But how great was his apprehension, when he farther understood, that [the force of parturition] acting upon the very vertex of the head, not only injured the brain itself, or cerebrum—but that it necessarily squeezed and propelled the cerebrum towards the cerebellum, which was the immediate seat of the understanding!—Angels and ministers of grace defend us! Cried my father—can any soul withstand this shock?—No wonder the intellectual web is so rent and tattered as we see it; and that so many of our best heads are no better than a puzzled skein of silk,—all perplexity—all confusion within-side.
I. FUNCTIONS OF THE CEREBELLUM
A. What the cerebellum does not do
1. Laurence Sterne correctly satirized the speculative neurophysiology of his time, which localized “the immediate seat of the understanding” to the cerebellum. Nevertheless, the cerebellum apparently participates in the regulation of cognition, emotion, and autonomic functions more than generally appreciated (Buckner, 2013). Cerebellar lesions can result in the cerebellar cognitive affective syndrome (CCAS) comprising a constellation of executive behavioral dysfunction, visual-spatial deficits, linguistic impairments, and behavioral-affective disturbances and a posterior fossa syndrome, presenting with similar symptoms but more often described in children after cerebellar tumor surgery. There is no general consensus with regard to assigning parts of the cerebellum to specific cognitive dysfunction, but it has been proposed that the anterior lobe and parts of medial lobule VI and lobule VIII of the posterior lobe contain the representation of the sensorimotor cerebellum; parts of lobule VI and lobule VII of the posterior lobe comprise the cognitive cerebellum; and the posterior vermis and the fastigial nucleus are the anatomical substrate for the limbic cerebellum (Buckner, 2013; De Smet et al, 2013).
2. The cerebellum has no clinically evident role in consciousness per se.
3. The cerebellum has no clinically evident role in the conscious appreciation of sensation, despite massive sensory connections. Holmes (Holmes, 1939; van Gijn, 2007) repeatedly stated that standard clinical tests did not reveal sensory deficits in cerebellar patients (Pts).
B. What the cerebellum does do
1. The most explicit function of the cerebellum for clinical testing is its role in coordinating willed muscular contractions. To coordinate means to adjust the rate, range, force, and sequence of willed muscular contractions. In so acting, the cerebellum belongs to a distributed sensorimotor network for coordination that includes the cerebral cortex, basal motor nuclei, thalamus, and reticular formation (De Smet et al, 2013).
2. As Hughling’s Jackson (1834–1911) stated, “It will not suffice to speak of coordination as a separate ‘faculty.’ Coordination is the function of the whole and every part of the nervous system.” Not the least are the sensory systems. Visual, tactile, and auditory systems send afferents to the cerebellum, but coordination pre-eminently requires proprioceptive input from joints, muscles, and vestibular system.
3. To make a movement, the brain must know where the body part starts from to orchestrate the sequence, rate, and force of muscular contractions required to get the part from point A to point B. Musculoskeletal proprioceptors and other senses inform the cerebellum about extremity position and movement, joint angles, and the length of and tension on muscles and joints, that is, the state of the muscles and skeletomuscular levers at any given instant to generate an internal model that assists with error detection and correction (Ebner et al, 2011; Manto et al, 2012). From this information, the cerebellum coordinates muscular contractions, through its feedback to the cerebral cortex as well as directly through the reticular formation and via their reticulospinal tracts, to produce steady volitional movements and steady volitional postures (Mottolese et al, 2013; Thach, 2014). Thus, the crucial clinical tests for cerebellar dysfunction expose unsteadiness of volitional movements and unsteadiness of volitionally sustained postures.
4. Now, if you understand the role of the cerebellum, you can answer this question: Could you test a paralyzed or comatose Pt for cerebellar dysfunction?  Yes/
Yes/ No. Explain. (
No. Explain. ( No)
No)
_________
_________
A comatose or paralyzed Pt makes no willed movements and maintains no willed postures.
5. Patients with cerebellar lesions make lower scores on neuropsychological tests and tend to have personality changes, with apathy or disinhibited, socially inappropriate behavior (De Smet et al, 2013). As yet no specific pattern of cognitive or affective dysfunction clearly localizes a lesion to the cerebellum, as do the standard motor tests. At one time control of movement was believed to be the main function of the cerebellum (“The cerebellar doctrine”) and Purkinje cells the only neuron involved in and the site of motor learning (Galliano and De Zeeuw, 2014). The rich bidirectional communication between widespread cortical areas and limbic system with the cerebellum and further insights into the cytoarchitecture and physiological characteristics of the microcircuits of the cerebellum provides further support for its major role in motor activity and some “explanations” for the observed role it plays in language, cognition, and behavior (Cerminara and Apps, 2011; Chadderton et al, 2014; Llinás 2014; Cerminara et al, 2015).
BIBLIOGRAPHY · Cerebellum
Buckner RL. The cerebellum and cognitive function: 25 years of insight from anatomy and neuroimaging. Neuron. 2013;80:807–815.
De Smet HJ, Paquier P, Verhoeven J, Marien P. The cerebellum: its role in language and related cognitive and affective functions. Brain Lang. 2013;127:334–342.
Cerminara NL, Apps R. Behavioral significance of cerebellar modules. Cerebellum. 2011;10:484–494.
Cerminara NL, Lang EJ, Sillitoe RV, Apps R. Redefining the cerebellar cortex as an assembly of non-uniform Purkinje cell microcircuits. Nature Rev Neurosci. 2015;16:79–93.
Chadderton P, Schaefer AT, Williams SR, Margrie TW. Sensory-evoked synaptic integration in cerebellar and cerebral cortical neurons. Nature Rev Neurosci. 2014;15:71–83.
Ebner TJ, Hewitt AI, Popa LS. What features of limb movements are encoded in the discharge of cerebellar neurons? Cerebellum. 2011;10:683–693.
Galliano E, De Zeeuw CI. Questioning the cerebellar doctrine. Prog Brain Res. 2014;210:59–77.
Llinás RR. The olivo-cerebellar system: A key to understanding the functional significance of intrinsic oscillatory brain properties. Front Neural Circuits. 2014;7:96.
Manto M, Bower JM, Comfort AB, et al. Consensus Paper: roles of the cerebellum in motor control—the diversity of ideas on cerebellar involvement in movement. Cerebellum. 2012;11:457–487.
Mottolese C, Richard N, Harquel S, et al. Mapping motor representations in the human cerebellum. Brain. 2013;136:330–342.
Thach WT. Does the cerebellum initiate movement? Cerebellum. 2014;13:139–150.
Van Gijn J. From the Archives. Symptomatology of cerebellar tumours; a study of forty cases. by T. Grainger Stewart (Registrar) and Gordon Holmes (Resident Medical Officer, National Hospital, Queen Square, London). Brain 1904;27:522–591. With The symptoms of acute cerebellar injuries due to gunshot injuries. By Gordon Holmes. Brain 1917;40:461–535. With the cerebellum of man. By Gordon Holmes. Brain 1939;62:1–30. Brain 2007;130:4–7.
II. ANATOMY OF THE CEREBELLUM
A. The three cerebellar lobes
1. Larsell divided the cerebellum transversely into three lobes and longitudinally into three parts, one midline vermis uniting two hemispheres (Fig. 8-1).
FIGURE 8-1. Schematic dorsal view of the cerebellum (Larsell nomenclature). In reality, the flocculonodular lobe is rolled under, out of sight, when the cerebellum is viewed dorsally (Fig. 8-2).
2. In contrast to the schematic depiction of lobes shown in Fig. 8-1, Fig. 8-2 shows the flocculonodular lobe rolled under in its true position. Label the lobes.
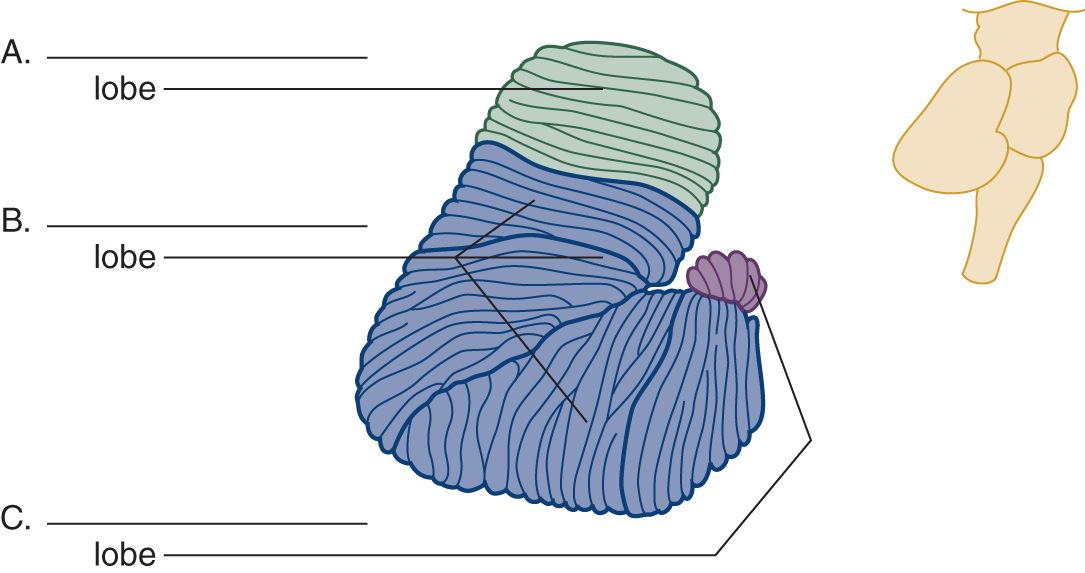
FIGURE 8-2. Right lateral view of the cerebellum. The inset at the right shows the relation of the cerebellum to the brainstem. Label the lobes A to C.
B. Cerebellar phylogenesis
1. Phylogeny provides the best understanding of the clinical syndromes of the cerebellum. The cerebellum evolved out of the vestibular nuclei. Its vestibular origin condemns it to straddle forever the vestibular nerves and nuclei, at the pontomedullary junction, and to retain forever its connections with the vestibular system—the law of retained original innervation.
2. Vestibular proprioceptors provide information about the movement of the head and its position in relation to the pull of gravity. Having no limbs, primitive animals require only a small nubbin of cerebellum to coordinate the axial muscles that position the eyes, head, and trunk. This nubbin is the flocculonodular lobe (as its major input is derived from the vestibular system it may be appropriate to use another frequently encountered name, vestibulocerebellum, or the one that has a teleological inspiration, archicerebellum).
3. All higher animals retain the vestibulocerebellar connections and their axial functions, but the budding limbs impress new roles on the cerebellum; it must now coordinate axial (trunk) and appendicular (limb) muscles. The emergence of the vertical bipedal from the quadrupedal posture places particular demands on gait coordination. The second portion of the cerebellum evolves to receive most of the proprioceptive input from the limbs and trunk, the anterior lobe (the term spinocerebellum is often used, but a misnomer as it implies that these are the only sources of input and again the term paleocerebellum is encountered implying an evolutionary origin).
4. The third cerebellar lobe expands in equal measure with the cerebrum, motor cortex, pyramidal tract, pontine basis, and inferior olivary nuclei. The corticopontocerebellar and olivocerebellar pathways send the major inputs to this newest part, the posterior lobe (the term pontocerebellum is occasionally used to indicate its input from the pons, but not entirely and hence confusing, and finally as a sign of its relative evolutionary “newness,” neocerebellum). The inferior olivary nuclei project topographically to all three cerebellar lobes.
5. To recapitulate: The cerebellum consists of three lobes: the anterior, posterior, and flocculonodular, based on phylogenesis and the major source of afferent connections (Baizer, 2014; Butts et al, 2014; Smaers, 2014). Complete Table 8-1.
TABLE 8-1 • Some Major Afferent Pathways to the Lobes of the Cerebellum
Cerebellar lobe | Major afferent pathway |
Anterior lobe (spinocerebellum) | _________ |
Posterior lobe (cerebrocerebellum) | _________ |
Flocculonodular lobe (vestibulocerebellum) | _________ |
All lobes | _________ |
6. Lesions of each of the lobes cause different clinical syndromes. From the clinical findings, the examiner (Ex) can predict the location and often the type of lesion (Table 8-3).
C. The three pairs of cerebellar peduncles and their pathways
1. Three pairs of peduncles anchor the cerebellum to the pons: the superior (rostral), middle, and inferior (caudal). These thick stalks convey only and all afferent and efferent cerebellar connections (Roostaei et al, 2014). Transection of the peduncles allows the cerebellum to fall free from the brainstem (Fig. 8-3).
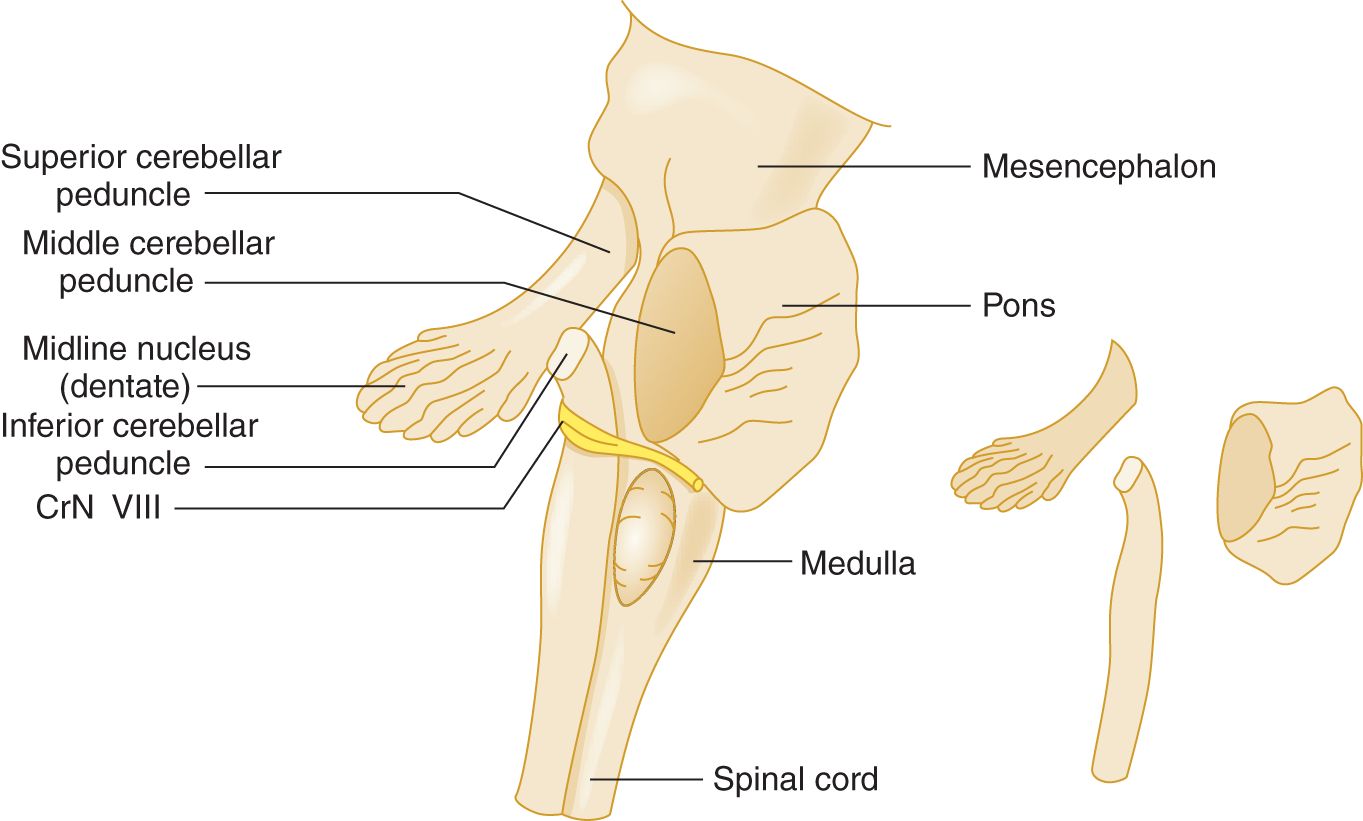
FIGURE 8-3. Right lateral view of the brainstem to show the cerebellar peduncles. The inset at the right is an exploded view of the peduncles.
2. The three pairs of peduncles anchor the cerebellum to only one part of the brainstem, the  mesencephalon/
mesencephalon/ pons/
pons/ medulla. Therefore, all cerebellar afferents and efferents must pass through the pons and through one of the peduncles. (
medulla. Therefore, all cerebellar afferents and efferents must pass through the pons and through one of the peduncles. ( pons)
pons)
3. The middle peduncle, the simplest peduncle in composition, conveys almost exclusively pontocerebellar fibers.
4. The connections of the inferior cerebellar peduncle are predicted by its neighbors: the spinocerebellar tracts, medulla, and vestibular nerve. Thus, the inferior peduncle transmits dorsal spinocerebellar, trigeminocerebellar, and olivocerebellar afferents and interchanges afferent and efferent connections with the medullary reticular formation and the vestibular nuclei.
5. The superior cerebellar peduncle (or brachium conjunctivum) angles forward and ventrally through the pons and into the midbrain (Fig. 8-3). It contains the major efferent cerebellar pathway that aims toward the contralateral red nucleus and thalamus. For the priggish neuroanatomist, we note that the dorsal spinocerebellar tract veers directly into the cerebellum via the inferior peduncle and that the ventral spinocerebellar tract ventures rostrally before entering via the superior peduncle—but the latter fact has no particular clinical value. More importantly, both spinocerebellar tracts end in the anterior lobe, especially in the vermis, making the anterior lobe the “spinocerebellum.” These tracts convey proprioceptive information to the anterior lobe from the muscles and joints of the neck, trunk, and extremities. Subpopulations of neurons that give rise to these tracts are also influenced by spinal cord interneurons of the spinal central pattern generators and descending tracts. Such a system allows proprioceptive and other information that is “expected” by a movement as well as unexpected to be provided to the cerebellum (Stecina et al, 2013).
D. Recapitulation of the cerebellar peduncles
1. In activating muscles for voluntary contractions, the cerebrum communicates with the cerebellum via the corticopontocerebellar pathway, which ends mainly in the _________
2. The corticopontocerebellar pathway runs in the _________
3. The major efferent peduncle is the _________
4. Afferents of the olivary, vestibular, and dorsal spinocerebellar systems and cerebellar efferents run through the _________
5. Recall that the cerebellar lobe that arose out of the vestibular system and retains strong vestibular connections throughout its phylogenetic history is the _________
6. Of the three cranial nerves (CrNs) attached along the pontomedullary sulcus, the most dorsal one, closest to the inferior peduncle, is CrN ________ and the most ventral one, farthest from the peduncle, is CrN _________
E. Circuits of the cerebellum
1. Major sources of afferents to the cerebellum arise from the following:
a. Spinocerebellar system, via inferior and superior peduncles, to the anterior lobe (“paleocerebellum,” “spinocerebellum”).
b. Corticopontocerebellar system, via middle peduncle, mainly to the posterior lobe (“neocerebellum,” “cerebrocerebellum”).
c. Vestibulocerebellar system, via inferior peduncle, mainly to the flocculonodular lobe (“archicerebellum,” “vestibulocerebellum”).
d. Olivocerebellar system, via inferior peduncle, to all cerebellar lobes.
e. The afferent fibers send collaterals to the deep cerebellar nuclei on their way to the cerebellar cortex.
2. Intrinsic cerebellar circuits: All afferent fibers ascend through the cerebellar white matter to influence ultimately the large Purkinje neurons found ubiquitously throughout the cerebellar cortex (Cerminara et al, 2015). The Purkinje axons afford the only way out of the cerebellar cortex. They descend through the cerebellar white matter, and the vast majority synapse on the deep nuclei of the cerebellum, and a small minority synapse directly on the vestibular nuclei. The deep cerebellar nuclei, the largest of which is the dentate nucleus, sit in the roof of the IV ventricle. Learn Fig. 8-4.
FIGURE 8-4. Diagram showing the flow of impulses through the cerebellum.
3. Extrinsic cerebellar circuits: The cortico-ponto-cerebello-thalamo-pyramidal circuit.
a. Well, yes, instead of inventing such a word, we could just introduce a law: Cerebral hemisphere lesions cause contralateral motor signs, whereas cerebellar hemisphere lesions cause ipsilateral signs, if that is all you want to know. It is more elegant, if more demanding, to learn the actual circuit that underlies the correlation between lesion site and clinical signs (Fig. 8-5). Learning it will cause no harm and has practical value which you can verify at your next opportunity.
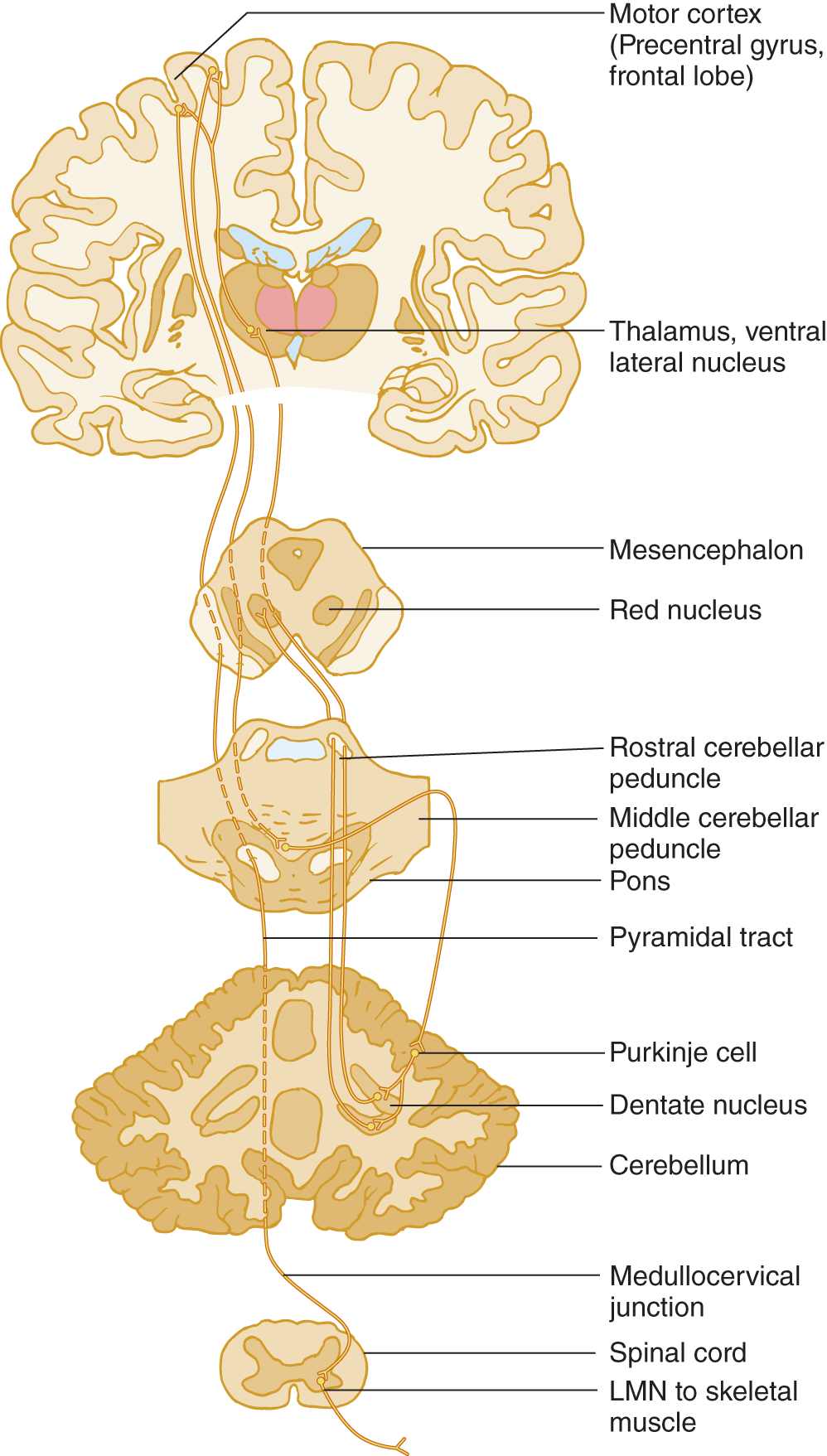
FIGURE 8-5. Diagram of the cerebro-cerebello-cerebral circuit. By this pathway, the cerebellum coordinates volitional movements by feeding back information to the cerebral motor cortex to influence its commands to the lower motoneurons via the pyramidal tract. Start at the motor cortex and trace through the circuit. Notice that the cerebro-cerebello-cerebral circuit double crosses the midline and that the pyramidal crossing brings the influence of one cerebellar hemisphere back to the same side.
b. Master Fig. 8-5 this way:
i. Learn the labeled structures.
ii. Start at the motor cortex in the precentral gyrus of the frontal lobe and trace a motor impulse from the motor cortex down to the cerebellar cortex, back to the motor cortex, and down the pyramidal tract.
iii. Using a colored pencil, draw the circuit on the opposite half of Fig. 8-5. Be sure to include the synapses, marked by Y.
c. By means of the single pyramidal decussation, cerebral hemisphere controls volitional movements on the  ipsilateral/
ipsilateral/ contralateral side of the body. (
contralateral side of the body. ( contralateral)
contralateral)
d. By means of double crossing pathways in conjunction with the pyramidal decussation, one cerebellar hemisphere ultimately coordinates muscular contractions on the  contralateral/
contralateral/ ipsilateral side of the body. (
ipsilateral side of the body. ( ipsilateral)
ipsilateral)
e. Hence, a lesion of one cerebellar hemisphere causes incoordinated muscular contractions on the  ipsilateral/
ipsilateral/ contralateral side. (
contralateral side. ( ipsilateral. Review the law in point 3-a.)
ipsilateral. Review the law in point 3-a.)
III. CLINICAL SIGNS OF CEREBELLAR DYSFUNCTION
A. The keys to detecting cerebellar dysfunction
Four cardinal cerebellar signs consist of ataxia (=dystaxia), tremor (intention tremor and postural), and, especially in acute lesions, hypotonia and asthenia. Taxis means “ordered,” as in taxonomy. Ataxia means “not ordered” or, as applied to the effect of cerebellar lesions, “uncoordinated” contractions of muscles during volitional movements or during volitionally sustained postures. Cerebellar signs derive not from weakness or loss of sensation but from loss of the movement coordination provided by the cerebellum.
Depressants such as alcohol preferentially affect vestibulocerebellar neurons. If you have ever been or seen an inebriated person, you will understand the syndrome immediately. A drunken person cannot coordinate any volitional muscular contractions. Thus, the person sways when standing (when maintaining a volitional posture), reels and missteps when walking, slurs words when talking, and his eyes oscillate when attempting to look at a target. The limbs hang loose and floppy. When a finger approaches a target, such as the nose, it may start to show a tremor as the movement progresses but will then definitely increase as the finger nears the target. If we apply technical terms to these signs, as is the habit of physicians, we can define the cerebellar syndrome as follows:
1. The overall incoordination of intentional movements is ataxia or dystaxia (Klockgether 2008; Pandolfo and Manto, 2013). Sensory ataxia also occurs with peripheral nerve or dorsal column lesions, as in the locomotor ataxia of tabes dorsalis due to syphilis, where proprioceptive input is impaired (Koike et al, 2010; Tong et al, 2013).
2. The tremor of intentionally maintained head or trunk posture or of a limb suspended in front of the body is called postural, positional, or static type of action tremor. (The “action” when holding a volitional posture is the active contraction of the muscles; see Fig. 7-38.) The unsteady oscillations of the head and trunk are also called titubation, occur a few times per second, and while it may be seen in cerebellar dysfunction is not pathognomonic or localizing.
3. The tremor as a limb approaches a target is called intention, end-point, or kinetic tremor. Classic cerebellar tremor occurs uni- or bilaterally depending on the underlying cerebellar disorder and usually has a frequency below 5 Hz.
4. The uncoordinated, slurred speech is called dysarthria, like any neurogenic disturbance of voice articulation.
5. The uncoordinated oscillations of the eyes are called nystagmus.
6. The loose floppy joints and muscles are called hypotonia, more frequently identified in affected children.
7. The person becomes silly, illogical, disinhibited, and socially inappropriate.
8. List the major clinical signs of cerebellar lesions (Hint: Start with the head and eyes and work caudally, visualizing a drunken person).
_________
_________
9. Another common neurogenic tremor, not caused by cerebellar lesions, is the tremor of Parkinson disease. This tremor appears when the part  rests/
rests/ undergoes volitional movement and disappears when the part
undergoes volitional movement and disappears when the part  rests/
rests/ undergoes volitional movement. (
undergoes volitional movement. ( rests;
rests;  undergoes volitional movement)
undergoes volitional movement)
B. The effect of cerebellar lesions on speech
Dysarthria in cerebellar Pts consists of slowness, slurring of words, and scanning speech. In scanning speech, the Pt’s voice varies from a low volume to a high volume as if scanning from peak to peak. The Pt fails to meter and modulate the strength of the muscular contractions that produce the speech sounds, thus accentuating the wrong syllables or words, or the Pt may speak too loudly and garrulously (Ogawa et al, 2010; Urban, 2013). A tremulousness, analogous to postural tremor, also may occur. Cerebellar lesions seem to affect speech less in children, but they may undergo a peculiar period of mutism after surgery for cerebellar neoplasms (Pitsika and Tsitouras, 2013).
C. The effects of cerebellar lesions on eye movement
Cerebellar lesions result in nystagmus, dysmetria of saccades, jerky rather than smooth pursuit, slowness in initiating eye movements, and skew deviation (Kheradmand and Zee, 2011; Eggenberger, 2014; Thurtell, 2014). Cerebellar nystagmus occurs pre-eminently during volitional use of the eyes and thus is gaze evoked; see the nystagmus dendrogram in Fig. 5-7.
To test for saccadic dysmetria, have the Pt look straight ahead and place your index fingers in the temporal fields. Ask the Pt to look first at one finger and then the other and then direct the Pt to look rapidly from one to the other several times and it will be noted that the eyes over or undershoot the target.
D. Clinical tests for dystaxia of station (stance) and gait
1. Symptomatic cerebellar lesions universally impair the gait and stance (the standing posture). Inspect the Pt for swaying when standing, which involves volitional posture, and for ataxia of gait, which involves volitional foot placement. The unsteady stance and reeling gait of the drunken person need no wordy description (lateropulsion is the tendency to move from side to side). To compensate for unsteadiness of stance and gait, the cerebellar Pt assumes a broad-based stance and a broad-based gait, just as a toddler does before gaining coordination, or an elderly Pt does after losing some. The signs witnessed not only consist of the motor and ocular disorders that accompany cerebellar dysfunction but also the safety strategies used by the Pt as well as their inaccurate adjustments undertaken to deal with their loss of balance (Ilg and Timmann, 2013).
2. To challenge the Pt’s coordination and overcome the compensatory broad-base, the Ex asks the Pt to stand with the feet together. Similarly, to expose gait incoordination, use a test known to every policeman: Ask the Pt to step along a straight line, placing the heel of one foot directly in front of the toe of the other, the so-called tandem walking, a sensitive test for gait ataxia. Now stand up and try tandem walking yourself. You will find that balancing on a narrow base when walking takes some ability.
3. To judge broad-based gaits, you must know where the heels fall in relation to the midline when a normal person walks. First, just for fun, guess where the medial margins of the heels fall in relation to the midline sagittal plane:  just on the midline/
just on the midline/ 2.5 cm off/
2.5 cm off/ 3 to 5 cm off/
3 to 5 cm off/ >5 cm off. (
>5 cm off. ( just on the midline)
just on the midline)
4. Unless the person has huge thighs, the medial margin of the heels falls exactly on the line. Verify this the next time you watch someone walk or, just as instructive, note the neat, precise tightrope placement of a dog’s hind feet.
5. Next stretch a string in a straight line or find a straight line on your floor and walk along it with your midline directly above it. Now walk straddling the string by deliberately placing each foot 2 to 3 in. to the side of the midline. Notice that even slight displacement of your heels from the midline will introduce a waddle in your gait. To the original signs of cerebellar dysfunction, we can add a swaying, broad-based stance and gait.
E. Clinical tests for arm dystaxia
1. Postural tremor and tremor of the arms during the finger-to-nose test
a. Ask the Pt to extend the arms straight out in front. Inspect the arms for wavering, indicating incoordination during this volitionally maintained posture, and for frank, rhythmic postural tremor. Having the Pt hold the fingers a little apart in front of the nose, with the arms elevated horizontally, in “the batswing” position, also demonstrates postural instability of the arms or postural tremor (Alusi et al, 2000).
b. After you have inspected the Pt with the arms held straight out, instruct the Pt to place his index finger on the tip of his nose.
i. To enlist the Pt’s best effort, say, “Move your finger in and place the tip of your finger exactly on the tip of your nose. Do not miss!”
ii. Inspect for dystaxia of the movement in progress or frank tremor that increases as the finger approaches the nose (intention type of kinetic tremor), and whether the Pt fails to precisely place the tip of the finger to the tip of the nose (dysmetria).
iii. Have the Pt perform this test (and later the heel-to-shin test) three times. If uncertain of the result, have the Pt alternately touch his nose, your finger, and his nose several times.
c. A tremor of the outstretched hands is called a _________
d. A tremor that increases as the finger approaches the nose or is reaching a target is called a _________
2. Cerebellar signs on one side implicate a lesion of the  ipsilateral/
ipsilateral/ contralateral cerebellar hemisphere because of
contralateral cerebellar hemisphere because of  one/
one/ two/
two/ three decussations. (
three decussations. ( ipsilateral;
ipsilateral;  three (Fig. 8-5))
three (Fig. 8-5))
3. Dysmetria: The dystaxic Pt, in seeking a specific endpoint, such as the nose on the finger-to-nose test, frequently undershoots or overshoots the target because of failure to control, or meter, the muscular contractions that set the distance.
4. The rapid alternating-movements tests for dystaxia and dysmetria (dysdiadokokinesia = dysdiadochokinesia)
a. The technical term for dystaxia-dysmetria of rapid alternating, movements, dysdiadochokinesia, is a lovely dactylic trimeter. This is the fórest priméval: dys di á dó ko ki né si a. This term describes nothing qualitatively different. It means only incoordination of muscular contractions during rapid alternating movements.
b. The Pt holds out the hands and pronates and supinates them as rapidly as possible. Test the hands separately and together. The dystaxic hand overshoots one time, undershoots the next, and is slower than normal (Fig. 8-6).
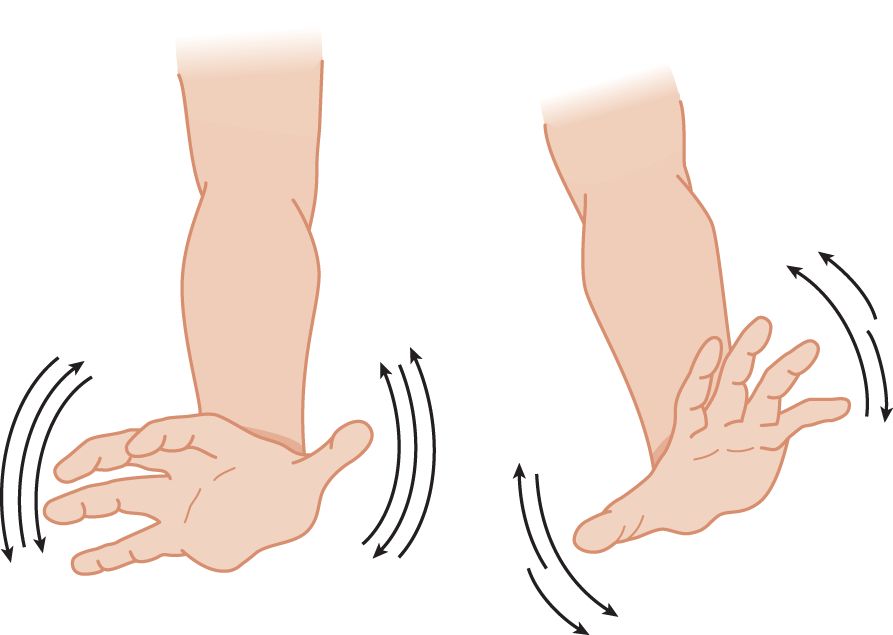
FIGURE 8-6. Pronation and supination test for dystaxia and dysmetria of the hands. Notice the even excursions of the normal right hand and the uneven excursions of the ataxic left hand.
c. A better method is the thigh-patting test. Test each hand separately and together. First demonstrate the action to the Pt by lightly slapping your own thigh, alternating first by slapping the palm and then the back of the hand, as rapidly and rhythmically as possible. Be sure to make an audible sound with each pat. Instruct the Pt to make actions that sound exactly like yours. The Ex sees and hears the slow rate and dysrhythmia of the ataxic hand (Fig. 8-7). You can detect the irregular rhythm of the alternating movements much better by sound than by sight.
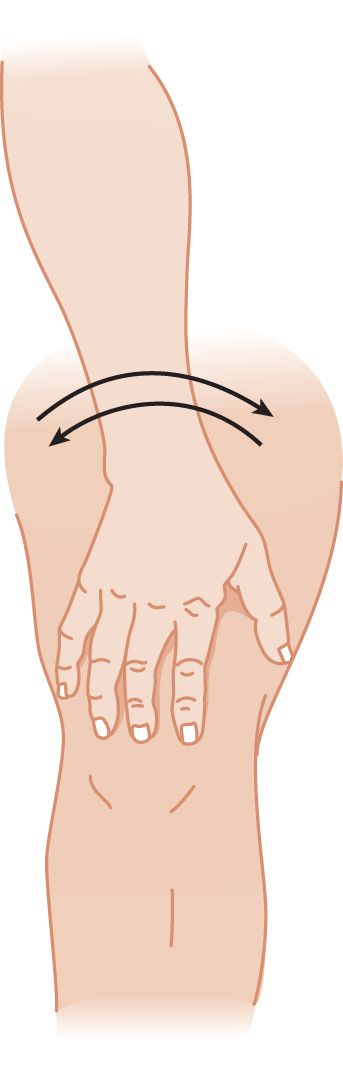
FIGURE 8-7. Thigh-patting test for dystaxia and dysmetria. The cerebellar patient slaps irregularly and turns the hand too much or too little in alternately slapping the front and the back of his hand on his thigh.
d. Here is a challenge to your mastery of this test: If you listen carefully, you will hear a slight but definite difference in the pitch of the sound from slapping the right or left thigh. We do not know the explanation, but the difference is real.
5. The finger-tapping test: Listen for dysrhythmia and slowness (Strauss, 2006). See Fig. 7-42.
F. Overshooting and checking tests of the arms
1. The cerebellar Pt has difficulty in maintaining a posture or position against a sudden, unexpected displacement. Have the Pt stand with eyes closed and arms outstretched.
2. Tell the Pt, “I am going to tap your arms. Hold them still. Do not let me budge them.” The Ex delivers to the back of the Pt’s wrist a quick push, strong enough to displace the arm. The normal subject’s arm returns quickly to its initial position. The cerebellar Pt’s arm oscillates back and forth: It overshoots several times (Fig. 8-8).
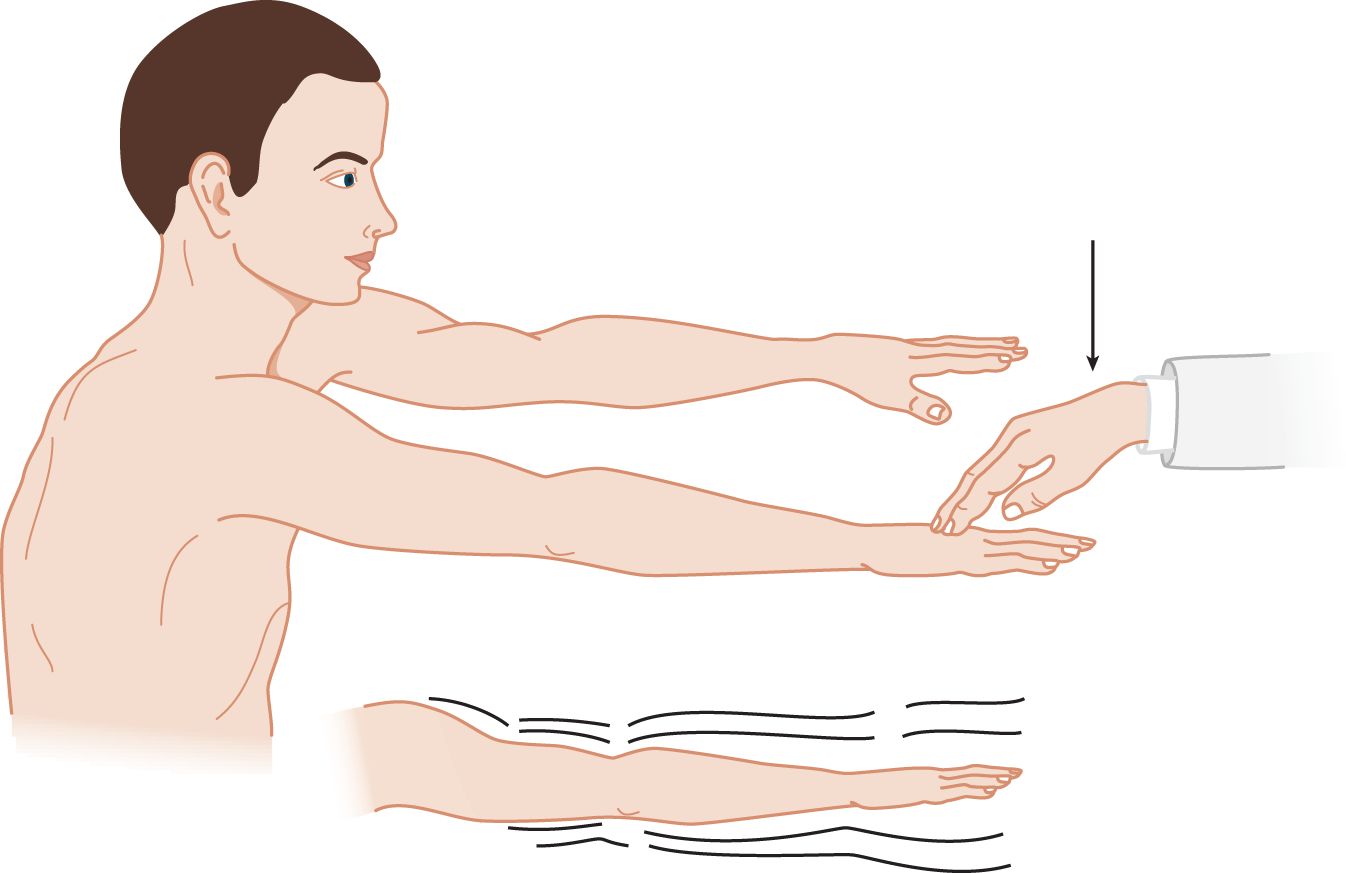
FIGURE 8-8. Wrist-tapping test for abnormal overshooting oscillation after sudden displacement of a part that is maintaining a volitional posture. The thin arrow shows the direction of the examiner’s push, which displaces the part.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


