1
Foramen Magnum Decompression
Ashwini D. Sharan, Laura Snyder, and Gregory J. Przybylski
Description
To achieve adequate decompression of the posterior cranial fossa without injury to the neurovascular structures at the craniocervical junction.
Key Principles
Bony removal should include sufficient occipital bone and upper cervical lamina to incorporate both the rostral-caudal as well as the lateral extent of pathology while protecting the transverse sinus and vertebral arteries. Dural expansion may be an additional component of decompression of the upper cervical spinal cord and lower medulla.
Expectations
Although spinal instability after foramen magnum decompression is not common, excessive lateral decompression in conjunction with disruption of posterior craniocervical ligaments may result in hypermobility of the craniocervical junction. One must be prepared to encounter a vestigial venous sinus within the dural leaves at the foramen magnum.
Indications
Chiari malformation, achondroplasia, syringobulbia, basilar invagination, complex C1, C2 fractures.
Contraindications
Adequate treatment of associated hydrocephalus should be achieved prior to foramen magnum decompression. Similarly, supratentorial masses should be excluded before opening the dura in the infratentorial posterior fossa.
Special Considerations
Magnetic resonance imaging (MRI) of the brain and craniocervical junction preoperatively is imperative to define the extent of compression. The extent of caudal cerebellar displacement (for Chiari malformation), hydrocephalus, or other supratentorial mass lesions can be detected on MRI. Additionally, the venous sinuses and vertebral artery are visualized on MRI. A computed tomography (CT) scan may be beneficial in gauging the thickness of the keel and bony anatomy when considering instrumentation of the craniocervical junction.
Special Instructions, Position, and Anesthesia
The patient is positioned prone with a Mayfield pin head holder. Maintaining the head in a flexed posture facilitates decompression, but may not be appropriate during stabilization procedures. Neurophysiologic monitoring may be used to monitor spinal cord and brainstem function, and arterial monitoring is beneficial in detecting blood pressure lability and bradycardia from brainstem compression.
Tips, Pearls, and Lessons Learned
Flexion of the neck so that the mandible is two fingerbreadths away from the sternum facilitates separation of the inferior occipital margin of the foramen magnum and the posterior atlas, thereby improving ease of craniocervical ligament dissection from the dura. Extensive flexion of the neck may exacerbate postoperative swallowing or respiratory problems.
Although the tentorium cerebelli and the transverse sinus are typically in the same axial plane as the upper third of the ear lobe, patients with hindbrain malformations may have a small posterior fossa and therefore a low-lying transverse sinus. A gross way to identify the transverse sinus is to connect a curved line from the mastoid process to the external occipital protuberance (EOP, or inion). Bony removal should be initiated inferior to these points to avoid sinus injury. Venous sinus bleeding can be controlled by pinching the inner and outer dural leaves together or sometimes by using vascular clips.
Subperiosteal dissection along the atlas should be limited to 1.5 cm from the midline of the posterior tubercle of the atlas in adults and 1 cm in children. Dissection beyond this must be performed with extreme caution to avoid injury to the vertebral artery. A large venous plexus is typically encountered at the lateral margin of decompression at the craniocervical junction, signifying proximity to the vertebral arteries.
Difficulties Encountered
The midline bony keel is thicker than the paramedian occipital bone. Burr holes on either side of the midline keel at the rostral extent of the craniectomy can facilitate separation of the dura from the inner skull table. Rapid bleeding from the occipital or marginal sinus during dural opening may occur, but can be avoided by surgical clip placement on both sides of the dural opening in advance of the incision. Bleeding from emissary veins during subperiosteal dissection of the occiput may also occur, but can be controlled with bone wax.
Key Procedural Steps
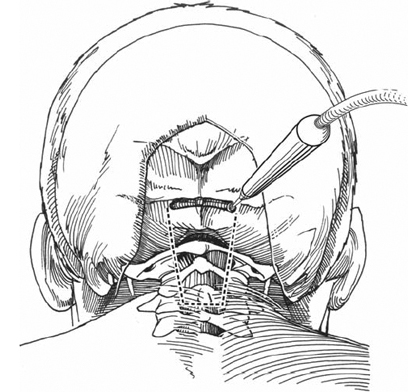
Shave and preparation of the skin should extend from above the EOP to the lower cervical spine. A midline incision with subperiosteal dissection provides exposure from the EOP to the predetermined caudal cervical lamina chosen for removal (Fig. 1.1). A Y -shaped incision of the fascia provides for a fascial flap attached to the superior nuchal line, aiding closure. Exposure is maintained with cerebellar retractors. Margins of the foramen magnum are defined with a curette. Preservation of muscular and ligamentous attachments of C2 are recommended if the axis is not removed in the decompression.
Typically, a 3 x 3 cm section of occipital bone with the posterior rim of the foramen magnum is removed. A high-speed drill is used to create a craniectomy on either side of the midline bony keel. The dura is dissected from the inner skull table as needed as the bone is gradually lifted away (Fig. 1.2). Additionally, it will be beneficial to thin the midline keel and the foramen magnum with the drill until a thin remnant of bone remains. This thinned bone easily cracks as a curette is then used to lift the isolated occipital bone starting at the foramen magnum away from the posterior fossa. Extreme care should be exercised when placing instruments between the bone and the dura in a compressed foramen magnum. Similarly, narrow troughs can be drilled at the lateral borders of each lamina to be removed until a thin remnant of bone remains. The detached lamina can be lifted away from the spinal canal with a rongeur while a curette is used to separate the underlying dura from the inner laminar surface. Rongeurs can be used to enlarge the lateral extent of decompression if needed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








