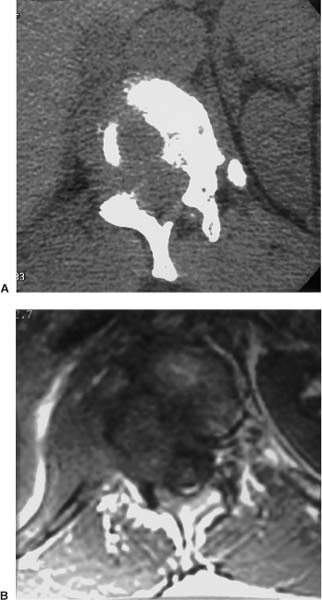
18 Frameless stereotaxy for intraoperative navigation during spinal tumor resection can be an effective tool for the anatomic localization of defined tumor margins and for precise placement of segmental spinal instrumentation. Anatomic localization of tumor margins can be advantageous for en bloc resections and for when lesions are near vulnerable vascular and neurologic structures (Fig. 18-1). Intraoperative navigation techniques may improve the accuracy of pedicle screw placement, particularly in complex cases involving the thoracic and cervical spine.1–5 High-resolution computed tomography (CT) and magnetic resonance imaging (MRI) typically provide two-dimensional (2D) images of pathologic anatomy. With its ability to provide multiplanar views, MRI, in particular, has improved diagnostic applicability and the precision of treatment substantially in the past decade. Contemporary scanners acquire the anatomic data in a three-dimensional (3D) volume but usually still depict the image in two dimensions for use by diagnosticians and clinicians. The value of 3D-anatomic representations is an emerging aspect of diagnosis, treatment planning, surgical accuracy, and real-time intraoperative surgical navigation. Furthermore, 3Danatomic data sets from CT and MRI can be “merged” accurately into a combined data set. This feature is particularly valuable in the application of skull base and spinal tumors. The surgeon has the ability to “window” the amount of CT data (for navigation in bone) and MRI data (for navigation in tissue) simultaneously and instantaneously to “match” the “flow” of the operative procedure (Fig. 18–2). The source data sets derived from CT and MRI representing a 3D geometrically precise description of a patient’s unique anatomy can be applied to 3D treatment planning in a “virtual patient” data set.6 Precise alignment of the actual patient with the virtual patient can be achieved routinely with coregistration of less than 1 mm in the spine, using infrared digital localization techniques (Fig. 18–3).7 Registration techniques include correlation of specific anatomic points (fiducials) on the radiologic data set and patient (paired-point technique) and correlation of specific surface contours on the radiologic data set and patient (surface-merge technique) (Fig. 18–4). An operative treatment platform using these techniques empowers a surgeon to examine and interpret abnormal patient anatomy, to plan a precise operative intervention in virtual space, and to transfer that data to the operating room with submillimetric accuracy. Intraoperative image acquisition of real-time data is an area of significant interest. The primary disadvantage of image-guided surgery is the dependence on preacquired image data. Fluoroscopy can be used in spinal navigation, either to augment a preacquired 3D data set or alone as the primary multiplanar 2D data set. Furthermore, efforts at integrating intraoperative MRI and CT into a navigational platform continue to progress. FIGURE 18–1 (A) Coronal magnetic resonance imaging (MRI) of a C3 malignant neurofibroma. (B) Axial MRI shows displacement of the spinal cord medially and the vertebral artery laterally. (C) With the aid of intraoperative navigation, the tumor margin was accurately localized for complete resection, and C2 pedicle and C3–C4 lateral mass screws were placed for fixation. Pedicle screws and rods provide superior stability compared with other posterior spinal fixation techniques. Specifically, biomechanical studies have suggested that pedicle screws provide more rigidity and construct stiffness than other posterior fixation techniques.8–10 This increase in rigidity permits shorter constructs to be used and decreases the time patients need to wear an external orthoses. Since King11 attempted to place the first transfacet screw in 1944, the technique of applying transpedicular screws for posterior fixation to treat spinal instability has evolved continuously. Even before the Food and Drug Administration upgraded transpedicular screws from a class III to a class II device in July 1998, may surgeons considered pedicle screws to be the best and most rigid form of posterior spinal fixation. FIGURE 18–2 (A) Computed tomography (CT) scan of a thoracic metastatic tumor. (B) MRI shows distinct tumor margin used to obtain complete resection with intraoperative navigation. Before the advent of intraoperative navigational techniques, pedicle screw placement in the lumbar spine was becoming widespread. The shape of the lower lumbar pedicles is uniform, and their dimensions are predictable. These features allow relatively safe and routine cannulation by using standard anatomical landmarks and intraoperative radiologic confirmation. Because thoracic pedicles are smaller and their 3D morphology is more complex than lumbar pedicles, transpedicular screw placement in the thoracic spine can be extremely challenging, and the technique has not been advocated widely. Anatomic studies have shown that the diameter, shape, and angle of thoracic pedicles vary considerably (Fig. 18–5) in terms of both the relationship of the transverse process to the axis of the pedicle and the angle of the pedicle to the vertebral body.12 Given the proximity of the thoracic pleura, nerve roots, and spinal cord, serious complications can be associated with a less than perfectly placed thoracic pedicle screw. In the cervical spine, pedicular fixation at C6 and C7 is associated with the same technical challenges encountered with thoracic pedicle fixation. Frameless stereotactic techniques can also improve the accuracy and safety of transarticular screw stabilization at C1–C2. The wealth of data collected about the anatomy of the spinal pedicles12–18 has been used to develop techniques intended to decrease the complications associated with pedicle screw placement.19,20 Because of the anatomic variability of the thoracic vertebrae, freehand placement of thoracic pedicle screws using anatomic landmarks can be imprecise and thus lead to errors in screw placement. Morphometric studies have shown that pedicular size varies from the smallest mean transverse diameter of 4.5 mm at T4 to the largest mean transverse diameter of 7.8 mm at T12.9 Medial errors are less forgiving in the thoracic spine because the spinal cord is less mobile than the nerve roots in the cauda equina. Lateral perforations of the pedicular cortex are potential threats to the pleural cavity and great vessels.21 Anatomic studies have shown that the placement of pedicle screws is feasible in the thoracic spine.18 Spine surgeons, however, may be reluctant to attempt to place thoracic pedicle screws given the technical difficulty and inherent risks associated with the technique. Clinical and cadaveric studies have shown that 15 to 50% of pedicle screws violate the pedicular cortex when placed using anatomic landmarks, fluoroscopic techniques, or both.19,22,23 Violations of the pedicular cortex have been analyzed by direct visualization in cadaveric specimens and by plain radiography and thin-cut CT (Table 18–1). Image-guided stereotaxy provides 3D intraoperative guidance that is well suited for placing cervical, thoracic, and upper lumbar pedicle screws. The accuracy of this technology in cadaveric studies has been extremely encouraging.23–25 Determining the point of screw entry in the thoracic spine is much more difficult compared with the lumbar pedicle. The general rule, which places the rostralcaudal center of the pedicle at the midpoint of the transverse process, does not necessarily apply to the widely variable thoracic spine.12 Not only does this point vary rostrally to caudally in the thoracic spine but also segmental variability in the horizontal plane is a concern. Moreover, unlike the large ovoid lumbar pedicle, the cross-sectional morphology of a single thoracic pedicle also varies widely in the coronal plane (Fig. 18-5).16 Several techniques, based on anatomic landmarks and intraoperative fluoroscopy, have evolved to improve the accuracy of determining the center of a pedicle in the thoracic spine.19,20 Nonetheless, given the required accuracy and the limited margin of tolerable error, several authors have concluded that the configuration of some thoracic pedicles may be too complex for a screw to be placed safely.18,19
Frameless Stereotaxy for Intraoperative Navigation During Spinal Tumor Resection
 Pedicle Screw Fixation
Pedicle Screw Fixation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






