TABLE 5-1 • The Five Major Eye-Movement Systems
System | Function or characteristic |
Saccadic system | Produces all volitional movements and the fast phase of reflex eye movements (frontal lobe) |
Fixation (position maintenance system) | Fixates and maintains eyes on target and locks them in unison to fuse the two retinal images into one visual image (occipital lobe) |
Smooth pursuit system | Keeps eyes on moving target (occipital lobe) |
Vergence system | Converges or diverges eyes for near or distant targets (occipital lobe) |
Counter-rolling system | Vestibular and neck proprioceptive system: counter-rolls the eyes to keep them fixed on the visual target in compensation for head movement |
1. Saccadic system: saccade = to jerk or rein in. Saccadic movement describes eye movements by increments or jerks, like a ratchet (Kennard et al., 1994).
a. Self-demonstration of saccades:
i. Look straight ahead. Then, while keeping your head completely still, move your eyes all the way to the right and hold them there.
ii. With your head still, very slowly try to move your eyes as continuously and smoothly as possible all the way from the right to the left. Attend to how your eyes move. Do they move continuously and smoothly or by incremental jerks? _________
b. You cannot move your eyes smoothly voluntarily. All volitional eye movements require saccades.
c. Fronto-tegmental corticobulbar pathways are thought to mediate all such saccades (Fig. 5-1).
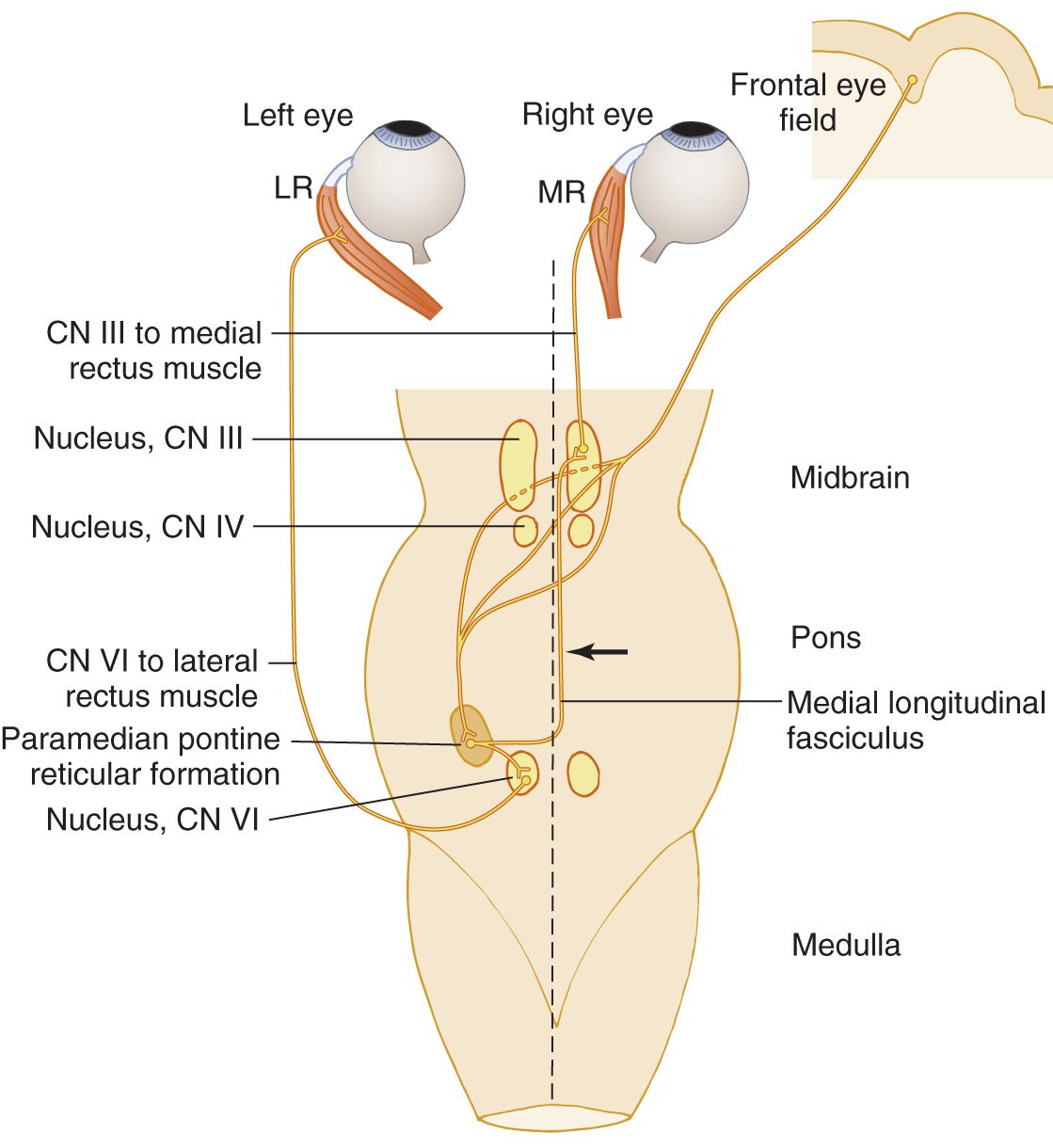
FIGURE 5-1. Dorsal view of the brainstem to show corticobulbar pathways for voluntary conjugate lateral eye movements.
d. The supplementary motor area, substantia nigra, superior colliculus, vermis, fastigial nucleus, reticular formation, and vestibular system play roles in saccadic production and accuracy.
e. To test for saccadic accuracy: Hold up your index fingers about 18 inches apart and ask the patient (Pt) to look at one and then the other. Move the targets around to require the Pt to look at different sites. Saccadic accuracy depends on connections in the dorsal part of the cerebellar vermis and the fastigial nuclei.
2. Fixation (position holding) system
a. After you choose a visual target and voluntarily saccade onto it, fixation reflexes hold the eyes on the target and promote fusion of both retinal images into one sharp visual image. Breaking away from the chosen target requires generation of another saccade to jerk the eyes away and onto a new visual target. Fixation reflexes tend to keep the eyes on target when the head moves.
b. Retino-geniculo-occipito-tegmental and retino-occipito-fronto-tegmental pathways mediate fixation and fusion.
3. Smooth pursuit system
a. Self-demonstration of smooth pursuit:
i. Keep your head still and facing straight ahead throughout this exercise.
ii. Move your eyes all the way to the right, but this time hold up your finger about 30 cm away, fixate on it, and move it slowly all the way across from right to left. Allow only your eyes to pursue it. If you actually keep your head still and keep your eyes fixed on the moving finger, you will experience smooth rather than saccadic movement.
iii. Practice eliciting smooth pursuit on another person.
b. The smooth pursuit system keeps the eyes on target when the target moves. Drug intoxication, including alcohol, causes irregular or jerky rather than smooth pursuit of a moving object.
c. Retino-geniculo-occipito-parieto-frontal-tegmental pathways mediate smooth pursuit.
4. Vergence system
a. This system converges or diverges the eyes to ensure fusion of the two retinal images and appropriate refraction when the person looks at a near or distant visual target. It also keeps the eyes on target as the target moves toward or away from the person. This system mediates the accommodation reflex.
b. The vergence system depends on retino-geniculo-occipito-tegmental pathways.
5. The counter-rolling system of the eyes
a. Self-demonstration of counter-rolling of the eyes:
i. Hold up your finger at arm’s length, directly in front of you. Then, while holding your finger still, fixate on it and move your head horizontally and vertically.
ii. Your eyes will reflexly counter-roll against the direction of head movement to maintain fixation on the chosen visual target.
b. In the alert Pt, two systems collaborate to hold the eyes on target:
i. The ocular fixation system.
ii. The proprioceptive system. It arises in the vestibule and neck. It counter-rolls the eyes, an action called the vestibulo-ocular reflex (VOR).
c. In the comatose Pt who cannot fixate, the examiner (Ex) can move the Pt’s head (doll’s eye maneuver) to test the counter-rolling reflex (VOR). See VOR in Chapters 9 and 12. The absence of fixation during coma makes counter-rolling depend on the VOR.
6. In summary
a. If the visual target moves, the smooth pursuit system holds the eyes on target.
b. If the Pt is conscious and if the head moves, the fixation reflexes and VOR keep the eyes on a target that is still.
c. If the Pt is unconscious, only the proprioceptive reflexes can act, because the Pt cannot fixate.
7. Now, we have not just loaded five more things to memorize on you. If you did the exercises, the following mnemonic will work:
8. The foregoing exercises involved a still head or a still target. If the head and eyes both move toward a target, the counter-rolling by the VOR opposes the head and eye movement and undergoes suppression.
C. The corticopontine pathway for voluntary conjugate horizontal eye movements
1. Different pathways mediate conjugate vertical and horizontal eye movements. The pathway for voluntary conjugate horizontal eye movements begins in the cortex of the posterior-inferior part of the frontal lobe and runs to the pontine tegmentum (Fig. 5-1).
2. This cortical pathway terminates in the paramedian pontine reticular formation (PPRF) near the midline of the pons and responsible for generating horizontal eye movements. This region sends fibers to the ipsilateral abducens nucleus. The abducens nucleus sends fibers via cranial nerve (CrN) VI to the ipsilateral lateral rectus muscle and, via the medial longitudinal fasciculus (MLF), also sends fibers that cross to the opposite medial rectus subnucleus. The medial rectus subnucleus innervates the medial rectus muscle. Thus, stimulation of the right PPRF or right abducens nucleus will make the eyes deviate conjugately to the right. (Frohman et al., 2001; Fig. 5-1).
3. Effects of interruption of the horizontal gaze pathway
a. Interruption of the cortical efferent pathway for horizontal movements rostral to its decussation results in deviation of the eyes ipsilateral to the lesion (the eyes “look toward the lesion”), because the opposite pathways are intact and continue to convey tonic innervation.
b. Interruption caudal to the decussation results in deviation to the side contralateral to the lesion.
4. Effects of interruption of one MLF
a. After interruption of one MLF, say the right (tip of the arrow in Fig. 5-1), the right eye will not adduct when the Pt attempts to look to the left (Ross and DeMyer, 1966).
b. In addition to adductor paralysis on left lateral gaze, the Pt’s left eye undergoes oscillations, a feature that you cannot deduce from the diagram. Such ocular oscillations are called nystagmus. Hence, a second sign of the MLF syndrome is monocular nystagmus of the abducting eye. At rest, the eye has no nystagmus. It occurs only during abduction. The symptoms accompanying the eye movements are diplopia and oscillopsia (oscillating vision).
c. These two signs, paralysis of the adducting eye and nystagmus of the abducting eye, appear only on gaze to the opposite side of the MLF lesion.
i. The eyes adduct normally on convergence.
ii. The corticobulbar pathways for convergence and vertical eye movements run directly into the mesencephalon to the lower motor neurons (LMNs) of the III and IV nuclei, rather than looping down into the pons and returning in the MLF.
d. After a left-sided MLF lesion, what would be the only direction of gaze that would cause diplopia and heterotropia? (To reason out the answer from Fig. 5-1, draw in the pathway from the left cerebral hemisphere with colored pencil)  looking right/
looking right/ looking left/
looking left/ looking straight ahead. (
looking straight ahead. ( looking to the right)
looking to the right)
e. Summary of the signs and symptoms of the MLF syndrome
i. The signs of a unilateral MLF lesion consist of heterotropia and monocular nystagmus. They appear only when the Pt attempts to look away from the side of the interruption of the MLF. Other eye movements, including conjugate vertical gaze and pupillary responses, remain normal.
ii. The symptoms of a unilateral MLF lesion may include diplopia and oscillopsia.
iii. During horizontal gaze, the Pt cannot  abduct/
abduct/ adduct the eye ipsilateral to the lesion and shows monocular nystagmus of the contralateral,
adduct the eye ipsilateral to the lesion and shows monocular nystagmus of the contralateral,  abducting/
abducting/ adducting eye. (
adducting eye. ( adduct;
adduct;  abducting)
abducting)
f. Describe the signs of a bilateral MLF lesion at the level of the arrow in Fig. 5-1.
_________
_________
g. Would the eyes of a Pt with a bilateral MLF lesion converge during accommodation?  Yes/
Yes/ No. Explain.
No. Explain.
_________ Yes. The convergence pathways run directly into the midbrain without involving the MLF.)
Yes. The convergence pathways run directly into the midbrain without involving the MLF.)
D. Bilateral destruction of the frontal corticotegmental pathway for horizontal gaze (supranuclear paralysis of gaze)
1. If bilateral lesions destroy the pathway to the brainstem from the frontal eye fields, the Pt cannot produce saccades to voluntarily move the eyes to either side, but the vestibular counter-rolling reflexes can still move the eyes to the sides. Some weakness of vertical gaze is present or will develop because the Pt often has a progressive dementia or severe bilateral cerebrovascular disease.
2. After paralysis of voluntary movements, the vestibulo-ocular and fixation reflexes tend to become overly active (“released”). Indeed, the full movement of the eyes by reflexes establishes that the LMNs of the ocular motor system are intact and that the cause for the paralysis of eye movements is supranuclear, in the upper motor neurons (UMNs). The Pt cannot voluntarily break fixation by moving the eyes and must blink or jerk the head to interrupt the afferent arc that maintains the fixation reflex. This condition when seen congenitally in children is called Cogan syndrome of oculomotor apraxia.
3. The slow deviation phase of calorically induced or optokinetic nystagmus remains but the saccadic kickback fails, because the saccades depend on the integrity of the frontal eye fields.
4. Another form of progressive supranuclear palsy, called the Steele–Richardson–Olszewski syndrome, affects vertical movements first, usually the downward before the upward (Liu et al., 2001; Steele, 1994), and then horizontal movements. The lesion responsible affects the midbrain and basal forebrain structures.
E. Cortical pathway for vertical eye movements
1. Pathways for vertical eye movements arise diffusely from frontal and parietal cortices. Like the convergence pathways, they project directly to the midbrain, without looping down into the pons and reflecting back in the MLF.
2. The cortical pathway for conjugate upward eye movements runs in the tegmentum dorsal to the pathway for downward movements (Bhihdayasiri et al., 2000).
a. Parinaud syndrome: Dorsal compression of the midbrain, as from a pineal tumor, mesencephalic hemorrhage, or obstructive hydrocephalus, will selectively impair upward vertical movements (Parinaud syndrome) before affecting downward gaze. Convergence palsy and light-near dissociation of the pupils are commonly present also.
b. Bell phenomenon (Sir Charles Bell, 1774-1842)
i. When most persons attempt to close their eyes, the eyeballs automatically rotate upward and somewhat outward. This associated eyeball movement, called Bell phenomenon, occurs during voluntary eyelid closure or sleep, but closure of the eyelid by the orbicularis oculi muscle obscures it.
ii. In a Pt with UMN paralysis of voluntary elevation of the eyes, the presence of Bell phenomenon proves that the midbrain and LMNs for the eye elevation are intact.
iii. The Ex will most easily see Bell phenomenon if interruption of the facial nerve paralyzes the face, preventing eyelid closure. Idiopathic interruption of the facial nerve is called Bell palsy (Chapter 7).
3. The cortical pathway for conjugate downward eye movements runs into the midbrain tegmentum dorsomedial to the red nucleus, where a lesion may selectively affect it, sparing vertical and horizontal eye movements (Bhihdayasiri et al., 2000). The lesion interrupts connections with the rostral interstitial nucleus of the MLF (riMLF), the saccadic brainstem center for vertical eye movements (Fig. 5-2), just as the PPRF is a brainstem center for horizontal saccades (see Fig. 5-1).
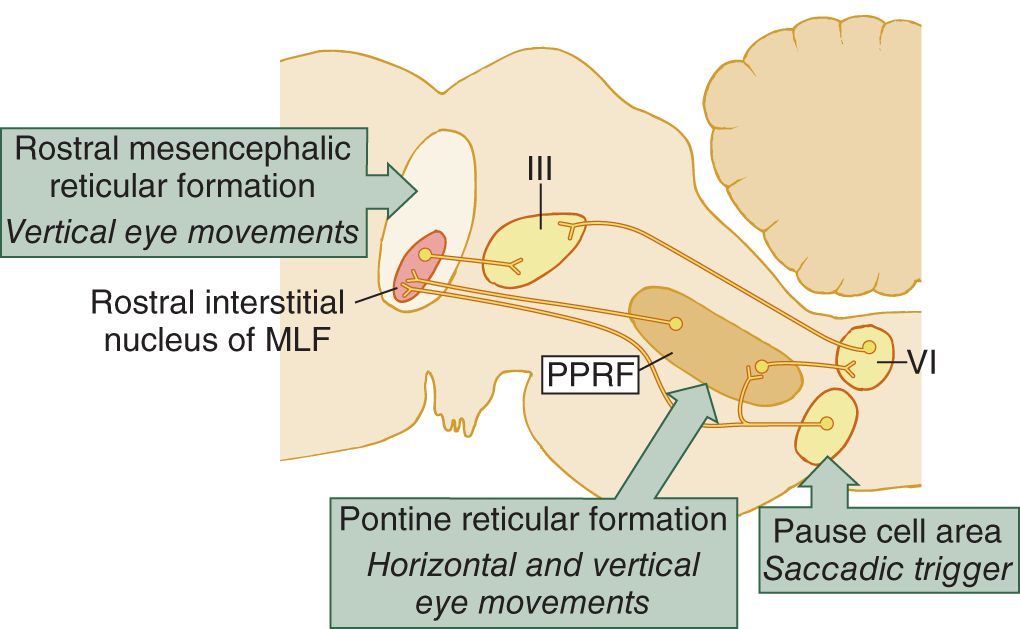
FIGURE 5-2. Sagittal section of the brainstem. The riMLF and the PPRF act as brainstem centers for the generation of saccades. The riMLF mediates vertical saccades and the PPRF mediates the horizontal. Lesions of these regions or their cortical input pathways impair the saccadic actions necessary for volitional vertical and horizontal gaze. PPRF = paramedian pontine reticular formation; riMLF = rostral interstitial nucleus of the medial longitudinal fasciculus. (Reproduced with permission from Kennard C, Crawford TJ, Henderson L. A pathophysiological approach to saccadic eye movements in neurologic and psychiatric disease. J Neurol Neurosurg Psychiatry. 1994;57:881-885.)
F. Comparison of the LMN (nuclear), internuclear, and UMN (supranuclear) lesions of the ocular pathways
1. Interruption of LMNs of CrN III, IV, or VI paralyzes individual extraocular muscles (EOMs) or sets of muscles. No reflex or voluntary act can activate a muscle affected by LMN paralysis. The Pt suffers diplopia and strabismus.
2. Interruption of internuclear pathways, such as the MLF, paralyzes only movements mediated through that pathway. Other reflexes or voluntary pathways can still activate the ocular muscles. The Pt has diplopia only when that pathway should participate, as in the MLF syndrome.
3. Interruption of supranuclear pathways, the UMNs of the ocular motor system, impairs voluntary conjugate eye movements, not the actions of the individual EOMs. Reflexes can still activate the muscles. The Pt does not have diplopia. We can conclude that ocular movements illustrate the previously announced epigram that UMN lesions paralyze  movements/
movements/ muscles, whereas LMN lesions paralyze
muscles, whereas LMN lesions paralyze  movements/
movements/ muscles. (
muscles. ( movements) (
movements) ( muscles)
muscles)
4. In fact, the MLF syndrome helps to emphasize the principle that, when a muscle is paralyzed for only one movement and participates in others, the responsible lesion cannot be at the LMN level.
G. The concept of a head- and eye-centering center
1. Self-demonstration of the head- and eye-centering tendency: You can stare straight ahead, more or less vacantly or vapidly for some period, with no discomfort. Such staring spells, trances, or “tuning out” spells are common, even in infants, and especially in many intellectually impaired and learning-disabled children. But if you stare fully to one side, or up or down, discomfort soon demands that you return to the neutral, primary position. To experience the centering demand do this:
a. Seat yourself comfortably. Pick out a target far to your left, almost behind you. Then turn your head and especially your eyes to the left and keep them there as long as possible, gazing at the target. Blink as necessary but do not break fixation. As you keep the eyes deviated, attend to your own sensations. Time how long you can maintain the deviated position. Now do the experiment.
b. After some period of increasing discomfort as you keep your head and eyes deviated, a physiologic imperative will demand that you return them to the primary position, sometimes after as little as 30 seconds. You may feel the discomfort as anxiety, vertigo, blurred vision, or even headache. In any event, notice that you felt a considerable relief when you returned to the primary position. Something about the organism wants its eyes and head straight ahead. In fact, many brain-impaired Pts cannot sustain deviation for even 30 seconds, a sign called motor impersistence.
c. Deviation of the eyes for any reason, voluntary or reflex, triggers a saccade that kicks the eyes back to the primary position, unless overridden by volition, as in the previous experiment. Inhibiting the saccadic kickback reflex requires some of voluntary effort in the eye deviation experiment as does overcoming visco-elastic forces in the eye socket consequent to deviating the eyes.
2. Many vectors compete to determine the position of the head and eyes at any given instant.
a. The will or intent of the bearer of the eyes, the emotional state, the survival requirements and advantage-seeking possibilities of the circumstances, and the attractiveness of the visual display.
b. The position of the head in relation to space, movement, gravity, and the activity of the vestibular system.
c. The illumination and conditions of vision.
d. The refractive capability of the eyes and the distance of the visual target.
e. The demands of binocular fixation and image fusion.
3. Origin of vectors that determine head and eye position: Vectors competing for the control of the head and eyes originate at every level of the neuraxis: posterior frontal cortex (Gaymard et al., 2000), basal motor nuclei, diencephalon, reticular formation, cerebellum, and even the rostral part of the spinal cord. Hence, lesions at any of these levels can more or less influence the movement and position of the head and eyes.
a. For each head and eye position, vectors act to keep them there and others to move them away. In the aggregate, these opposing vectors result in tonic innervation. The continuous active contraction of the intraocular muscles and EOMs maintains them in a state of oppositional tension that positively determines eye position. The head and eyes seek the null, primary position, not because of the absence of stimulation but because all vectors balance out.
b. To avoid chaos, some circuitry must integrate and balance these vectors. Although no head- and eye-centering center exists as such in one specific site, the concept of a head- and eye-centering center that balances the right and left vectors and the up and down vectors explains a number of clinical phenomena.
4. A tale of opposing vectors
a. Normally, the right cerebral hemisphere tends to drive the head and eyes to the left, balanced by the left hemisphere trying to drive them to the right. The vectors from the two hemispheres actively oppose and counterbalance each other. Study Figs. 5-3A to 5-3C.
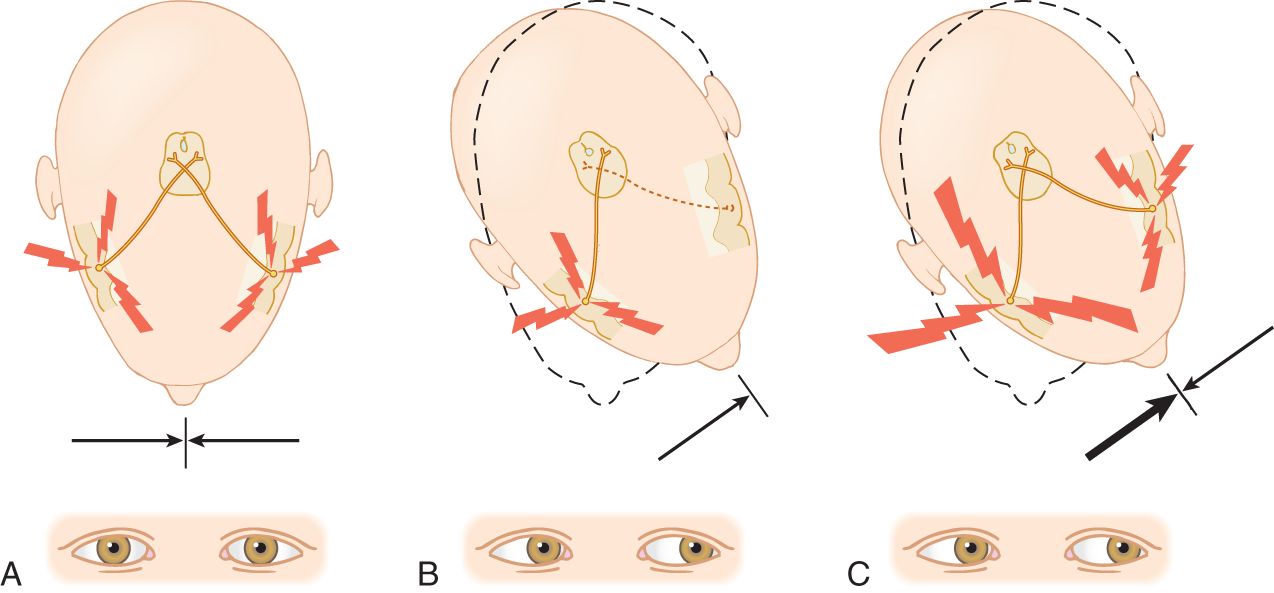
FIGURE 5-3. A head- and eye-turning center (conjugate gaze center) occupies the posterior part of the frontal lobe (zigzag lines). The arrows beneath A through C represent the strength of a vector originating on one side, acting to turn the head and eyes contralaterally. Notice the corticobulbar pathway to the pons and that it decussates. Relate this pathway to Fig. 5-1. (A) Normal resting condition. The vectors are equal and the head and eyes remain straight ahead. (B) A lesion has destroyed the left conjugate gaze center. The vector from the right center acts unopposed, deviating the head and eyes to the left. (C) An epileptogenic lesion has caused an excessive discharge of impulses from the right conjugate gaze center. The vector from the right hemisphere overpowers the one from the left. The head and eyes deviate to the left but for an entirely different reason than in B.
b. The corollary is that any persistent conjugate deviation of the eyes or head and eyes in any direction means some disorder of the central nervous system (CNS) pathways. If only one eye deviates, the lesion affects the LMNs or neuromuscular level.
H. Effect of destructive cerebral lesions on the position of the eyes and head
1. A sudden massive lesion of one cerebral hemisphere, say the right, will interrupt the corticobulbar and corticospinal tracts, causing a complete left hemiplegia. This lesion also nullifies the vector arising in the right hemisphere that should continually strive to turn the eyes and head to the left (Fig. 5-3B).
2. What would you expect the position of the head and eyes to be in the foregoing Pt?  midline/
midline/ turned to the left/
turned to the left/ turned to the right. Explain.
turned to the right. Explain.
_________
_________ turned to the right. The lesion has eliminated the vector from the right hemisphere that always tries to turn the head and eyes to the left. The vector from the left hemisphere acts unopposed. Therefore, the head and eyes turn to the right, toward the side of the lesion and opposite to the hemiplegic side.)
turned to the right. The lesion has eliminated the vector from the right hemisphere that always tries to turn the head and eyes to the left. The vector from the left hemisphere acts unopposed. Therefore, the head and eyes turn to the right, toward the side of the lesion and opposite to the hemiplegic side.)
3. The head and eye deviations are most prominent in the acute phase of the lesion (Tijssen et al., 1991). The head- and eye-centering mechanisms reset themselves quickly, but the hemiplegia endures.
I. Effect of irritative lesions on the position of the head and eyes
1. Some cerebral lesions irritate cortical neurons, causing them to fire excessively. Such an irritative lesion initiates epileptic seizures. Electrical stimulation of the cortex has the same effect. Suppose a Pt has a focal epileptic seizure that begins by turning the head and eyes to the right. You would anticipate that the Pt had an epileptogenic focus in the  right/
right/ left frontal lobe (Fig. 5-3C). (
left frontal lobe (Fig. 5-3C). ( left)
left)
2. During the epileptic discharge, the excess of impulses on the left side overcomes the normal vector from the right. After the epileptic cataclysm has subsided, the excessive discharge has metabolically exhausted the neurons in the seizure focus, rendering them temporarily nonfunctional. Immediately after an epileptic seizure caused by a left-sided cerebral lesion, to which side would the head and eyes be turned?  right/
right/ left. Explain.
left. Explain.
_________
_________ left. Because the left eye- and head-turning center is exhausted, the right acts unopposed. The head and eyes turn to the left, opposite to the direction that they turned during the seizure.)
left. Because the left eye- and head-turning center is exhausted, the right acts unopposed. The head and eyes turn to the left, opposite to the direction that they turned during the seizure.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


