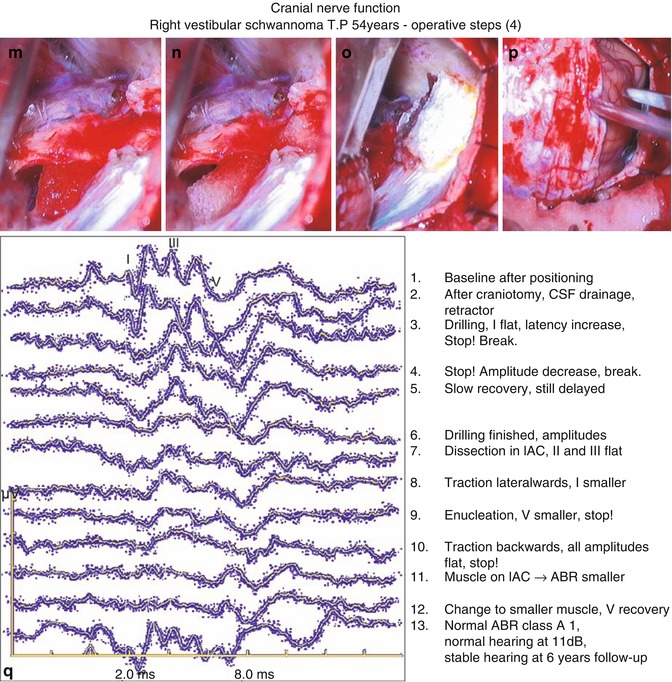
Fig. 24.1
(a) Right vestibular schwannoma exposed via the lateral suboccipital approach. (b) The dura of the petrous bone is resected. (c) The posterior wall of the internal auditory canal (IAC) is opened with the aid of a diamond drill. (d) The content of the IAC is exposed. (e) The intrameatal tumour part is mobilised out of the fundus. (f) The intrameatal tumour is enucleated and removed stepwise up to the porus. (g) The tumour is lifted and pulled upwards to expose the arachnoid at the border between tumour and cochlear nerve (arrow). (h) The tumour is pulled down and backwards, and a hint of the facial nerve appears at the upper border (arrow). (i) The tumour is pulled lateral for further enucleation and decompression of the brainstem. (j) The tumour capsule is lifted up exposing the caudal cranial nerves and cochlear nerve. (k) The tumour is pulled upwards and the cochlear nerve can be loosened in the arachnoid layer. (l) Most of the cochlear nerve is prepared free from the tumour and a part of the facial nerve becomes visible. (m) The tumour is completely removed with preservation of the facial and cochlear nerves. A moist fibrin sponge is positioned under the nerve bundle. (n) The exposed nerves are covered by a moist piece of fibrin sponge at the intrameatal portion. The petrous vein is observed under jugular venous compression. (o) The IAC is closed by layers of dura, muscle and fibrin plaster. (p) The cerebellum and dura are in an optimal state. (q) Intraoperative auditory brainstem response (ABR) monitoring with functional preservation of the cochlear (VIIIth) nerve. CSF cerebrospinal fluid
The subsequent microsurgical steps are to be undertaken and closely correlated with changes of EMG and ABR:
Baseline (after patient positioning)
Second baseline after craniotomy/craniectomy
Cerebrospinal fluid release
Retraction of the cerebellum
Arachnoid dissectivon and exposure of nerves and tumour
Bone removal of posterior wall of the internal auditory canal (conservation of labyrinthine structures)
Intrameatal tumour dissection
Tumour mobilization at the fundus of the IAC
Volume reduction (by 50 %) of space-occupying lesion in CPA
Stretching of tumour nerve bundle
Direct dissection at the tumour nerve plane
Complete resection of space-occupying lesion
Measures for haemostasis
Sealing of the internal auditory canal
Retractor removal
Dural closure
24.3.1.9 Microscopic Approach
The dura is opened in a laterally convex mode within the sinus angle and pulled outwards by two to three sutures. The cerebellum is lifted up with a retractor blade and the arachnoid over the caudal cranial nerves and the cisterna magna is opened for release of cerebrospinal fluid. Only if evoked potentials are stable, a definite retractor blade is positioned; otherwise, retraction must be loosened, until EP recovery occurs. In large tumours, considerable deterioration is observed already at this early step. Tension exerted by retraction is minimized by dissection of any arachnoid cover (Fig. 24.1a, b).
In tumour extension classes 1, 2 and 3, the next step is the opening of the internal auditory canal. In extension class 4 and in all other cases with critical EP, some tumour enucleation is performed first in order to reduce nerve traction.
For opening of the IAC, the vascularization of the dura of the petrous bone is coagulated (Fig. 24.1c) and the dura is excised (Fig. 24.1d) and is kept in moist tissues for re-use during closure later on.
The posterior wall of the IAC is opened with diamond drills. Respecting the labyrinthine system is facilitated, if the posterior wall of the IAC is preserved for at least 3.5 mm; the latter may be measured easily with the aid of an angulated hook [11]. During drilling repeated breaks are necessary, as no reliable ABR responses can be obtained simultaneous to any drilling. In addition to ABR, ECoch shall be observed providing fast information on any deterioration of inner ear function. Opening or destruction of the labyrinthine system is indicated by a steep amplitude loss of wave I or of the electrocochleographic potential. This will be followed by a general decline of all ABR components. If a considerable decline of wave I and of ECoch is observed, a fenestration of the bone layer of a semicircular canal must be presumed. Immediate sealing of the semicircular canal with microsurgical fibrin plaster can be tried. In case of hearing preservation, there is a significant drop of quality of hearing to be expected.
24.3.1.10 Intrameatal Dissection
After IAC opening intrameatal tumour reduction and nerve mobilization at the lateral end in the fundus are the next and risky steps. The identification of the facial nerve at the upper anterior part of the IAC is performed by slight mobilization of the upper tumour part. The tumour movement causes some facial nerve activation in EMG recordings. At the dorsal surface the superior and inferior vestibular nerves are identified and inspected for tumour infiltration; in most cases both nerves are tumourous and are transsected; then the intrameatal tumour portion is reduced in size by stepwise enucleation. Hereafter, the lateral tumour end may be luxated out of the fundus. During these steps special attention must be paid to ABR components I and II. If the ABR amplitude decreases repeatedly by 50 %, even with intermittent recovery, this is regarded as critical and some longer period for recovery to the original state is indicated. If this does not develop, the implantation of a small fibrin sponge soaked with nimodipine or papaverine solution under or on the nerve bundle may be helpful.
If recovery of the cochlear and nerve potentials I and II remains scarce, a change to a different site of action may be wise.
24.3.1.11 Tumour Dissection in the CPA Cistern
The tumour portion in the CPA is enucleated by use of the CUSA, platelet-shaped knife and micro-forceps as far as possible in order to reduce the compression to the brainstem and the tension on the nerves. The inner tumour parts are dissected, while the tumour capsule is maintained as long as possible. During the period of reduction, intermittent ABR deterioration may occur, especially if the tumour sinks down onto the eighth nerve. The facial and trigeminal nerves might show intermittent activity; as long as this comes up only on surgical activity, this is acceptable. If, however, post-manipulation activity occurs, then the traction on the nerves must be reduced, and irrigation with Ringer solution and some vasodilating (nimodipine, papaverine) solution is indicated.
24.3.1.12 Tumour Dissection at Tumour Nerve Border
After extensive debulking of the tumour, its capsule is gripped and lifted upwards. This may cause EMG responses and usually rather an improved ABR. Then the arachnoid layer is taken by a very fine forceps and pulled away from the tumour towards the course of the nerves. In large tumours the caudal cranial nerves are released from the tumour first; then the eighth nerve is to be loosened along its course from the brainstem to the porus. If the connection with the tumour is still too tight and ABR responses become critical, then there are three possibilities to safe nerve handling: first, the inferior tumour part needs further enucleation; second, sharp dissection is performed leaving some tumour remnants along the course of the nerve; or third, dissection of this site is left for later.
The next working direction is the dissection at the border between the brainstem and tumour towards the origin of the facial and trigeminal nerves. The tumour traction is now in lateral and slightly upward direction where the facial nerve will become visible at its brainstem origin. For easier identification direct electric stimulation at 0.5 mA is performed with a bipolar micro-forceps. Then the same mode of microsurgical action with soft short movements is performed for dissection of the arachnoid layer towards the nerve. If this leads again to serious traction and electrophysiological deterioration, then further tumour enucleation is necessary.
Thereafter, the tumour may be pulled backwards and downwards to expose the superior and anterior part of the tumour where the facial nerve is usually adherent and spread apart in diverted fascicle groups. Dissection of its arachnoid, lifting the nerve slowly away from the tumour, provokes EMG responses and allows the identification of the whole nerve up to the porus. While this is the moment of facial nerve identification and conservation, these actions may be most dangerous to the cochlear nerve.
Traction downwards and backwards is critical to the cochlear nerve and leads to deterioration of ABR components III to V. This may be counteracted by repeated breaks during which the tumour is lifted up to reduce the tension on the eighth nerve temporarily.
Both the nerves, cochlear and facial nerves, are most adherent to the tumour medial to the porus of the internal auditory canal. Dissection at this site is usually not possible in a soft mode, but sharp dissection may be necessary. Beforehand, it is essential to identify and secure both nerves at either side of this difficult region. After maximal tumour removal within the cistern, the internal auditory canal is approached again to remove final intrameatal tumour parts and to identify the facial and cochlear nerve courses. The tumour remnant is then lifted up and dissected off the cochlear nerve. Thereafter, the tumour remnant at the facial nerve is removed stepwise with intermittent use of electric stimulation to differentiate between facial nerve fascicle groups and tumourous parts until complete tumour resection. Direct nerve stimulation at the brainstem origin and within the IAC is performed and responses are compared to each other.
The nerves in the IAC are being covered by a moist fibrin sponge.
After control of all electrophysiological parameters, careful inspection of the operating field is performed and then repeated under jugular venous compression; hereby, inapparent opening of cerebellar and tentorial veins is identified and will be sealed by bipolar coagulation or by fibrin plaster (Fig. 24.1).
24.3.1.13 Closure
The internal auditory canal is reconstructed in part by implantation of the dural piece previously taken from the petrous bone. A sealing of any mastoid cells of that area is accomplished by implantation of a piece of muscle combined with fascia taken during the surgical approach; fixation is done with some fibrin glue or plaster. During muscle placement ABR responses must be controlled carefully, as compression by the muscle may lead to deterioration of auditory potentials (Fig. 24.1). If deterioration of wave III or waves I to III occurs, immediate removal of the muscle must be performed; after wave recovery, reimplantation may be tried, possibly with a smaller piece of muscle.
Finally, the tumour capsule may be set under traction away from the nerves, and the tumour is dissected off the nerves within the arachnoid plane by traction or by sharp dissection.
Closure of the approach consists of dural closure in a watertight mode, covering the dura by a layer of muscle fascia and covering the external mastoid cells by muscle fascia. The bone flap is fixed or substituted by methyl methacrylate.
24.3.2 Special Aspects for Selected Cases
Some patients pose a more advanced challenge to the neurosurgical team due to individual conditions such as the following ones:
Very large schwannoma
Schwannoma recurrence with some facial palsy
Schwannoma with only hearing ear and bad conventional ABR
24.3.2.1 Special Considerations on the Facial Nerve and Multimodality Control in Large Schwannomas
In large schwannomas the conventional free-run EMG for motor cranial nerve control is of limited use. For a long period of surgery, the facial and other nerves are not visible and cannot be tested by direct stimulation. While debulking the tumour, the surgeon does not know whether the motor nerves are still in continuity. If a part of a motor nerve is finally exposed, this may still be at a rather distal portion of the nerve course. Furthermore, only parts of the nerve may be identified and amenable to stimulation and testing. Motor evoked potentials can be of great help for these conditions. By contralateral anodal activation of the motor pathway and by transcranial electric multipulse stimulation technique, a reproducible activation of the motor cranial nuclei and nerves is initiated and motor evoked electromyographic responses can be recorded. MEP can be performed throughout surgery and long before direct nerve exposure. Due to artefact contamination performance and analysis are by no means simple (Fig. 24.2a, b). The usefulness of MEP is based on three aspects: (1) MEP are performed independent of nerve exposure, (2) MEP indicate a pre-existing lesion and (3) MEP are a helpful tool for prognostic measures.
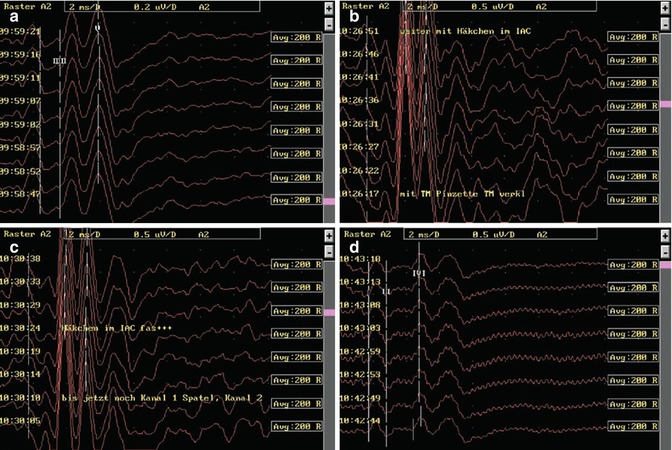
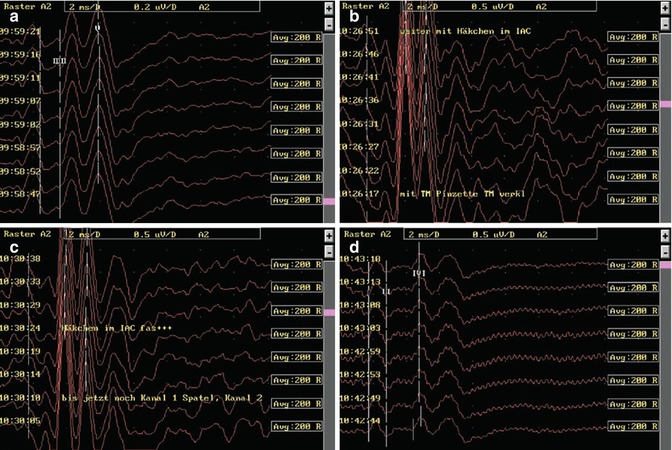
Fig. 24.2
(a) Conventional ABR. (b) Nearfield ABR: tumour enucleation. (c) Nearfield ABR: intrameatal dissection. (d) Preserved conventional ABR
Figure 24.2c demonstrates intraoperative facial MEP registration in a patient with a long-standing facial paresis. Due to the paresis the MEP latency is severely increased from an average of 14–18 ms; furthermore, during surgery a great variability in latency and amplitude is to be observed; preservation of the MEP up to the end of surgery correlated well with preserved facial function at House-Brackmann Grade 4 and subsequent recovery to Grade 3 within 6 weeks.
Regarding motor cranial nerve electromyography, all actions with some traction should cause some EMG activity. If this is diminished or absent and if the course of the facial nerve is difficult to identify, then electric stimulation is useful in order to differentiate tumour nerve fibres and different motor nerves (Fig. 24.3). Stimulation should be kept at a limited intensity of 0.5–1 mA and rather at low stimulation frequency in order to prevent any nerve block.
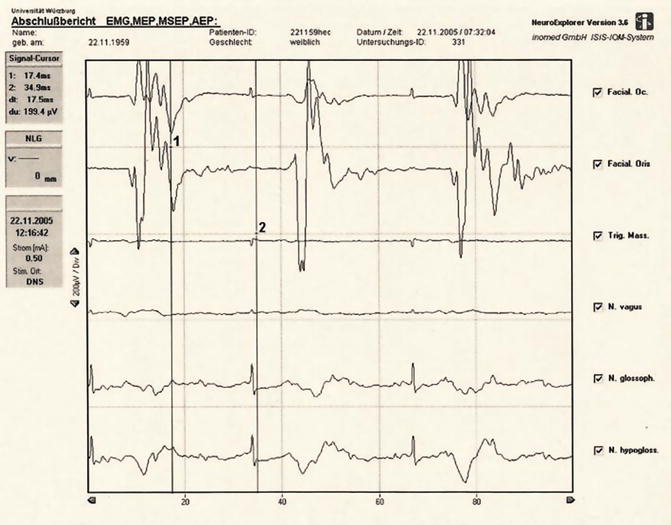
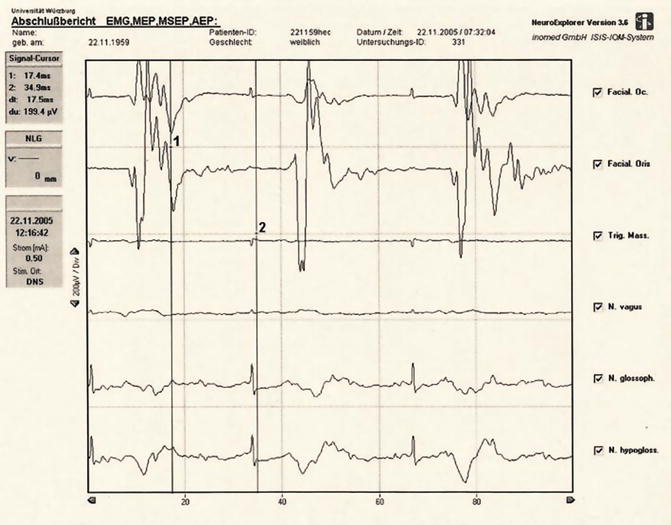
Fig. 24.3
Electromyography motor cranial nerves in the cerebellopontine angle (CPA): muscle action potentials evoked by direct nerve stimulation at 0.5 mA. A stimulus artefact is visible in all recordings. EMG Electromyography, MEP motor evoked potential, MSEP median nerve somatosensory evoked potential, AEP auditory evoked potential
24.3.2.2 Special Considerations on the Auditory Pathway and Multimodality Control in Critical Hearing Function
In some patients, despite normal to good hearing, conventional ABR may be severely deformed or not routinely reproducible. However, preservation of auditory function may be essential for their further life course, as in the case of the last hearing ear or in professionals with a special need of bilateral hearing. Then advanced techniques of functional microsurgery become necessary, namely, the support by near-field monitoring. By principle, in contrast to conventional far-field electrophysiological monitoring, near-field monitoring requires special electrode positioning as closely to the site of the potential generators as possible in order to register larger amplitude potentials and avoid the process of averaging potentials over 15 s or longer. Near-field recording offers the unique option of the so-called online information without delay of averaging and processing. Furthermore, thanks to the close position, potentials may be obtained in a certain number of patients where conventional recording fails and only by near-field technique some monitoring is enabled.
24.3.3 Electrocochleography
Electrocochleography may be performed by a transtympanal penetrating needle electrode or by a non-invasive tympanal surface electrode on the involved side.
Non-invasive technique of electrocochleography is carried out under visual control by otoscopy: a little ball electrode with some electrode contact jelly is placed on the tympanus. It is important to restrict the size of the electrode and the amount of surface jelly in order to contain the flexibility of the tympanus and to allow the simultaneous insertion of the earphone. By this near-field technique a cochlear microphonic and a large peak I are registered; in addition, due to the increasing distance of the generating anatomical structures, components II, III, IV and V of the ABR are also visible.
24.3.4 Brainstem Recording
A little ball electrode is placed at the lateral recess and covered with some cotton or one or two ball electrodes are mounted to the cerebellar retractor (Fig. 24.4). The latter technique may be performed in a bipolar fashion or with the Cz reference used generally for ABR. The same near-field electrode may be changed in position in order to be set closer to or directly on the auditory nerve during the microsurgical process. Recording produces a near-field ABR containing components III, IV and V. It may also show components I and II in an inverted mode.
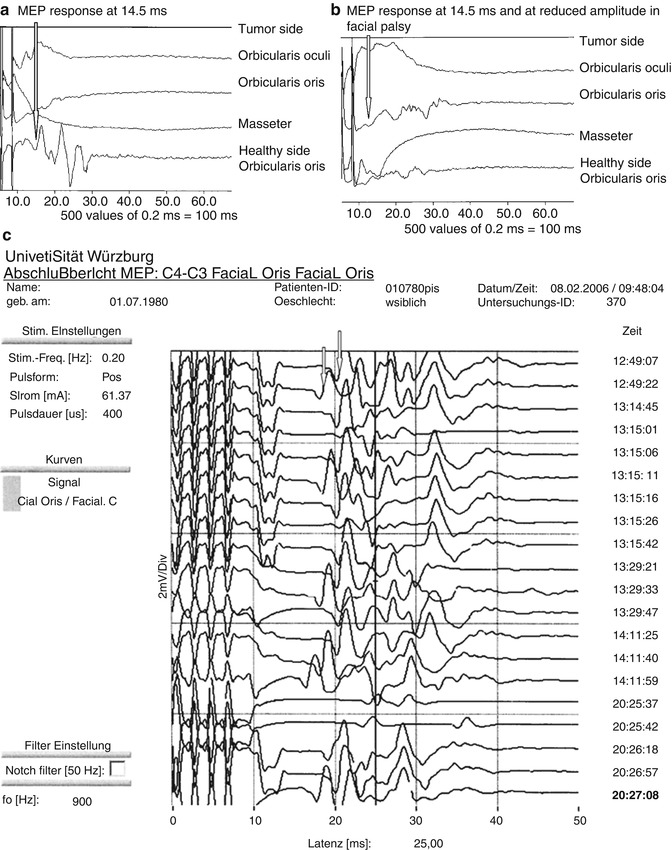
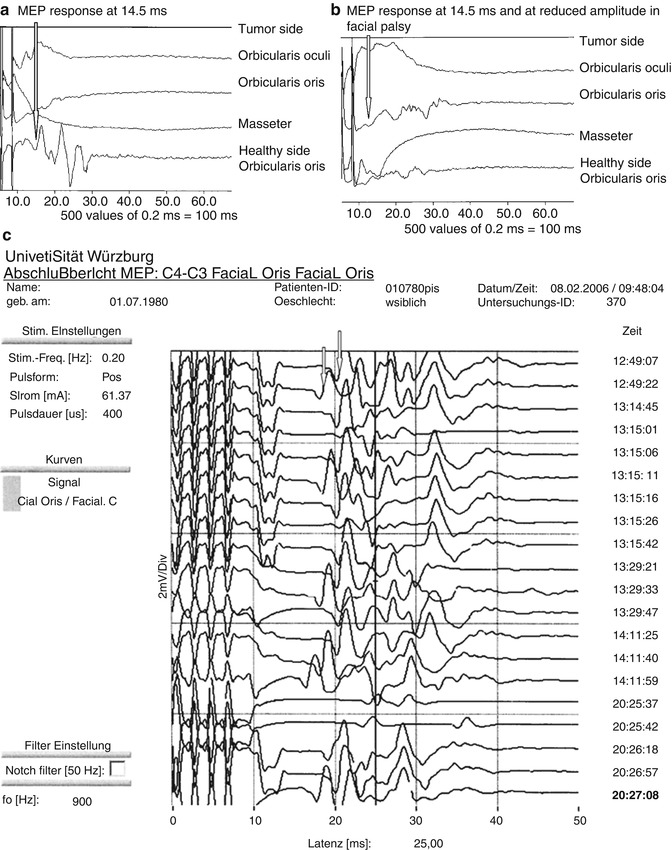
Fig. 24.4
(a) Stimulation M4/M3 on the healthy side: MEP response at 14.5 ms. (b) Stimulation M4/M3 on the tumour side: MEP response at 14.5 ms and at reduced amplitude in a case of facial palsy. (c) Stimulation M4/M3 on the tumour side: MEP response at 17.5 and 20 ms (white arrows) in a case of facial palsy
The obtained potentials are at minimum tenfold larger, and ten recordings form a well-discernible response within 2 s, but even if 60 averaged recordings are used, this process will take at a maximum of 5 s.
24.3.5 Principles of Neurophysiological Co-work
During microsurgery continuous exchange must take place between the neurosurgeon and the neurophysiologist. The neurophysiologist will report any deterioration with an atmosphere of reassurance as long as it is not critical. Once any deterioration proceeds towards a critical direction, he or she will indicate this in order to give the chance to the surgeon to prevent harmful changes by performing an early break in time. This might mean a true break with waiting for a recovery, some irrigation with Ringer solution or a vasoactive substance or the changing of the site of action to another less sensitive area for some time.
Vice versa, the experienced surgeon will predict and announce to the neurophysiologist those actions he or she is planning, and regarding as potentially critical for the monitoring.
Within an experienced team, the microsurgical process is therefore not slower, but in general rather faster than without monitoring, because those periods with stable recording are used in an optimal way by the surgeon – if he or she has gained some positive experience.
The criteria to follow during monitoring are multifold: by principle conservation of ABR waves I and V is the first line goal. In order to achieve those, all the changes occurring beforehand must be detected and counteracted, namely, critical changes of components II and III. Those components are endangered under special microsurgical conditions, at most on traction backwards and downwards. But also during dissection within the IAC or at the tumour nerve border, a special risk exists. Besides, the traction away from the brainstem and away from the cochlea is to be judged as critical and needs a close observation [12, 16].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








