 up to base of occiput
• Semispinalis capitis: transverse processes of cervical vertebrae to nuchal ligament and occipital bone; superficial to suboccipital muscles
• Longissimus capitis: similar to semispinalis but runs and attaches more laterally to the occiput
Table 2.1 Principal CVJ Ligaments: Their Attachments and Modes of Action
| Ligament | Attachments | Action |
| Apical | Odontoid tip (superiorly) to basion | Limits O-C2 distraction |
| Alar | Odontoid tip (laterally) to medial tubercle of occipital condyles and lateral masses of C1 | Limits O-C2 subluxation/hyperrotation |
| Cruciate | Vertical component: body of C2 to basion Transverse component: medial tubercles of C1 lateral masses to posterior dens | Prevents C1/C2 subluxation and O-C1/C2 distraction |
| Tectorial | Posterior aspect of vertebral bodies, dorsal to cruciate ligament (continuation of PLL) | Limits hyperflexion, distraction |
| ALL | Anterior aspect of vertebral bodies | Limits hyperextension, distraction |
| Accessory atlantoaxial | C2 body laterally to medial C1 lateral masses | Limits atlantoaxial hyperrotation |
| Capsular | O-C1 and C1-C2 articulating facets | Stabilizes facet joints |
| Anterior and posterior atlantooccipital membranes | Anterior: basion to C1 tubercle (C1 button) Posterior: opisthion to C1 posterior arch | Limit atlantooccipital distraction |
Abbreviations: ALL, anterior longitudinal ligament; O, occiput; PLL, posterior longitudinal ligament.
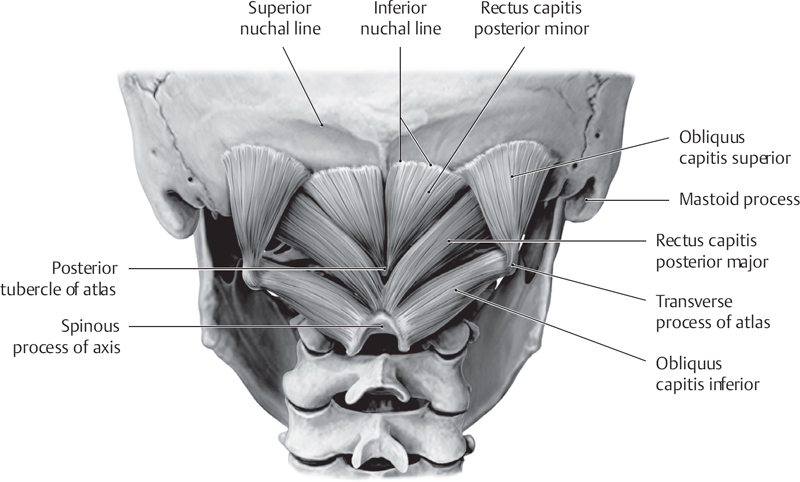
Fig. 2.4 Muscles of the suboccipital triangle (from Atlas of Anatomy, (c) Thieme 2008, Illustration by Karl Wesker).
VI. Surgical Pearls
– C1 nerve root, if present, can be sacrificed; though we don’t routinely perform this, C2 nerve root may also be sacrificed (with minimal risk of occipital neuralgia).2
– Integrity of cruciate ligament must be considered before any CVJ stabilization procedure is undertaken.
– Venous plexus around C2 ganglion may cause considerable bleeding, which should not be mistaken for VA injury.
– Thin-cut CT of the CVJ and/or CT angiography (CTA) should be obtained prior to C1/C2 fixation to verify route and patency of the vertebral arteries, as well as dimensions of the pars interarticularis and/or pedicle.
Common Clinical Questions
1. What is the source of the blood supply to the odontoid process of the axis?
2. What forms the continuation of the posterior longitudinal ligament (PLL) at the CVJ?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







