Fig. 20.1
Preferential access routes to the interbody space at varying spinal segments
Lateral – Open lateral approaches have been used for decades to access the mid-lumbar spine. Originally used for the treatment of Pott’s disease, this method later found utility for managing thoracolumbar fractures and releasing the mid-lumbar spine for ASD pathologies. This method has the morbidities associated with the ALIF approach and originally also required an extensive disruption of the soft tissues via the thoracoabdominal approach. Its use has been largely supplanted by less invasive methods such as the extreme lateral interbody fusion (XLIF) and direct lateral interbody fusion (DLIF). These approaches are discussed extensively in Chaps. 24, 25, 26, 27, 28, 29, 30, 31, and 32. Expandable cages also have potential applications in this arena.
Oblique – A new method approaching the spine from an intermediary approach has also been developed (Fig. 20.2). Limited data are available on the safety and efficacy of this approach, particularly for treating spinal deformities, but the oblique lateral interbody fusion (OLIF) has the advantages of accessing the spine posterolaterally without any bone removal. More data is needed on the safety and efficacy of this method for treating spinal deformities.
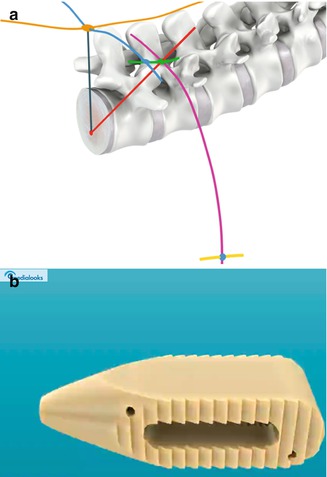
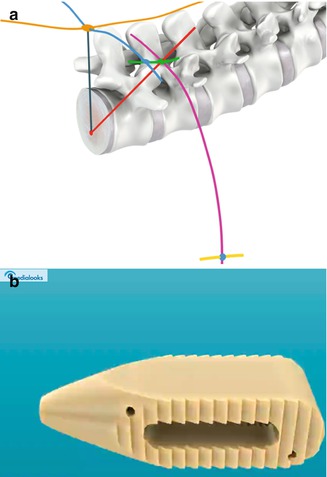
Fig. 20.2
Oblique lateral interbody fusion. (a) Access is through Kambin’s triangle, and (b) a cannulated and bulleted cage is inserted through the inferior neuroforamen
Trans-sacral – Approaching the lumbosacral junction via a low incision through the presacral fat pad has also been popular (see Chap. 35). This method, which allows an interbody fusion at L5–S1 and occasionally L4–5, has the advantage of allowing for an anterior interbody spacer to be placed at the lumbosacral junction with the patient in the prone position. This accomplishes the goal of stress shielding the sacral screws while not excessively prolonging the operation with a second position surgical approach.
Posterior – Because the above approaches are covered in other chapters in this textbook, this discussion on expandable cages will focus on the use of these devices in minimally invasive posterior surgeries.
20.3 Problems with Traditional Posterior Interbody Cages
Posterior lumbar interbody fusion (PLIF) has been a widely utilized technique since its introduction by Ralph Cloward a half century ago [2]. This method is robust as it completely treats a spinal segment with decompression, fixation, and fusion. It is effective as a treatment for segmental correction of spinal deformities [5].
While powerful as a technique, rates of new neural symptoms can be seen in as many as 7 % of patients undergoing PLIF. Much of this has been attributed to the neural retraction needed for cage placement. Thus, the technique of transforaminal lumbar interbody fusion (TLIF) was innovated by Harms. This method approaches the disc space more laterally and from only one side, thus reducing the likelihood of nerve root retraction and its attendant clinical problems. Regardless, both methods typically involve some amount of nerve root manipulation, particularly to place an appropriately sized graft.
With the advent of MIS PLIF and TLIF, new problems emerged, much of this was related to interbody graft undersizing. This was due to less complete disc space preparation and a reduced ability to distract upon pedicle screws to allow cage placement. While potentially acceptable in cases of degenerative disease, treatment of ASD requires special attention to spinal alignment and maintenance/restoration of lordosis.
20.4 Kambin’s Triangle and the Geometry of Interbody Cages
Placement of an interbody grafts involves adequate disc space clearance and preparation, selection of an ideal height spacer, management of neural tissues, and graft insertion. Creation of a corridor of space requires an understanding of the geometry of these corridors. While selection of the ideal spacer height is a relatively straightforward but arbitrary decision, the confines limiting cage placement are to some degree fixed and real. The relationship of the traversing and exiting nerve roots, lateral removal of the facet joint, scarring and adhesions, and the elasticity of the neural elements all influence the available space for cage placement. Furthermore, the cage shape, route of entry, and the trajectory of approach all affect the space needed.
In a previous report by Barnes et al., it was shown that, in order to achieve a predefined spacer height, placement of a cylindrical cage would have to require more nerve root retraction than a rectangular cage. They investigated this in a cohort of 49 patients. Clinically, this translated to a 13.6 % rate of permanent nerve root injuries in patients with cylindrical cages vs. 0 % in rectangular cages [1]. Currently, nearly all cylindrical cages have been replaced by impacted rectangular implants.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








